Assessment of Efficacy of Bezlotoxumab for Prevention of Clostridium Difficile Infection Recurrence by Diagnostic Test Method
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Where Do Novel Drugs of 2016 Fit In?
FORMULARY JEOPARDY: WHERE DO NOVEL DRUGS OF 2016 FIT IN? Maabo Kludze, PharmD, MBA, CDE, BCPS, Associate Director Elizabeth A. Shlom, PharmD, BCPS, SVP & Director Clinical Pharmacy Program Acurity, Inc. Privileged and Confidential August 15, 2017 Privileged and Confidential Program Objectives By the end of the presentation, the pharmacist or pharmacy technician participant will be able to: ◆ Identify orphan drugs and first-in-class medications approved by the FDA in 2016. ◆ Describe the role of new agents approved for use in oncology patients. ◆ Identify and discuss the role of novel monoclonal antibodies. ◆ Discuss at least two new medications that address public health concerns. Neither Dr. Kludze nor Dr. Shlom have any conflicts of interest in regards to this presentation. Privileged and Confidential 2016 NDA Approvals (NMEs/BLAs) ◆ Nuplazid (primavanserin) P ◆ Adlyxin (lixisenatide) ◆ Ocaliva (obeticholic acid) P, O ◆ Anthim (obitoxaximab) O ◆ Rubraca (rucaparib camsylate) P, O ◆ Axumin (fluciclovive F18) P ◆ Spinraza (nusinersen sodium) P, O ◆ Briviact (brivaracetam) ◆ Taltz (ixekizumab) ◆ Cinqair (reslizumab) ◆ Tecentriq (atezolizumab) P ◆ Defitelio (defibrotide sodium) P, O ◆ Venclexta (venetoclax) P, O ◆ Epclusa (sofosburvir and velpatasvir) P ◆ Xiidra (lifitigrast) P ◆ Eucrisa (crisaborole) ◆ Zepatier (elbasvir and grazoprevir) P ◆ Exondys 51 (eteplirsen) P, O ◆ Zinbyrta (daclizumab) ◆ Lartruvo (olaratumab) P, O ◆ Zinplava (bezlotoxumab) P ◆ NETSTPOT (gallium Ga 68 dotatate) P, O O = Orphan; P = Priority Review; Red = BLA Privileged and Confidential History of FDA Approvals Privileged and Confidential Orphan Drugs ◆FDA Office of Orphan Products Development • Orphan Drug Act (1983) – drugs and biologics . “intended for safe and effective treatment, diagnosis or prevention of rare diseases/disorders that affect fewer than 200,000 people in the U.S. -

Bezlotoxumab (Zinplava®)
Zinplava Swiss Risk Management Plan Summary V1.5 Swiss Summary of the Risk Management Plan (RMP) for Zinplava® (Bezlotoxumab 1000mg) Concentrate for solution for infusion Version 1.5 (November 2016) The Risk Management Plan (RMP) is a comprehensive document submitted as part of the application dossier for market approval of a medicine. The RMP summary contains information on the medicine's safety profile and explains the measures that are taken in order to further investigate and follow the risks as well as to prevent or minimise them. The RMP summary of Zinplava® is a concise document and does not claim to be exhaustive. As the RMP is an international document, the summary might differ from the “Arzneimittelinformation / Information sur le médicament” approved and published in Switzerland, e.g. by mentioning risks occurring in populations or indications not included in the Swiss authorisation. Please note that the reference document which is valid and relevant for the effective and safe use of Zinplava® in Switzerland is the “Arzneimittelinformation / Information sur le médicament” (see www.swissmedicinfo.ch) approved and authorized by Swissmedic. MSD Merck Sharp & Dohme AG is fully responsible for the accuracy and correctness of the content of the published summary RMP of Zinplava®. Zinplava Swiss Risk Management Plan Summary V1.5 1 Elements for Summary Tables in the EPAR 1.1 Summary Table of Safety Concerns Table 1 Summary of Safety Concerns Important identified risks None Important potential risks Infusion-related Reactions Including -

