Covid-19 Messenger Rna Vaccine
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Main Outcomes of Discussion of WHO Consultation on Nucleic Acid
MAIN OUTCOMES OF DISCUSSION FROM WHO CONSULTATION ON NUCLEIC ACID VACCINES I. Knezevic, R. Sheets 21-23 Feb, 2018 Geneva, Switzerland CONTEXT OF DISCUSSION • WHO Consultation held to determine whether the existing DNA guidelines were due for revision or if they remained relevant with today’s status of nucleic acid vaccine development and maturity towards licensure (marketing authorization) • Presentation will cover alignment to existing guidelines • Current status of development of DNA and RNA vaccines, both prophylactic & therapeutic • Main outcomes of discussion • Next steps already underway & planned STATUS OF DEVELOPMENT OF NUCLEIC ACID VACCINES • First likely candidate to licensure could be a therapeutic DNA vaccine against Human Papilloma Viruses • Anticipated to be submitted for licensure in 3-5 years • Other DNA vaccines are likely to follow shortly thereafter, e.g., Zika prophylaxis • RNA vaccines – less clinical experience, but therapeutic RNAs anticipated in 2021/22 timeframe to be submitted for licensure • For priority pathogens in context of public health emergencies, several candidates under development (e.g., MERS-CoV, Marburg, Ebola) MAIN OUTCOMES - GENERAL • Regulators expressed need for updated DNA guideline for prophylaxis and therapy • Less need at present for RNA vaccines in guideline but need some basic PTC • Flexibility needed now until more experience gained for RNA vaccines that will come in next few years • Revisit need for a more specific guideline at appropriate time for RNA vaccines • Institutional Biosafety Committees are regulated by national jurisdictions & vary considerably • How can WHO assist to streamline or converge these review processes? Particularly, during Public Health Emergency – can anything be done beforehand? MAIN OUTCOMES - DEFINITIONS • Clear Definitions are needed • Proposed definition of DNA vaccine: • A DNA plasmid(s) into which the desired immunogen(s) is (are) encoded and prepared as purified plasmid preparations to be administered in vivo. -

Review of COVID-19 Vaccine Subtypes, Efficacy and Geographical Distributions Andre Ian Francis ,1 Saudah Ghany,1 Tia Gilkes,1 Srikanth Umakanthan2
Review Postgrad Med J: first published as 10.1136/postgradmedj-2021-140654 on 6 August 2021. Downloaded from Review of COVID-19 vaccine subtypes, efficacy and geographical distributions Andre Ian Francis ,1 Saudah Ghany,1 Tia Gilkes,1 Srikanth Umakanthan2 1Department of Clinical Medical ABSTRACT 2021, the Ad26.COV2.S, developed by Janssen Sciences, The Faculty of Medical As of 1 May 2021, there have been 152 661 445 (Johnson & Johnson) and Moderna on 30 April.4 Sciences, The University of the COVAX, coordinated by WHO, Gavi: The West Indies, St. Augustine, Covid-19 cases with 3 202 256 deaths globally. Trinidad and Tobago This pandemic led to the race to discover a vaccine Vaccine Alliance, the Coalition for Epidemic 2Pathology unit, Department to achieve herd immunity and curtail the damaging Preparedness Innovations (CEPI), acts as a of Paraclinical Sciences, The effects of Covid-19. This study aims to discuss the most programme that supports the development of University Of The West Indies, St. COVID-19 vaccine candidates and negotiates their Augustine, Trinidad and Tobago recent WHO-approved Covid-19 vaccine subtypes, their status and geographical scheduled updates as of 4 pricing to ensure low- and- middle- income countries have a fair shot at receiving vaccines.5 Correspondence to May 2021. The keywords “Covid-19, Vaccines, Pfizer, Mr. Andre Ian Francis, The BNT162b2, AstraZeneca, AZD1222, Moderna, mRNA- This article aims at discussing the most recent University of the West Indies, St. 1273, Janssen, Ad26.COV2.S” were typed into PubMed. WHO- approved COVID-19 vaccine subtypes, their Augustine, Trinidad and Tobago; Thirty Two relevant PubMed articles were included in status and geographical scheduled updates as of 4 andre. -

