HCV Infection in South Australian Prisoners
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Charting New Waters 2015-2018
THREE YEARS ON 2015-2018 Charting new waters OUR GOVERNANCE BRINGING HOPE Offering the chance to change Bringing Hope is our in-prison volunteering program. Each week JOHN DR LYNN HENRY Second Chances SA volunteers visit prisons right across South DOYLE AC, QC ARNOLD AO OLONGA Australia - providing friendship and practical support including PATRON JUSTICE ADVOCATE AMBASSADOR banking and property storage. To break the cycle of crime we focus our attention on giving BOARD MEMBERS ADVISORY PANEL those in prison the opportunity to turn their life around. Our volunteers support prisoners before and after release - providing Chairman: Timothy Minahan Bob Brooks Glenn O’Rourke Gary Byron AM mentoring and friendship as they encourage those they come Vice Chairman: Julian Grobler Brenda Bates Jayme Watson Rev Bill Reddin alongside to live crime-free futures. Secretary: Les Dennis Geoff Glanville Peter Do Treasurer: Krystal Gurney Paula Dickson FROM THE CHAIRMAN FROM THE CEO 3,212 They said, “You won’t last the year” – but we did. After 20 years For two years we dreamt of relocating to ground floor offices, on with a national charity, we moved away 1 February 2015 to form a traffic corridor not far from the city precinct. As at 1 January Adult prisoners in SA* an exclusive South Australian charity. We wanted to be more 2018 we entered into a three year lease on 229 Fullarton Road *SA Department for Correctional Services (2018) holistic, focussed and expand our programs specifically on the Eastwood giving us our own place with off street parking. Second Chances SA in-prison volunteers work needs of the invisible victims of crime – the children of prisoners. -

Towards Safer and More Congruent Prison Environments for Male Aboriginal Prisoners a Southaustralian Study
({{ Iqlo, \ ''": ,'/ / ,':;r\'\' ., ..' Towards Safer and more Congruent Prison Environments for Male Aboriginal Prisoners A SouthAustralian Study Elizabeth Grant A thesis submitted to the University of Adelaide in fulfilment of the requirernents of the Degree of Doctor of Philosophy The School of Architecture, Landscape Architecture and Urban Design June2008 A Suulh Alisrra!iarl Table of Contents List of Figures .....................................................................................................................................................xi List of Tables ..................................................................................................................................................... xv Abbreviations .................................................................................................................................................. xvii Glossary of Terms ............................................................................................................................................ xix Abstract .......................................................................................................................... , ................................. xxi Declaration ..................................................................................................................................................... xxiii Acknowledgements ........................................................................................................................................ -

Annual Report 2010 – 2011
ANNUAL REPORT 2010 – 2011 Level 2, 400 King William Street ADELAIDE SA 5000 Telephone: 08 8226 9000 www.corrections.sa.gov.au CONTENTS DEPARTMENT FOR CORRECTIONAL SERVICES ......................................................................................... 6 HIGHLIGHTS 2010–11 ............................................................................................................................ 6 INTRODUCTION .................................................................................................................................... 7 YEAR IN REVIEW ................................................................................................................................... 8 STRATEGIC PLAN 2008-11 .............................................................................................................................................. 10 ORGANISATIONAL CHART........................................................................................................................................ 11 OVERVIEW OF THE DEPARTMENT FOR CORRECTIONAL SERVICES.................................................................... 12 OFFICE OF THE CHIEF EXECUTIVE ...................................................................................................................................... 12 STRATEGIC SERVICES ........................................................................................................................................................ 12 OFFENDER DEVELOPMENT .............................................................................................................................................. -

Correctional Services
Department for Correctional Services Financial report for the year ended 30 June 2018 Government of South Australia INDEPENDENT AUDITOR'S REPORT � Auditor-General's Department ��M1 Level 9 State Administration Centre 200 Victoria Square Adelaide SA 5000 DX 56208 Victoria Square Tel +618 8226 9640 Fax +618 8226 9688 ABN 53 327 061 410 [email protected] www.audit.sa.gov.au To the Chief Executive Department for Correctional Services As required by section 31 (1)(b) of the Public Finance and Audit Act 1987, I have audited the financialreport of the Department for Correctional Services for the financial year ended 30 June 2018. Opinion In my opinion, the accompanying financialreport gives a true and fair view of the financial position of the Department for Correctional Services as at 30 June 2018, its financial performance and its cash flows for the then year ended in accordance with the Treasurer's Instructions promulgated under the provisions of the Public Finance and Audit Act 1987 and Australian Accounting Standards. The financial report comprises: • a Statement of Comprehensive Income forthe year ended 30 June 2018 a Statement of Financial Position as at 30 June 2018 • a Statement of Changes in Equity for the year ended 30 June 2018 a Statement of Cash Flows for the year ended 30 June 2018 notes, comprising significantaccounting policies and other explanatory information • a Certificate fromthe Chief Executive and the Executive Director, People and Business Services. Basis for opinion I conducted the audit in accordance with the Public Finance and Audit Act 1987 and Australian Auditing Standards. -