Revenue Codes with Special Linkages
INDIANA HEALTH COVERAGE PROGRAMS PROVIDER CODE TABLES Revenue Codes with Special Procedure Code Linkages Note: Due to possible changes in Indiana Health Coverage Programs (IHCP) policy or national coding updates, inclusion of a code on the code tables does not necessarily indicate current coverage. See IHCP Banner Pages and Bulletins and the IHCP Fee Schedules for updates to coding, coverage, and benefit information. For information about using this code table, see the Claim Submission and Processing provider reference module. Table 1 – Procedure Codes Linked to Revenue Code 260 – IV Therapy – General Table 2 – Procedure Codes Linked to Revenue Code 274 – Prosthetic/Orthotic Devices Table 3 – Procedure Codes Linked to Revenue Code 636 – Drugs Requiring Detailed Coding Table 4 – Procedure Code Linked to Revenue Code 724 – Labor Room/Delivery – Birthing Center Table 5 – Procedure Codes Linked to Revenue Code 920 – Other Diagnostic Services – General Table 6 – Procedure Codes Linked to Revenue Code 929 – Other Diagnostic Services Table 7 – Procedure Codes Linked to Revenue Code 940 – Other Therapeutic Services – General Table 8 – Procedure Codes Linked to Revenue Codes for Managed Care Billing Only (Revenue Codes 912, 913, and 960) Published: September 16, 2021 1 Indiana Health Coverage Programs Revenue Codes with Special Procedure Code Linkages Table 1 – Procedure Codes Linked to Revenue Code 260 – IV Therapy – General Reviewed/Updated: June 8, 2021 Note: The procedure codes in this table may be billed with revenue code 260 to receive separate reimbursement when billed on the same date of service as a treatment room revenue code. Injection administration (including vaccine administration) is included in the reimbursement for treatment rooms. -

761046Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 761046Orig1s000 MICROBIOLOGY/VIROLOGY REVIEW(S) Division of Anti-Infective Products Clinical microbiology Review BLA761046 Bezlotoxumab BLA: 761046 Date Submitted: 11-22-15 Date Received by CDER: 11-23-15 Date Assigned: 12-1-15 Date Completed: 4-19-16 Reviewer: Kerian Grande Roche, Ph.D. APPLICANT: Merck Sharp and Dohme Corp., a subsidiary of Merck and Co., Inc. (Merck) DRUG PRODUCT NAMES: Proprietary: Bezlotoxumab Nonproprietary: CDB1, MK6072 Antibody Class: IgG1/kappa isotype subclass Molecular Weight: 148.2 kDa DRUG CATEGORY: Human monoclonal antibody to C. difficile Toxin B PROPOSED INDICATION: Prevention of Clostridium difficile infection (CDI) recurrence in patients 18 years or older receiving antibiotic therapy for CDI PROPOSED DOSAGE FORM, STRENGTH, ROUTE OF ADMINISTRATION AND DURATION OF TREATMENT: MK-6072 drug product is a sterile, aqueous solution. Vials contain a target deliverable dose of 40 mL of 25mg/mL MK-6072 for a total of 1000 mg per vial. MK-6072 drug product is diluted (b) (4) prior to administration. The recommended dose of bezlotoxumab is 10 mg/kg by intravenous infusion over 60 minutes in one dose. DISPENSED: Rx RELATED PRODUCTS: N/A REMARKS: This submission is for an original Biologics License Application (BLA) for bezlotoxumab injection for intravenous use. Bezlotoxumab (MK-6072) is a fully human monoclonal antibody (mAb) of the IgG1/kappa isotype subclass that binds to Clostridium difficile (C. difficile) toxin B. CONCLUSIONS AND RECOMMENDATIONS: From clinical microbiology perspective, this BLA submission is approvable pending an accepted version of the labeling. See FDA’s proposed version of the microbiology section of the labeling below (this may not be the final Agency label as discussions are still ongoing). -

