Nanoparticle-Based Delivery Platforms for Mrna Vaccine Development
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Rnase a Cleanup of DNA Samples Version Number: 1.0 Version 1.0 Date: 12/21/2016 Author(S): Yuko Yoshinaga, Eileen Dalin Reviewed/Revised By
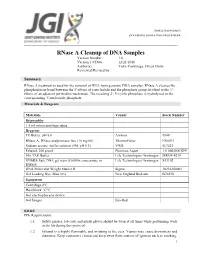
SAMPLE MANAGEMENT STANDARD OPERATING PROCEDURE RNase A Cleanup of DNA Samples Version Number: 1.0 Version 1.0 Date: 12/21/2016 Author(s): Yuko Yoshinaga, Eileen Dalin Reviewed/Revised by: Summary RNase A treatment is used for the removal of RNA from genomic DNA samples. RNase A cleaves the phosphodiester bond between the 5'-ribose of a nucleotide and the phosphate group attached to the 3'- ribose of an adjacent pyrimidine nucleotide. The resulting 2', 3'-cyclic phosphate is hydrolyzed to the corresponding 3'-nucleoside phosphate. Materials & Reagents Materials Vendor Stock Number Disposables 1.5 ml microcentrifuge tubes Reagents TE Buffer, pH 8.0 Ambion 9849 RNase A, DNase and protease-free (10 mg/ml) ThermoFisher EN0531 Sodium acetate buffer solution (3M, pH 5.2) VWR 567422 Ethanol, 200 proof Pharmco-Aaper 111000200CSPP 50x TAE Buffer Life Technologies/ Invitrogen MRGF-4210 SYBR® Safe DNA gel stain (10,000x concentrate in Life Technologies/ Invitrogen S33102 DMSO) DNA Molecular Weight Marker II Sigma 10236250001 Gel Loading Dye, Blue (6x) New England BioLabs B7021S Equipment Centrifuge 4°C Heat block 37°C Gel electrophoresis device Gel Imager Bio-Rad EH&S PPE Requirements: 1.1 Safety glasses, lab coat, and nitrile gloves should be worn at all times while performing work in the lab during this protocol. 1.2 Ethanol is a highly flammable and irritating to the eyes. Vapors may cause drowsiness and dizziness. Keep containers closed and keep away from sources of ignition such as smoking. 1 SAMPLE MANAGEMENT STANDARD OPERATING PROCEDURE Avoid contact with skin and eyes. In case of contact with eyes, rinse immediately with plenty of water and seek medical advice. -

Secretariat of the CBD Technical Series No. 82 Convention on Biological Diversity
Secretariat of the CBD Technical Series No. 82 Convention on Biological Diversity 82 SYNTHETIC BIOLOGY FOREWORD To be added by SCBD at a later stage. 1 BACKGROUND 2 In decision X/13, the Conference of the Parties invited Parties, other Governments and relevant 3 organizations to submit information on, inter alia, synthetic biology for consideration by the Subsidiary 4 Body on Scientific, Technical and Technological Advice (SBSTTA), in accordance with the procedures 5 outlined in decision IX/29, while applying the precautionary approach to the field release of synthetic 6 life, cell or genome into the environment. 7 Following the consideration of information on synthetic biology during the sixteenth meeting of the 8 SBSTTA, the Conference of the Parties, in decision XI/11, noting the need to consider the potential 9 positive and negative impacts of components, organisms and products resulting from synthetic biology 10 techniques on the conservation and sustainable use of biodiversity, requested the Executive Secretary 11 to invite the submission of additional relevant information on this matter in a compiled and synthesised 12 manner. The Secretariat was also requested to consider possible gaps and overlaps with the applicable 13 provisions of the Convention, its Protocols and other relevant agreements. A synthesis of this 14 information was thus prepared, peer-reviewed and subsequently considered by the eighteenth meeting 15 of the SBSTTA. The documents were then further revised on the basis of comments from the SBSTTA 16 and peer review process, and submitted for consideration by the twelfth meeting of the Conference of 17 the Parties to the Convention on Biological Diversity. -