August· \989 L------Ii
If you have issues viewing or accessing this file contact us at NCJRS.gov. I~' -=.~;z'_ ~..-! i!'£'i!i!_' ;""""6 ...... "'-"'-" ---- ~:FOICE OF CRIME STATISTICS Y - rney-Gen era I'5 Department " 2 sociAl iSSUES SEmESLIl.----------------:--: THE-- IMPACT Of PAROLE LEGISLATION CHANGE IN SOUTH AUSTRALIA , " . _________ ~AUGUST· \989 L-----------II S·A. DEPARTMENT OF C RESEARCH AND P ORRECTIONAL SERVICES LANNING UNIT l \ 15 I z.,7 Social Issues Series No. 2 August 1989 THE IMPACT OF PAROLE LEGISLATION CHANGES IN SOUTH AUSTRALIA DEPARTMENT OF CORRECTIONAL SERVICES ATIORNEY·GENERAL'S DEPARTMENT RESEARCH AND PLANNING UNIT OFFICE OF CRIME STATISTICS 118127 u.~. Department of JUstfce Nal/onal Institute of Justice This document has been re rodu ce ine~~on or organization origin~ing it : .e~act/y.as received from the IS document are those of the' % s of view or opinions stated ~:~~~ent the official position or POI~~~~o~~ t~ndNdo. not necessarily . e allonal Instilute of Permission to reprod h' granted by uce I IS copyrighled material has been -J\t~?LIL~_~GE~J1gra11 --Q£f~Q.e--.D£ Cr' -----.---~.-Pe&Cl...~'tmen t t~P~~,*~ J m~S.:tat j s tics I JUstice Reference Service (NCJRS Further reproduction outside of h J. Slon of Ihe copyright owner. I e NCJRS system requires permis. 1l1?/ZI CONTENTS PREFACE i 1. INTRODUCTION 1 2. PAROLE IN SOUTH AUSTRALIA 3 3. THE ORIGINS AND HISTORY OF PAROLE 5 4. HOW THE PAROLE CHANGES WERE COMMUNICATED AND ACCEPTED 11 4.1 The Views of Correctional Staff and Offenders 4.2 How Prison Managers and Judges Viewed the Parole Changes 5. -

Prisoner's Kids: the Invisible Victims of Crime
Prisoner’s Kids: The Invisible Victims of Crime An evidence-based report on the importance of a holistic approach to crime Prepared by Nova Smart Solutions For Second Chances SA July 2016 Executive summary This report from Nova Smart Solutions presents thorough, a positive impact in their lives and a very high return (i.e. evidence-based research that shows South Australia is facing a for every dollar spent there is an impact ten times larger). critical issue - the alarming lack of awareness of the situation Nevertheless, due to a lack of awareness by community and of children following the imprisonment of a parent. authorities about PKs, only few organisations in our country are taking action to tackle this issue. The current legal, prison and educational systems neglect these kids. In South Australia, when a person is imprisoned there is In South Australia, Second Chances SA (SCSA) has identified this not any formal record that captures his or her parenthood issue. SCSA is the only agency in South Australia (within and status. This data-capture failure contributes to neglect the outside of Government) that works implementing programs needs of a group of overlooked and vulnerable children that are that reduce the probability of PKs going to prison. themselves highly likely to end up in prison. This report presents an issue that we face as a society and The failure to track the status of these children risks fostering an breaks down the work that SCSA is currently doing with PKs. intergenerational cycle of crime. Whilst there is little research The benefits brought to our community by SCSA’s holistic about the probability of Prisoner’s Kids ending up in prison, the approach needs further financial support to continue and US Department of Justice estimates that imprisoning a parent improve its impacts in the future. -