Medicines/Pharmaceuticals of Animal Origin V3.0 November 2020
Medicines/pharmaceuticals of animal origin V3.0 November 2020 Medicines/pharmaceuticals of animal origin - This guideline provides information for all clinical staff within Hospital and Health Services (HHS) on best practice for avoidance of issues related to animal products. Medicines/pharmaceuticals of animal origin - V3.0 November 2020 Published by the State of Queensland (Queensland Health), November 2020 This document is licensed under a Creative Commons Attribution 3.0 Australia licence. To view a copy of this licence, visit creativecommons.org/licenses/by/3.0/au © State of Queensland (Queensland Health) 2020 You are free to copy, communicate and adapt the work, as long as you attribute the State of Queensland (Queensland Health). For more information contact: Medication Services Queensland, Queensland Health, GPO Box 48, Brisbane QLD 4001, email [email protected] An electronic version of this document is available at https://www.health.qld.gov.au/__data/assets/pdf_file/0024/147507/qh-gdl-954.pdf Disclaimer: The content presented in this publication is distributed by the Queensland Government as an information source only. The State of Queensland makes no statements, representations or warranties about the accuracy, completeness or reliability of any information contained in this publication. The State of Queensland disclaims all responsibility and all liability (including without limitation for liability in negligence) for all expenses, losses, damages and costs you might incur as a result of the information being inaccurate -
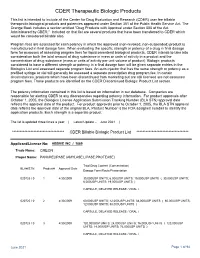
CDER Therapeutic Biologic Products List
CDER Therapeutic Biologic Products This list is intended to include all the Center for Drug Evaluation and Research (CDER) user fee billable therapeutic biological products and potencies approved under Section 351 of the Public Health Service Act. The Orange Book includes a section entitled "Drug Products with Approval under Section 505 of the Act Administered by CBER." Included on that list are several products that have been transferred to CDER which would be considered billable also. Program fees are assessed for each potency in which the approved (non-revoked, non-suspended) product is manufactured in final dosage form. When evaluating the specific strength or potency of a drug in final dosage form for purposes of assessing program fees for liquid parenteral biological products, CDER intends to take into consideration both the total amount of drug substance in mass or units of activity in a product and the concentration of drug substance (mass or units of activity per unit volume of product). Biologic products considered to have a different strength or potency in a final dosage form will be given separate entries in the Biologics List and assessed separate program fees. An auto-injector that has the same strength or potency as a prefilled syringe or vial will generally be assessed a separate prescription drug program fee. In certain circumstances, products which have been discontinued from marketing but are still licensed are not assessed program fees. Those products are identified on the CDER Discontinued Biologic Product List section. The potency information contained in this list is based on information in our database. -

ENTRY WATCH 2016 Published by the Patented Medicine Prices Review Board June 2018 Meds Entry Watch, 2016 Is Available in Electronic Format on the PMPRB Website
MEDS ENTRY WATCH 2016 Published by the Patented Medicine Prices Review Board June 2018 Meds Entry Watch, 2016 is available in electronic format on the PMPRB website. Une traduction de ce document est également disponible en français sous le titre : Veille des médicaments mis en marché, 2016 Patented Medicine Prices Review Board Standard Life Centre Box L40 333 Laurier Avenue West Suite 1400 Ottawa, ON K1P 1C1 Tel.: 1-877-861-2350 TTY 613-288-9654 Email: [email protected] Web: www.pmprb-cepmb.gc.ca ISSN 2560-6204 Cat. No.: H79-12E-PDF © Her Majesty the Queen in Right of Canada, as represented by the NPDUIS initiative of the Patented Medicine Prices Review Board, 2018 MEDS ENTRY WATCH 2016 About the PMPRB Acknowledgements The Patented Medicine Prices Review Board This report was prepared by the Patented (PMPRB) is a respected public agency that makes Medicine Prices Review Board (PMPRB) a unique and valued contribution to sustainable as part of the National Prescription Drug spending on pharmaceuticals in Canada by: Utilization Information System (NPDUIS). ~ providing stakeholders with price, cost and The PMPRB would like to acknowledge the utilization information to help them make timely contributions of and knowledgeable drug pricing, purchasing and ~ The members of the NPDUIS Advisory reimbursement decisions; and Committee for their expert oversight and ~ acting as an effective check on the patent rights guidance in the preparation of this report. of pharmaceutical manufacturers through the ~ PMPRB NPDUIS staff for their contribution responsible and efficient use of its consumer to the analytical content of the report: protection powers. -

FDA Briefing Document Bezlotoxumab Injection Meeting of the Antimicrobial Drugs Advisory Committee (AMDAC) June 9, 2016
FDA Briefing Document Bezlotoxumab Injection Meeting of the Antimicrobial Drugs Advisory Committee (AMDAC) June 9, 2016 The committee will discuss biologic license application (BLA) 761046 bezlotoxumab injection, submitted by Merck Sharpe & Dohme Corp., for the proposed indication of prevention of Clostridium difficile infection (CDI) recurrence. 1 The attached package contains background information prepared by the Food and Drug Administration (FDA) for the panel members of the advisory committee. The FDA background package often contains assessments and/or conclusions and recommendations written by individual FDA reviewers. Such conclusions and recommendations do not necessarily represent the final position of the individual reviewers, nor do they necessarily represent the final position of the Review Division or Office. We have brought bezlotoxumab injection to this Advisory Committee in order to gain the Committee’s insights and opinions, and the background package may not include all issues relevant to the final regulatory recommendation and instead is intended to focus on issues identified by the Agency for discussion by the Advisory Committee. The FDA will not issue a final determination on the issues at hand until input from the advisory committee process has been considered and all reviews have been finalized. The final determination may be affected by issues not discussed at the advisory committee meeting. 2 Table of Contents 1 Introduction ................................................................................................................ -