Common COVID-19 Myths and Misinformation
Common COVID-19 Myths and Misinformation Myth: The side effects of Myth: The COVID-19 Myth: If I’ve already had the COVID-19 vaccine are vaccine can affect COVID-19, I don’t need a dangerous. women’s fertility. vaccine. Myth: Researchers rushed the development of the Myth: Getting the COVID- Myth: The COVID-19 COVID-19 vaccine, so its 19 vaccine gives you vaccine can affect effectiveness and safety COVID-19. women’s fertility. cannot be trusted. Myth: The COVID-19 vaccine enters your cells and changes your DNA. Information gathered from the following website: https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/covid-19-vaccines-myth-versus-fact https://www.muhealth.org/our-stories/covid-19-vaccine-myths-vs-facts FACT: People who have gotten sick with COVID-19 may still benefit from getting vaccinated. Due to the severe health risks associated with COVID-19 and the fact that re-infection with COVID-19 is possible, people may be advised to get a COVID-19 vaccine If I’ve already had even if they have been sick with COVID-19 before. There is not enough information currently available to COVID-19, I don’t say if or for how long people are protected from getting COVID-19 after they have had it (natural need a vaccine. immunity). Early evidence suggests natural immunity from COVID-19 may not last very long, but more studies are needed to better understand this. Several subjects in the Pfizer trial who were previously infected got vaccinated without ill effects. Some scientists believe the vaccine offers better protection for coronavirus than natural infection. -

V.5 3/18/2021 1 COVID-19 Vaccine FAQ Sheet
COVID-19 Vaccine FAQ Sheet (updated 3/18/2021) The AST has received queries from transplant professionals and the community regarding the COVID-19 vaccine. The following FAQ was developed to relay information on the current state of knowledge. This document is subject to change and will be updated frequently as new information or data becomes available. What kinds of vaccines are available or under development to prevent COVID-19? There are currently several vaccine candidates in use or under development. In the United States, the Government is supporting six separate vaccine candidates. Several other vaccines are also undergoing development outside of the United States government sponsorship and further information can be found here: NYTimes Coronavirus Vaccine Tracker: https://www.nytimes.com/interactive/2020/science/coronavirus-vaccine- tracker.html Washington Post Vaccine Tracker: https://www.washingtonpost.com/graphics/2020/health/covid-vaccine-update- coronavirus/ v.5 3/18/2021 1 The types of vaccines are as follows (March 1, 2021) 1: Table 1: Vaccines Under Development or Available Through EUA Vaccine Type Compound Name [Sponsor] Clinical Notes Trial Phase mRNA mRNA-1273 [Moderna] Phase 3 Emergency use in U.S., E.U., other countries Approved in Canada BNT162b2 (Comirnaty) [Pfizer] Phase 2/3 Emergency use in U.S., E.U., other countries Also approved in Canada and other countries Replication- AZD1222 (Covishield) Phase 2/3 Emergency use defective [AstraZeneca] in U.K., India, adenoviral other countries vector (not U.S.) JNJ-78326735/Ad26.COV2.S -
Update on Approved and Candidate COVID-19 Vaccines in the EU
Update on approved and candidate COVID-19 vaccines in the EU Dr. Marco Cavaleri Head of Biological Health Threats and Vaccines Strategy, EMA An agency of the European Union Outline 1 EMA response to COVID-19 pandemic - milestones 2 COVID-19 vaccines approved in the EU 3 Benefits and risks of COVID-19 vaccines 4 Real world evidence on effectiveness 5 Studies in children 6 Vaccines under review by EMA 7 Adapting COVID-19 vaccines to variants 8 Additional information Classified as public by the European Medicines Agency EMA RESPONSE TO COVID-19 PANDEMIC Milestones in the fight against the pandemic Scientific & regulatory Rapid development & Transparency & mobilisation evaluation outreach Approval: Comirnaty, COVID-19 vaccine Moderna, COVID-19 vaccine AstraZeneca, COVID-19 vaccine Janssen Accelerated development & evaluation procedures WHO declares pandemic COVID-19 Experts’ Task Force Jan Feb Mar Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar Apr May Jun Jul Aug Sep Oct Nov Dec 2020 2021 1 Classified as public by the European Medicines Agency COVID-19 vaccines approved in the EU 4 vaccines authorised in the EU • Comirnaty and Moderna vaccines contain a molecule called messenger RNA (mRNA) with instructions for producing the spike protein from SARS-CoV-2, the virus that causes COVID-19 • The AstraZeneca and Janssen vaccine uses a non-replicating adenovirus as a carrier that has been modified to produce the spike protein from SARS-CoV-2. • The vaccines do not contain the SARS-CoV-2 virus causing COVID-19 itself and cannot cause the disease. Comirnaty COVID-19 Vaccine COVID-19 Vaccine COVID-19 Vaccine (BioNTech/Pfizer) Moderna AstraZeneca Janssen 21 Dec 6 Jan 29 Jan 11 Mar 2 Classified as public by the European Medicines Agency BENEFITS AND RISKS Efficacy of COVID-19 vaccines in trials All COVID-19 vaccines approved in the EU have a positive benefit-risk balance in prevention of COVID-19 disease. -