U6 Small Nuclear RNA Is Transcribed by RNA Polymerase III (Cloned Human U6 Gene/"TATA Box"/Intragenic Promoter/A-Amanitin/La Antigen) GARY R
Proc. Nati. Acad. Sci. USA Vol. 83, pp. 8575-8579, November 1986 Biochemistry U6 small nuclear RNA is transcribed by RNA polymerase III (cloned human U6 gene/"TATA box"/intragenic promoter/a-amanitin/La antigen) GARY R. KUNKEL*, ROBIN L. MASERt, JAMES P. CALVETt, AND THORU PEDERSON* *Cell Biology Group, Worcester Foundation for Experimental Biology, Shrewsbury, MA 01545; and tDepartment of Biochemistry, University of Kansas Medical Center, Kansas City, KS 66103 Communicated by Aaron J. Shatkin, August 7, 1986 ABSTRACT A DNA fragment homologous to U6 small 4A (20) was screened with a '251-labeled U6 RNA probe (21, nuclear RNA was isolated from a human genomic library and 22) using a modified in situ plaque hybridization protocol sequenced. The immediate 5'-flanking region of the U6 DNA (23). One of several positive clones was plaque-purified and clone had significant homology with a potential mouse U6 gene, subsequently shown by restriction mapping to contain a including a "TATA box" at a position 26-29 nucleotides 12-kilobase-pair (kbp) insert. A 3.7-kbp EcoRI fragment upstream from the transcription start site. Although this containing U6-hybridizing sequences was subcloned into sequence element is characteristic of RNA polymerase II pBR322 for further restriction mapping. An 800-base-pair promoters, the U6 gene also contained a polymerase III "box (bp) DNA fragment containing U6 homologous sequences A" intragenic control region and a typical run of five thymines was excised using Ava I and inserted into the Sma I site of at the 3' terminus (noncoding strand). The human U6 DNA M13mp8 replicative form DNA (M13/U6) (24). -

Expanding the Genetic Code Lei Wang and Peter G
Reviews P. G. Schultz and L. Wang Protein Science Expanding the Genetic Code Lei Wang and Peter G. Schultz* Keywords: amino acids · genetic code · protein chemistry Angewandte Chemie 34 2005 Wiley-VCH Verlag GmbH & Co. KGaA, Weinheim DOI: 10.1002/anie.200460627 Angew. Chem. Int. Ed. 2005, 44,34–66 Angewandte Protein Science Chemie Although chemists can synthesize virtually any small organic molecule, our From the Contents ability to rationally manipulate the structures of proteins is quite limited, despite their involvement in virtually every life process. For most proteins, 1. Introduction 35 modifications are largely restricted to substitutions among the common 20 2. Chemical Approaches 35 amino acids. Herein we describe recent advances that make it possible to add new building blocks to the genetic codes of both prokaryotic and 3. In Vitro Biosynthetic eukaryotic organisms. Over 30 novel amino acids have been genetically Approaches to Protein encoded in response to unique triplet and quadruplet codons including Mutagenesis 39 fluorescent, photoreactive, and redox-active amino acids, glycosylated 4. In Vivo Protein amino acids, and amino acids with keto, azido, acetylenic, and heavy-atom- Mutagenesis 43 containing side chains. By removing the limitations imposed by the existing 20 amino acid code, it should be possible to generate proteins and perhaps 5. An Expanded Code 46 entire organisms with new or enhanced properties. 6. Outlook 61 1. Introduction The genetic codes of all known organisms specify the same functional roles to amino acid residues in proteins. Selectivity 20 amino acid building blocks. These building blocks contain a depends on the number and reactivity (dependent on both limited number of functional groups including carboxylic steric and electronic factors) of a particular amino acid side acids and amides, a thiol and thiol ether, alcohols, basic chain. -

"Modified" RNA (And DNA) World
July editorial The "modified" RNA (and DNA) world A few months ago, as COVID-19 vaccinations were getting underway in the U.S., a non-scientist friend said he was uneasy because had heard that the RNA in them had been "doped". Leaning in, I asked "How?" (I knew of course, vide infra). "With some chemical" he replied. This struck me as a perfect storm of an educated, reasonably informed non- scientist being led astray by how the media often doesn't get it quite right, though we all recognize that too much detail can be narcoleptic. The art is to convey the science in just the right dose, as Lewis Thomas and Carl Sagan did for example (1). I told my friend what the "doping" was, using lay terms. He listened thoughtfully and then I came in with my final shot: nature is full of RNA that is "doped", and even DNA is as well. These chemical modifications are not done by mad scientists but the very biological systems in which these RNAs and DNAs reside, using their own enzymes. He left somewhat convinced and hopefully is now vaccinated. This encounter gave me the thought that I, and my readers, should take a step back and think about all the "modified" RNAs and DNAs out there. For transfer RNAs alone, there are 120 known base modifications, with their prevalence as high as 13 of the 76 nucleotides in human cytosolic tRNAtyr(2). N6- adenosine methylation of messenger RNA, discovered in 1974, has recently come to the fore, although not all experts agree on its functional significance (3,4). -