Myles Flynn: a Criminal, Lunatic, & Alcoholic Who Unknowingly
Myles Flynn: A Criminal, Lunatic, & Alcoholic who unknowingly changed SA for the better. David Buob Glenside Hospital Historical Society Inc. Thursday 24th May 2018 The Crime Scene Block 14 Smelters (BHP) 1912 Block 14 Smelters in vicinity of sheds 16/17 – remnant chimneys when site cleared for MTT power turbines Municipal Tramways Trust – Power Turbines for the Tramlines (DC) Highway Robbery 1750 Last in UK in 1897 Jan 23rd 1902 John Greenway (Manager) & Joseph Winter (Assist Mgr) collected the BHP’s Block 14 Smelters payroll from the Union Bank and headed back towards the Ocean Steamers Wharf around 2pm with the £1,224 8s 6d. 2 Horsemen approached them as they came to a bend in the road, one of whom was wearing a blue jersey & butchers apron, common in the area, so all seemed in order. The horsemen quickened their pace and as they came up on either side of the horse and trap they shouted “Bail Up” - their faces were covered with black crepe masks. Joseph cut the pony with the whip and made a run for it. The robbers began firing their revolvers with one killing the pony instantly tossing both men onto the roadway. Whilst one man covered the two men with his pistol, the other grabbed the bag containing the money from the trap. As he did so two men ran up from Block 14 to assist the fallen men but were warned off. At that moment the wind briefly blew the crepe mask off the first man’s face. Both robbers rode off at speed, Joseph Winter taking out his pistol and firing a number of rounds & missing! The Escape Route The robbers went over Fisher Bridge, past the Colac Hotel and through Tin Town (The wool stores area), On to Grand Junction Rd, then Torrens Road, crossing the rail lines at the Cheltenham Station, on to Woodville, & the Reed Beds at Fulham Gardens. -
Growth in the Prison Population - Impact on Custodial and Community Corrections Capacity - Options for the Future
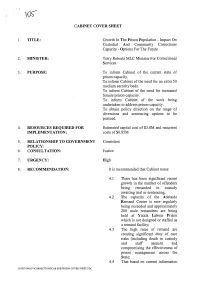
CABINET COVER SHEET TITLE: Growth In The Prison Population - Impact On Custodial And Community Corrections Capacity - Options For The Future MINISTER: Terry Roberts MLC Minister For Correctional Services 3. PURPOSE: To inform Cabinet of the current state of prison capacity. To inform Cabinet of the need for an extra 50 medium security beds. To inform Cabinet of the need for increased female prison capacity. To inform Cabinet of the work being undertaken to address prison capacity. To obtain policy direction on the range of diversions and sentencing options to be pursued. 4. RESOURCES REQUIRED FOR Estimated capital cost of $3.8M and recurrent IMPLEMENTATION: costs of $0.85M 5. RELATIONSHIP TO GOVERNMENT Consistent POLICY: 6. CONSULTATION: Justice 7. URGENCY: High 8. RECOMMENDATION: It is recommended that Cabinet notes: 4.1 There has been significant recent growth in the number of offenders being remanded in custody awaiting trial or sentencing; 4.2 The capacity of the Adelaide Remand Centre is now regularly being exceeded and approximately 200 male remandees are being held at Yatala Labour Prison which is not designed or staffed as a remand facility; 4.3 The high rates of remand are creating significant duty of care risks (including death in custody and staff assault) and compromising the effectiveness of prison management across the State; 4.4 That based on current information G:\JSU\TMLOV\CORRECTIONS\CAB SUB PRISON COVER SHEET.DOC -2- available, the numbers of remand and sentenced prisoners is expected to continue to increase; 4.5 That -

Trainee Correctional Officers Thinking of Joining Corrections?
FOR OPPORTUNITY. FLEXIBILITY. PURPOSE. TRAINEE CORRECTIONAL OFFICERS Department For Correctional Services Yatala Labour Prison, Adelaide Womens Prison/Pre-Release Centre, Mobilong Prison, Port Augusta, Port Lincoln Prison and Cadell Training Centre Full Time/Part Time Positions Available Training Salary: $51,120 pa (CO1) for first 12 weeks plus superannuation Qualified Salary: $55,315 - $63,026 pa (CO2) after 12 weeks plus superannuation The base salary plus appropriate penalties equates to an approximate annual average of $68,500 pa plus Superannuation. THINKING OF JOINING CORRECTIONS? The Department for Correctional Services (DCS) offers career opportunities that are challenging, demanding and rewarding. DCS contributes to building a safe, just and fair society where the supervision and rehabilitation of offenders is humane, and the rights of the victims are respected. Trainee Correctional Officers work in South Australian institutions performing a range of duties related to the security, safety and welfare of prisoners. This is a unique opportunity to provide a positive role model to prisoners. You will contribute to prisoner rehabilitation efforts to reduce the risk of re-offending on return to the community. DCS is a socially inclusive employer that recognises the benefits of having a workforce that reflects community diversity and culture. We strive to achieve a diverse range of Correctional Officers and encourage applications from Aboriginal and/or Torres Strait Islander people, LGBTIQA+, and women. Part time positions are available as part of the SA Government’s commitment to diversity and workplace flexibility. Candidates must be aged 18 years or over, be a Permanent resident or Australian citizen and possess a current unrestricted driver’s licence. -