An Update on Self-Amplifying Mrna Vaccine Development
Review An Update on Self-Amplifying mRNA Vaccine Development Anna K. Blakney 1,* , Shell Ip 2 and Andrew J. Geall 2 1 Michael Smith Laboratories, School of Biomedical Engineering, University of British Columbia, Vancouver, BC V6T 1Z4, Canada 2 Precision NanoSystems Inc., Vancouver, BC V6P 6T7, Canada; [email protected] (S.I.); [email protected] (A.J.G.) * Correspondence: [email protected] Abstract: This review will explore the four major pillars required for design and development of an saRNA vaccine: Antigen design, vector design, non-viral delivery systems, and manufacturing (both saRNA and lipid nanoparticles (LNP)). We report on the major innovations, preclinical and clinical data reported in the last five years and will discuss future prospects. Keywords: RNA; self-amplifying RNA; replicon; vaccine; drug delivery 1. Introduction: The Four Pillars of saRNA Vaccines In December 2019, the SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) virus emerged, causing a respiratory illness, coronavirus disease 2019 (COVID-19), in Hubei province, China [1,2]. The virus has spread globally, with the World Health Organization (WHO) declaring it a Public Health Emergency of International concern on 30 January 2020 and a pandemic officially on 7 March 2020 [3]. There is a strong consensus globally that a COVID-19 vaccine is likely the most effective approach to sustainably controlling the COVID-19 pandemic [4]. There has been an unprecedented research effort and global Citation: Blakney, A.K.; Ip, S.; Geall, coordination which has resulted in the rapid development of vaccine candidates and A.J. An Update on Self-Amplifying initiation of human clinical trials. -

1 Title: Interim Report of a Phase 2 Randomized Trial of a Plant
medRxiv preprint doi: https://doi.org/10.1101/2021.05.14.21257248; this version posted May 17, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. All rights reserved. No reuse allowed without permission. 1 Title: Interim Report of a Phase 2 Randomized Trial of a Plant-Produced Virus-Like Particle 2 Vaccine for Covid-19 in Healthy Adults Aged 18-64 and Older Adults Aged 65 and Older 3 Authors: Philipe Gobeil1, Stéphane Pillet1, Annie Séguin1, Iohann Boulay1, Asif Mahmood1, 4 Donald C Vinh 2, Nathalie Charland1, Philippe Boutet3, François Roman3, Robbert Van Der 5 Most4, Maria de los Angeles Ceregido Perez3, Brian J Ward1,2†, Nathalie Landry1† 6 Affiliations: 1 Medicago Inc., 1020 route de l’Église office 600, Québec, QC, Canada, G1V 7 3V9; 2 Research Institute of the McGill University Health Centre, 1001 Decarie St, Montreal, 8 QC H4A 3J1; 3 GlaxoSmithKline Biologicals SA (Vaccines), Avenue Fleming 20, 1300 Wavre, 9 Belgium; 4 GlaxoSmithKline Biologicals SA (Vaccines), rue de l’Institut 89, 1330 Rixensart, 10 Belgium; † These individuals are equally credited as senior authors. 11 * Corresponding author: Nathalie Landry, 1020 Route de l’Église, Bureau 600, Québec, Qc, 12 Canada, G1V 3V9; Tel. 418 658 9393; Fax. 418 658 6699; [email protected] 13 Abstract 14 The rapid spread of SARS-CoV-2 globally continues to impact humanity on a global scale with 15 rising morbidity and mortality. Despite the development of multiple effective vaccines, new 16 vaccines continue to be required to supply ongoing demand. -