Chapter 3. the Beginnings of Genomic Biology – Molecular
Chapter 3. The Beginnings of Genomic Biology – Molecular Genetics Contents 3. The beginnings of Genomic Biology – molecular genetics 3.1. DNA is the Genetic Material 3.6.5. Translation initiation, elongation, and termnation 3.2. Watson & Crick – The structure of DNA 3.6.6. Protein Sorting in Eukaryotes 3.3. Chromosome structure 3.7. Regulation of Eukaryotic Gene Expression 3.3.1. Prokaryotic chromosome structure 3.7.1. Transcriptional Control 3.3.2. Eukaryotic chromosome structure 3.7.2. Pre-mRNA Processing Control 3.3.3. Heterochromatin & Euchromatin 3.4. DNA Replication 3.7.3. mRNA Transport from the Nucleus 3.4.1. DNA replication is semiconservative 3.7.4. Translational Control 3.4.2. DNA polymerases 3.7.5. Protein Processing Control 3.4.3. Initiation of replication 3.7.6. Degradation of mRNA Control 3.4.4. DNA replication is semidiscontinuous 3.7.7. Protein Degradation Control 3.4.5. DNA replication in Eukaryotes. 3.8. Signaling and Signal Transduction 3.4.6. Replicating ends of chromosomes 3.8.1. Types of Cellular Signals 3.5. Transcription 3.8.2. Signal Recognition – Sensing the Environment 3.5.1. Cellular RNAs are transcribed from DNA 3.8.3. Signal transduction – Responding to the Environment 3.5.2. RNA polymerases catalyze transcription 3.5.3. Transcription in Prokaryotes 3.5.4. Transcription in Prokaryotes - Polycistronic mRNAs are produced from operons 3.5.5. Beyond Operons – Modification of expression in Prokaryotes 3.5.6. Transcriptions in Eukaryotes 3.5.7. Processing primary transcripts into mature mRNA 3.6. Translation 3.6.1. -

Evaluation of the Quality, Safety and Efficacy of Messenger RNA
1 2 3 WHO/BS/2021.2402 4 ENGLISH ONLY 5 6 7 8 9 Evaluation of the quality, safety and efficacy of messenger RNA vaccines for 10 the prevention of infectious diseases: regulatory considerations 11 12 13 14 15 16 NOTE: 17 18 This draft document has been prepared for the purpose of inviting comments and suggestions on 19 the proposals contained therein which will then be considered by the WHO Expert Committee on 20 Biological Standardization (ECBS). The distribution of this draft document is intended to 21 provide information on the proposed document: Evaluation of the quality, safety and efficacy of 22 messenger RNA vaccines for the prevention of infectious diseases: regulatory considerations to a 23 broad audience and to ensure the transparency of the consultation process. 24 25 The text in its present form does not necessarily represent the agreed formulation of the 26 ECBS. Written comments proposing modifications to this text MUST be received by 17 27 September 2021 using the Comment Form available separately and should be addressed to 28 the Department of Health Products Policy and Standards, World Health Organization, 20 Avenue 29 Appia, 1211 Geneva 27, Switzerland. Comments may also be submitted electronically to the 30 Responsible Officer: Dr Tiequn Zhou at: [email protected]. 31 32 The outcome of the deliberations of the Expert Committee will be published in the WHO 33 Technical Report Series. The final agreed formulation of the document will be edited to be in 34 conformity with the second edition of the WHO style guide (KMS/WHP/13.1). -