Drug Consumption at Wholesale Prices in 2017 - 2020
Page 1 Drug consumption at wholesale prices in 2017 - 2020 2020 2019 2018 2017 Wholesale Hospit. Wholesale Hospit. Wholesale Hospit. Wholesale Hospit. ATC code Subgroup or chemical substance price/1000 € % price/1000 € % price/1000 € % price/1000 € % A ALIMENTARY TRACT AND METABOLISM 321 590 7 309 580 7 300 278 7 295 060 8 A01 STOMATOLOGICAL PREPARATIONS 2 090 9 1 937 7 1 910 7 2 128 8 A01A STOMATOLOGICAL PREPARATIONS 2 090 9 1 937 7 1 910 7 2 128 8 A01AA Caries prophylactic agents 663 8 611 11 619 12 1 042 11 A01AA01 sodium fluoride 610 8 557 12 498 15 787 14 A01AA03 olaflur 53 1 54 1 50 1 48 1 A01AA51 sodium fluoride, combinations - - - - 71 1 206 1 A01AB Antiinfectives for local oral treatment 1 266 10 1 101 6 1 052 6 944 6 A01AB03 chlorhexidine 930 6 885 7 825 7 706 7 A01AB11 various 335 21 216 0 227 0 238 0 A01AB22 doxycycline - - 0 100 0 100 - - A01AC Corticosteroids for local oral treatment 113 1 153 1 135 1 143 1 A01AC01 triamcinolone 113 1 153 1 135 1 143 1 A01AD Other agents for local oral treatment 49 0 72 0 104 0 - - A01AD02 benzydamine 49 0 72 0 104 0 - - A02 DRUGS FOR ACID RELATED DISORDERS 30 885 4 32 677 4 35 102 5 37 644 7 A02A ANTACIDS 3 681 1 3 565 1 3 357 1 3 385 1 A02AA Magnesium compounds 141 22 151 22 172 22 155 19 A02AA04 magnesium hydroxide 141 22 151 22 172 22 155 19 A02AD Combinations and complexes of aluminium, 3 539 0 3 414 0 3 185 0 3 231 0 calcium and magnesium compounds A02AD01 ordinary salt combinations 3 539 0 3 414 0 3 185 0 3 231 0 A02B DRUGS FOR PEPTIC ULCER AND 27 205 5 29 112 4 31 746 5 34 258 8 -

A Abacavir Abacavirum Abakaviiri Abagovomab Abagovomabum
A abacavir abacavirum abakaviiri abagovomab abagovomabum abagovomabi abamectin abamectinum abamektiini abametapir abametapirum abametapiiri abanoquil abanoquilum abanokiili abaperidone abaperidonum abaperidoni abarelix abarelixum abareliksi abatacept abataceptum abatasepti abciximab abciximabum absiksimabi abecarnil abecarnilum abekarniili abediterol abediterolum abediteroli abetimus abetimusum abetimuusi abexinostat abexinostatum abeksinostaatti abicipar pegol abiciparum pegolum abisipaaripegoli abiraterone abirateronum abirateroni abitesartan abitesartanum abitesartaani ablukast ablukastum ablukasti abrilumab abrilumabum abrilumabi abrineurin abrineurinum abrineuriini abunidazol abunidazolum abunidatsoli acadesine acadesinum akadesiini acamprosate acamprosatum akamprosaatti acarbose acarbosum akarboosi acebrochol acebrocholum asebrokoli aceburic acid acidum aceburicum asebuurihappo acebutolol acebutololum asebutololi acecainide acecainidum asekainidi acecarbromal acecarbromalum asekarbromaali aceclidine aceclidinum aseklidiini aceclofenac aceclofenacum aseklofenaakki acedapsone acedapsonum asedapsoni acediasulfone sodium acediasulfonum natricum asediasulfoninatrium acefluranol acefluranolum asefluranoli acefurtiamine acefurtiaminum asefurtiamiini acefylline clofibrol acefyllinum clofibrolum asefylliiniklofibroli acefylline piperazine acefyllinum piperazinum asefylliinipiperatsiini aceglatone aceglatonum aseglatoni aceglutamide aceglutamidum aseglutamidi acemannan acemannanum asemannaani acemetacin acemetacinum asemetasiini aceneuramic -