Statements Contained in This Release As the Result of New Information Or Future Events Or Developments
Pfizer and BioNTech Provide Update on Booster Program in Light of the Delta-Variant NEW YORK and MAINZ, GERMANY, July 8, 2021 — As part of Pfizer’s and BioNTech’s continued efforts to stay ahead of the virus causing COVID-19 and circulating mutations, the companies are providing an update on their comprehensive booster strategy. Pfizer and BioNTech have seen encouraging data in the ongoing booster trial of a third dose of the current BNT162b2 vaccine. Initial data from the study demonstrate that a booster dose given 6 months after the second dose has a consistent tolerability profile while eliciting high neutralization titers against the wild type and the Beta variant, which are 5 to 10 times higher than after two primary doses. The companies expect to publish more definitive data soon as well as in a peer-reviewed journal and plan to submit the data to the FDA, EMA and other regulatory authorities in the coming weeks. In addition, data from a recent Nature paper demonstrate that immune sera obtained shortly after dose 2 of the primary two dose series of BNT162b2 have strong neutralization titers against the Delta variant (B.1.617.2 lineage) in laboratory tests. The companies anticipate that a third dose will boost those antibody titers even higher, similar to how the third dose performs for the Beta variant (B.1.351). Pfizer and BioNTech are conducting preclinical and clinical tests to confirm this hypothesis. While Pfizer and BioNTech believe a third dose of BNT162b2 has the potential to preserve the highest levels of protective efficacy against all currently known variants including Delta, the companies are remaining vigilant and are developing an updated version of the Pfizer-BioNTech COVID-19 vaccine that targets the full spike protein of the Delta variant. -

Revision Rápida
REVISION RÁPIDA EVALUACIÓN DE LAS CARACTERÍSTICAS DE ALMACENAMIENTO, TRANSPORTE Y DISTRIBUCIÓN DE LAS VACUNAS COVID-19 EN ESTUDIO, Y LAS CARACTERÍSTICAS CLÍNICAS DE LA POBLACIÓN CANDIDATA A VACUNACIÓN Noviembre de 2020 El Instituto de Evaluación Tecnológica en Salud – IETS, es una corporación sin ánimo de lucro, de participación mixta y de carácter privado, con patrimonio propio, creado según lo estipulado en la Ley 1438 de 2011. Su misión es contribuir al desarrollo de mejores políticas públicas y prácticas asistenciales en salud, mediante la producción de información basada en evidencia, a través de la evaluación de tecnologías en salud y guías de práctica clínica, con rigor técnico, independencia y participación. Sus miembros son el Ministerio de Salud y Protección Social – MinSalud, el Departamento Administrativo de Ciencia, Tecnología e Innovación – Colciencias, el Instituto Nacional de Vigilancia de Medicamentos y Alimentos – INVIMA, el Instituto Nacional de Salud – INS, la Asociación Colombiana de Facultades de Medicina – ASCOFAME y la Asociación Colombiana de Sociedades Científicas – ACSC. Autores Lucas López Quiceno. Médico y cirujano, Especialista en Epidemiología, Magister en Epidemiología, Magíster en economía de la salud (c). Instituto de Evaluación Tecnológica en Salud - IETS. Jhyld Carolaind Camacho Barbosa, Nutricionista y Dietista, Magister en Epidemiología. Instituto de Evaluación Tecnológica en Salud - IETS. Kelly Estrada-Orozco. Médica, Magister en Epidemiología Clínica, Magister en Neurociencia. Doctorado en Salud Pública (actual). Doctorado en Epidemiología Clínica (actual). Instituto de Evaluación Tecnológica en Salud - IETS. Revisores Cortes-Muñoz, Ani Julieth. Bacterióloga y laboratorista clínica. MSc. Epidemiología. Instituto de Evaluación Tecnológica en salud - IETS. Ospina-Lizarazo, Nathalie. Nutricionista Dietista. MSc. Epidemiología Clínica. Instituto de Evaluación Tecnológica en salud - IETS. -