TOTAL RNA Microrna LABELED CRNA GENOMIC DNA HYB MIX
YALE CENTER FOR GENOME ANALYSIS – MICROARRAY SAMPLE SUBMISSION FORM SHIP TO: YCGA B‐36, 300 HEFFERNAN DRIVE, WEST HAVEN, CT 06516; 203‐737‐3047 (LAB); 203‐737‐3104 (FAX) NAME DATE NEW USER? YES NO‐ YMD USER CODE: E‐MAIL ADDRESS (ONE ONLY) TO SEND DATA P.I. BILLING ADDRESS P.I. E‐MAIL ADDRESS DEPARTMENT INSTITUTION SHIPPING ADDRESS TELEPHONE # YALE PTAEO / PURCHASE ORDER # SPLIT CHARGING? 2ND PTAEO SAMPLE TYPE SERVICE REQUESTED PLATFORM TOTAL RNA FULL SERVICE GENE EXPRESSION PROFILING* AFFYMETRIX (ISOLATED & PURIFIED) NUGEN GENE EXPRESSION PROFILING* microRNA FULL SERVICE SNP GENOTYPING* EXIQON (ISOLATED & PURIFIED) METHLYATION* LABELED CRNA ILLUMINA (PURIFIED) MICRORNA EXPRESSION PROFILING GENOMIC DNA HYBRIDIZATION ONLY NIMBLEGEN (ISOLATED & PURIFIED) SAMPLE QC (SPECTROPHOTOMETRY & BIOANALYZER) HYB MIX OTHER: SEQUENOM CELL TYPE / EXTRACTION METHOD: # OF SAMPLES MICROARRAY NAME (SPECIES AND VERSION #) PROVIDED BY: QTY. REC.: USER FACILITY SAMPLE OR PLATE NAME CONC. VOL SAMPLE OR PLATE NAME CONC. VOL SAMPLE OR PLATE NAME CONC. VOL 1 5 9 2 6 10 3 7 11 4 8 12 *THE FACILITY IS NOT RESPONSIBLE FOR ANY SAMPLES THAT FAIL DUE TO INADEQUATE CONCENTRATION OR QUALITY. We assume ALL samples (including DNA for genotyping & methylation) submitted to us have met the posted recommendations listed on our website for processing. Sample terminated due to poor QC will still be subject to appropriate service charges. HIC APPROVED PROJECT? SOFTWARE TUTORIAL REQUESTED. NORMALIZATION METHOD REQUESTED: ALL SAMPLES MAY BE DISCARDED IF NOT RETRIEVED WITHIN 60 DAYS OF DATA POSTING. Sample forms without signatures will not be brought to West Campus. Apologies for any inconvenience. The samples listed above do not contain any of the following: radioactive material, hazardous chemicals (e.g. -

The Binding of Monoclonal and Polyclonal Anti-Z-DNA Antibodies to DNA of Various Species Origin
International Journal of Molecular Sciences Article The Binding of Monoclonal and Polyclonal Anti-Z-DNA Antibodies to DNA of Various Species Origin Diane M. Spencer 1,2, Angel Garza Reyna 3 and David S. Pisetsky 1,2,* 1 Department of Medicine and Immunology, Division of Rheumatology, Duke University Medical Center, Durham, NC 27710, USA; [email protected] 2 Medical Research Service, Veterans Administration Medical Center, Durham, NC 27705, USA 3 Department of Chemistry, Duke University, Durham, NC 27705, USA; [email protected] * Correspondence: [email protected] Abstract: DNA is a polymeric macromolecule that can display a variety of backbone conformations. While the classical B-DNA is a right-handed double helix, Z-DNA is a left-handed helix with a zig-zag orientation. The Z conformation depends upon the base sequence, base modification and supercoiling and is considered to be transient. To determine whether the presence of Z-DNA can be detected immunochemically, the binding of monoclonal and polyclonal anti-Z-DNA antibodies to a panel of natural DNA antigens was assessed by an ELISA using brominated poly(dG-dC) as a control for Z-DNA. As these studies showed, among natural DNA tested (Micrococcus luteus, calf thymus, Escherichia coli, salmon sperm, lambda phage), micrococcal (MC) DNA showed the highest binding with both anti-Z-DNA preparations, and E. coli DNA showed binding with the monoclonal anti-DNA preparation. The specificity for Z-DNA conformation in MC DNA was demonstrated by an inhibition binding assay. An algorithm to identify propensity to form Z-DNA indicated that Citation: Spencer, D.M.; Reyna, A.G.; Pisetsky, D.S. -