South Australian's Safety and Security
MINISTER FOR POLICE, EMERGENCY SERVICES AND CORRECTIONAL SERVICES HON VINCENT TARZIA MP MEDIA RELEASE Tuesday 22 June 2021 South Australians’ safety and security supported with increased investment for Police and Emergency Services Almost $100 million has been dedicated to SAPOL over the last two budgets for its COVID-19 response as officers continue their valued work protecting South Australians, forming part of the Marshall Liberal Government’s crucial recovery plan from the pandemic. A total $77.5million is invested in SAPOL in today’s State Budget 2021-22 to support the continued COVID-19 operational response at medi-hotels, border checkpoints and for compliance tasks. This includes a significant boost to policing resources across the state to further enhance the safety and security of South Australians, with $15.2m provided in 2021-22 and a further $8.4m in 2022-23 to extend the employment of 54 Protective Security Officers (PSO’s) employed in 2020-21 and recruit and train an additional 114 PSO’s. “The Marshall Government is dedicated to forging a safe passage out of the pandemic while supporting SAPOL and its hardworking officers who protect South Australians,” Minister for Police, Emergency Services and Correctional Services Vincent Tarzia said. “We value the critical work they do in keeping the community safe, and the Government’s increased investment for SAPOL will ensure they continue to be well-resourced and well- equipped to carry out their important duties.” Stage 3 and 4 of SAPOL’s Shield System will get $21.2m over three years to finalise the implementation of a comprehensive integrated system, directly linking with other justice sector agencies, not only improving data sharing but leading to a more efficient use of policing resources. -

The Health of Australia's Prisoners 2009
The health of Australia’s prisoners 2009 The Australian Institute of Health and Welfare is Australia’s national health and welfare statistics and information agency. The Institute’s mission is better information and statistics for better health and wellbeing. © Australian Institute of Health and Welfare 2010 This work is copyright. Apart from any use as permitted under theCopyright Act 1968, no part may be reproduced without prior written permission from the Australian Institute of Health and Welfare. Requests and enquiries concerning reproduction and rights should be directed to the Head, Media and Communications Unit, Australian Institute of Health and Welfare, GPO Box 570, Canberra ACT 2601. A complete list of the Institute’s publications is available from the Institute’s website <www.aihw.gov.au>. ISBN 978-1-74249-011-3 Suggested citation Australian Institute of Health and Welfare 2010. The health of Australia’s prisoners 2009. Cat. no. PHE 123. Canberra: AIHW. Australian Institute of Health and Welfare Board Chair Hon. Peter Collins, AM, QC Director Penny Allbon Any enquiries about or comments on this publication should be directed to: Ingrid Johnston Australian Institute of Health and Welfare GPO Box 570 Canberra ACT 2601 Phone: (02) 6244 1211 Email: [email protected] Published by the Australian Institute of Health and Welfare Design and typesetting by Sam Highley Printed by Union Offset Printers Cover art by an Indigenous offender Please note that there is the potential for minor revisions of data in this report. Please check the online version at <www.aihw.gov.au> for any amendments. Foreword Foreword An estimated 50,000 people are released from prison each year in Australia. -
Nnual Report
If you have issues viewing or accessing this file contact us at NCJRS.gov. WITH THE COMPLIMENTS OF THE ::/)iJ'ec/ol' ADELAIDE nnual Report Director, Department of Correctional Services 1973-74 r - SOUTH AUSTRALIA ANNUAL REPORT OF THE South Australian Departlnent OF Correctional Services For the Year 1973-74 " By AUTHORITY: A. B. JAMES, Government Printer, South Australia 1975 rl r [p.P.38 Report on the Activities of the Department of Correctional Services for the Year 1973-74 The Honourable the Chief Secretary. Sir-t have the honour to pre~ent my report on the activities of the Dep<lrtment llf Corre~tional S~f\ ke~ for the year ended 30th June, J 974. The mo~t ~igniiicant feature for the year \\-as undoubtedly the publkation of the hr~t Repllft of the Criminal Law and Penal Methods Reform Committee. Whiht there are many ueLi"ions yet required on the sections to be implementeu and the priorities to be ob~er.,eu, we ha\e had. for the fir"t time ~in(e the early J 900\ (-,0 far as l can ascertain) an inuepenuent re\ie\~ of the whole "y,tem. \VlIiI..,t a number of the recommendation" have been departmental policy for .,ome time. the review of legislation , .. ill formalise much or what b being uone, and the other change,> emi~aged are at present hein,!! u'i,>e..,..,ed and reported on. Probably the most intere'>ting aspect of the Fir..,t Report wa.., it-. re(llmmelhlation that the department shoulu continue to lIe\c1op a.., an integrateu unit.