Dostupnost Antiinfektiv V České Republice
aktuálně ročník 27 | číslo 5/2017 LÉKY A PRÁVO Dostupnost antiinfektiv v České republice MVDr. Veronika Valdová Arete‑Zoe, LLC Souhrn Valdová V. Dostupnost antiinfektiv v České republice. Remedia 2017; 27: 509–513. na Seznamu nepostradatelných léčiv Světové zdravotnické organizace figuruje 119 antiinfektiv, z nichž v České republice není registrováno 29. Dalších 10 léčiv je registrováno, ale neobchodováno. Dostupnost antibiotik a dalších nezbytných léčiv má přímý dopad na klinickou praxi. Příkladem je aktuali- zovaný postup pro léčbu sepse a septického šoku, který doporučuje deeskalaci a zacílení na identifikovaný patogen ihned po jeho identifikaci z důvodu snížení zátěže pro organismus pacienta. aktualizované léčebné postupy je nutno brát v úvahu při sestavování národních seznamů nepostradatelných léčiv. Z nepostradatelných tuberkulostatik a antivirotik chybějí v ČR některé fixní kombinace určené pro první linii léčby tuberkulózy a HIV/aIDS. Padělky léčivých přípravků a nedoléčené infekce jsou hlavními příčinami vzniku multirezistentních kmenů původce tuberkulózy. Z hyperimunních sér v ČR chybí sérum proti záškrtu. Vakcíny se potýkají s celosvětovým nedostatkem v důsledku délky a náročnosti výroby. Klíčová slova: antiinfektiva – nepostradatelná léčiva – dostupnost léčiv – nedostatek léčiv – tuberkulóza – HIV/aIDS – sepse. Summary Valdova V. Availability of antiinfectives in the Czech Republic. Remedia 2017; 27: 509–513. the World Health Organization (WHO) lists 119 antiinfectives on the list of essential medicines. Of these, 29 are not registered in the Czech Republic, and another 10 are registered but not marketed. availability of antimicrobials and other essential medicines directly affects clinical practice. One such example is the newly revised guidelines for the treatment of sepsis and septic shock, which recommends deescalation of antibiotic treatment and targeting the causative pathogen immediately after its identification to minimize toxicity to the patient’s metabolism. -

(12) Patent Application Publication (10) Pub. No.: US 2016/0184445 A1 Perroth Et Al
US 2016O184445A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2016/0184445 A1 Perroth et al. (43) Pub. Date: Jun. 30, 2016 (54) BUTYRYLCHOLINESTERASE Publication Classification ZWITTERONIC POLYMER CONUGATES (51) Int. Cl. (71) Applicant: Kodiak Sciences Inc., Palo Alto, CA A647/48 (2006.01) (US) CI2N 9/18 (2006.01) CI2N 9/96 (2006.01) (72) Inventors: D. Victor Perlroth, Palo Alto, CA (US); A638/46 (2006.01) Stephen A. Charles, Ravenna, OH (US); C07K 7/08 (2006.01) Wayne To, San Mateo, CA (US); (52) U.S. Cl. Xiaojian Huang, Mountain View, CA CPC ......... A61K 47/48 176 (2013.01); A61 K38/465 (US); Martin Linsell, San Mateo, CA (2013.01); C07K 7/08 (2013.01); C12N 9/96 (US); Didier Benoit, San Jose, CA (US) (2013.01); C12N 9/18 (2013.01); C07K 2319/30 (2013.01); C12Y-301/01008 (2013.01) (21) Appl. No.: 14/932,913 (22) Filed: Nov. 4, 2015 (57) ABSTRACT Related U.S. Application Data The present invention provides recombinant butyrylcho (63) Continuation of application No. PCT/US2015/ linesterase fusion proteins, including Fc fusion proteins and 0561 12, filed on Oct. 16, 2015. multi-armed high MW polymers containing hydrophilic (60) Provisional application No. 62/065,471, filed on Oct. groups conjugated to the fusion proteins, and methods of 17, 2014. preparing Such polymers. Patent Application Publication Jun. 30, 2016 Sheet 1 of 5 US 2016/O1844.45 A1 900 800 700 600 500 400 300 200 100 -5 5 15 25 35 TIME (DAYS) FIG. 1 Patent Application Publication Jun.