Aptamer Applications in Emerging Viral Diseases
pharmaceuticals Review Aptamer Applications in Emerging Viral Diseases Arne Krüger 1,† , Ana Paula de Jesus Santos 2,†, Vanessa de Sá 2, Henning Ulrich 2,* and Carsten Wrenger 1,* 1 Department of Parasitology, Institute of Biomedical Sciences, University of São Paulo, São Paulo 05508-000-SP, Brazil; [email protected] 2 Department of Biochemistry, Institute of Chemistry, University of São Paulo, São Paulo 05508-900-SP, Brazil; [email protected] (A.P.d.J.S.); [email protected] (V.d.S.) * Correspondence: [email protected] (H.U.); [email protected] (C.W.) † These authors contributed equally to this work. Abstract: Aptamers are single-stranded DNA or RNA molecules which are submitted to a process denominated SELEX. SELEX uses reiterative screening of a random oligonucleotide library to identify high-affinity binders to a chosen target, which may be a peptide, protein, or entire cells or viral particles. Aptamers can rival antibodies in target recognition, and benefit from their non-proteic nature, ease of modification, increased stability, and pharmacokinetic properties. This turns them into ideal candidates for diagnostic as well as therapeutic applications. Here, we review the recent accomplishments in the development of aptamers targeting emerging viral diseases, with emphasis on recent findings of aptamers binding to coronaviruses. We focus on aptamer development for diagnosis, including biosensors, in addition to aptamer modifications for stabilization in body fluids and tissue penetration. Such aptamers are aimed at in vivo diagnosis and treatment, such as quantification of viral load and blocking host cell invasion, virus assembly, or replication, respectively. Although there are currently no in vivo applications of aptamers in combating viral diseases, such Citation: Krüger, A.; de Jesus Santos, strategies are promising for therapy development in the future. -
Candidate SARS-Cov-2 Vaccines in Advanced Clinical Trials: Key Aspects Compiled by John D
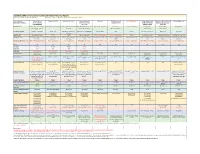
Candidate SARS-CoV-2 Vaccines in Advanced Clinical Trials: Key Aspects Compiled by John D. Grabenstein, RPh, PhD All dates are estimates. All Days are based on first vaccination at Day 0. Vaccine Sponsor Univ. of Oxford ModernaTX USA BioNTech with Pfizer Johnson & Johnson Novavax Sanofi Pasteur with CureVac with Bayer CanSino Biologics with Sinopharm (China National Sinovac Biotech Co. [with Major Partners] (Jenner Institute) (Janssen Vaccines & GlaxoSmithKline Academy of Military Biotec Group) (Beijing IBP, with AstraZeneca Prevention) Medical Sciences Wuhan IBP) Headquarters Oxford, England; Cambridge, Cambridge, Massachusetts Mainz, Germany; New York, New Brunswick, New Jersey Gaithersburg, Maryland Lyon, France; Tübingen, Germany Tianjin, China; Beijing, China; Beijing, China England, Gothenburg, New York (Leiden, Netherlands) Brentford, England Beijing, China Wuhan, China Sweden Product Designator ChAdOx1 or AZD1222 mRNA-1273 BNT162b2, tozinameran, Ad26.COV2.S, JNJ-78436735 NVX-CoV2373 TBA CVnCoV Ad5-nCoV, Convidecia BBIBP-CorV CoronaVac Comirnaty Vaccine Type Adenovirus 63 vector mRNA mRNA Adenovirus 26 vector Subunit (spike) protein Subunit (spike) protein mRNA Adenovirus 5 vector Inactivated whole virus Inactivated whole virus Product Features Chimpanzee adenovirus type Within lipid nanoparticle Within lipid nanoparticle Human adenovirus type 26 Adjuvanted with Matrix-M Adjuvanted with AS03 or Adjuvanted with AS03 Human adenovirus type 5 Adjuvanted with aluminum Adjuvanted with aluminum 63 vector dispersion dispersion vector AF03 -

Covid-19 Vaccine Myths
COVID-19 VACCINE MYTHS Family physicians want you to know what’s true. MYTH 1: You can delay routine vaccinations until the MYTH 5: The vaccine will alter my DNA. pandemic is over. This isn’t possible. mRNA vaccines work in the cell’s cytoplasm You shouldn’t postpone your vaccinations. Routine and never enter the cell nucleus, where the DNA, your genetic childhood and adult vaccinations are an important part of maintaining material, lives. It’s broken down quickly once it enters the cell and your health because they prevent other illnesses. Talk with your family delivers the needed vaccine “message” to the cell’s machinery. The physician about what vaccinations you still need and how to safely virus spike protein is also rapidly broken down once there is no longer catch up. They may have alternate times or locations to vaccinate any mRNA. The adenovirus platform uses DNA encoding the spike healthy patients, decreasing exposure to those who might be sick with protein which does enter the nucleus. However, it does not alter the COVID-19. cell’s DNA in any way. MYTH 2: The COVID-19 vaccines were developed MYTH 6: COVID-19 vaccines will deliver a microchip too fast to be safe. into my body. The technology used to develop the new mRNA There is not a microchip in the vaccines. This false rumor COVID-19 vaccines isn’t new. It’s been studied and used started after comments about digital vaccine records. State electronic for cancer research, and the original research on messenger RNA immunization records help patients and physicians track vaccines they (mRNA) vaccines is decades old.