Advances in Oligonucleotide Drug Delivery
REVIEWS Advances in oligonucleotide drug delivery Thomas C. Roberts 1,2 ✉ , Robert Langer 3 and Matthew J. A. Wood 1,2 ✉ Abstract | Oligonucleotides can be used to modulate gene expression via a range of processes including RNAi, target degradation by RNase H-mediated cleavage, splicing modulation, non-coding RNA inhibition, gene activation and programmed gene editing. As such, these molecules have potential therapeutic applications for myriad indications, with several oligonucleotide drugs recently gaining approval. However, despite recent technological advances, achieving efficient oligonucleotide delivery, particularly to extrahepatic tissues, remains a major translational limitation. Here, we provide an overview of oligonucleotide-based drug platforms, focusing on key approaches — including chemical modification, bioconjugation and the use of nanocarriers — which aim to address the delivery challenge. Oligonucleotides are nucleic acid polymers with the In addition to their ability to recognize specific tar- potential to treat or manage a wide range of diseases. get sequences via complementary base pairing, nucleic Although the majority of oligonucleotide therapeutics acids can also interact with proteins through the for- have focused on gene silencing, other strategies are being mation of three-dimensional secondary structures — a pursued, including splice modulation and gene activa- property that is also being exploited therapeutically. For tion, expanding the range of possible targets beyond example, nucleic acid aptamers are structured -

Comparing Yield and Quality of Genomic DNA and Total RNA from Cancer Cell Lines Using Allprep Kits Or Dedicated Kits for a Single Nucleic Acid Type
Technical Information Comparing yield and quality of genomic DNA and total RNA from cancer cell lines using AllPrep Kits or dedicated kits for a single nucleic acid type Introduction Human cancer-derived cell lines are the most widely used using our specialized AllPrep Kits and dedicated DNA models for studying cancer biology and for testing or RNA prep kits such as DNeasy® and RNeasy®. hypotheses to improve cancer treatment. Using an appropriate in vitro model in cancer research is crucial for Cell culture procedure investigating genetic, epigenetic and cellular pathways to 2 study proliferation, apoptosis and cancer progression, Cell lines were cultured in 75 cm tissue culture flasks at enabling potential molecular markers to be defined and 37°C and 5% CO2 until 80% confluence was reached. The cancer therapeutics to be screened and characterized. Best cell culture media used are listed consecutively in the table cell culture practice is essential for ensuring consistent and below. To harvest the cells, the media was removed and the reproducible results from the same cancer cell lines. cells were washed with PBS. The cells were removed from Simultaneous purification of high-quality genomic DNA and the plate after a short treatment (10–30 s) with 1 ml trypsin RNA from a single biological sample maximizes the use of using a cell-scraper. Cells were pelleted by centrifugation precious sample material, especially if only a limited number (2 min, 300 x g at room temperature) and washed with of cells are available. The AllPrep Kits have optimized PBS. The cells were centrifuged again and diluted to 1 x 6 nucleic acid purification protocols that allow simultaneous 10 cells/ml in PBS. -

De Novo Nucleic Acids: a Review of Synthetic Alternatives to DNA and RNA That Could Act As † Bio-Information Storage Molecules
life Review De Novo Nucleic Acids: A Review of Synthetic Alternatives to DNA and RNA That Could Act as y Bio-Information Storage Molecules Kevin G Devine 1 and Sohan Jheeta 2,* 1 School of Human Sciences, London Metropolitan University, 166-220 Holloway Rd, London N7 8BD, UK; [email protected] 2 Network of Researchers on the Chemical Evolution of Life (NoR CEL), Leeds LS7 3RB, UK * Correspondence: [email protected] This paper is dedicated to Professor Colin B Reese, Daniell Professor of Chemistry, Kings College London, y on the occasion of his 90th Birthday. Received: 17 November 2020; Accepted: 9 December 2020; Published: 11 December 2020 Abstract: Modern terran life uses several essential biopolymers like nucleic acids, proteins and polysaccharides. The nucleic acids, DNA and RNA are arguably life’s most important, acting as the stores and translators of genetic information contained in their base sequences, which ultimately manifest themselves in the amino acid sequences of proteins. But just what is it about their structures; an aromatic heterocyclic base appended to a (five-atom ring) sugar-phosphate backbone that enables them to carry out these functions with such high fidelity? In the past three decades, leading chemists have created in their laboratories synthetic analogues of nucleic acids which differ from their natural counterparts in three key areas as follows: (a) replacement of the phosphate moiety with an uncharged analogue, (b) replacement of the pentose sugars ribose and deoxyribose with alternative acyclic, pentose and hexose derivatives and, finally, (c) replacement of the two heterocyclic base pairs adenine/thymine and guanine/cytosine with non-standard analogues that obey the Watson–Crick pairing rules.