NEUROPATHIC PAIN: ARE YOU SEEING IT PAIN MANAGEMENT MORE THAN YOU THINK? (YES) Mark Epstein, DVM, DABVP (C/F), CVPP
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Generalized Edema Resulting from Mixed Intestinal Infection by Entamoebia Histolytica and E
Case Report JOJ Case Stud Volume 12 Issue 2 -April 2021 Copyright © All rights are reserved by Ajite Adebukola DOI: 10.19080/JOJCS.2021.12.555833 Generalized Edema Resulting from Mixed Intestinal Infection by Entamoebia Histolytica and E. Coli in a Nigerian Female Adolescent: A Case Report Ajite Adebukola1,2*, Oluwayemi Oludare1,2 and Fatunla Odunayo2 1Department of Paediatrics, Ekiti State University, Nigeria 2Department of Paediatrics, Ekiti State University Teaching Hospital, Nigeria Submission: March 15, 2021; Published: April 08, 2021 *Corresponding author: Ajite Adebukola, Consultant Paediatrician, Department of Paediatrics, Ekiti State University, Ado Ekiti, Nigeria Abstract Amoebiasis, a clinical condition caused by Entamoeba histolytica does not usually present with generalized oedema known as anarsarca. We present a case of an adolescent female Nigerian who was admitted on account of chronic diarrhea and anarsarca in a tertiary hospital, Southwest Nigeria. There was no proteinuria. She however had cyst of E. histolytica and growth of E. coli in her stool; she also had E. coli isolated in her urine. She had hypoproteinaemia (35.2g/L) and hypoalbuminaemia (21.3g/L) as well as hypokalemia (2.97mmol/L). Symptoms resolved Entamoeba histolytica and Escherichia coli bacteria may be responsible for the worse clinical manifestations of Amoebiasis and biochemical parameters normalized following treatment with Nitrofurantoin, Tinidazole and Ciprofloxacin. A mixed infection of Keywords: Amoebiasis; Chronic diarrhea; Hypoproteinaemia; Anasarca Introduction Amoebiasis, caused by the protozoan Entamoeba histolytica of amenorrhoea. is an infection that frequently manifests clinically with symptoms recurrent generalized body swelling, and a seven-month history of abdominal pain, diarrhoea, dysentery and weight loss [1,2]. -

Ehrlichiosis and Anaplasmosis Are Tick-Borne Diseases Caused by Obligate Anaplasmosis: Intracellular Bacteria in the Genera Ehrlichia and Anaplasma
Ehrlichiosis and Importance Ehrlichiosis and anaplasmosis are tick-borne diseases caused by obligate Anaplasmosis: intracellular bacteria in the genera Ehrlichia and Anaplasma. These organisms are widespread in nature; the reservoir hosts include numerous wild animals, as well as Zoonotic Species some domesticated species. For many years, Ehrlichia and Anaplasma species have been known to cause illness in pets and livestock. The consequences of exposure vary Canine Monocytic Ehrlichiosis, from asymptomatic infections to severe, potentially fatal illness. Some organisms Canine Hemorrhagic Fever, have also been recognized as human pathogens since the 1980s and 1990s. Tropical Canine Pancytopenia, Etiology Tracker Dog Disease, Ehrlichiosis and anaplasmosis are caused by members of the genera Ehrlichia Canine Tick Typhus, and Anaplasma, respectively. Both genera contain small, pleomorphic, Gram negative, Nairobi Bleeding Disorder, obligate intracellular organisms, and belong to the family Anaplasmataceae, order Canine Granulocytic Ehrlichiosis, Rickettsiales. They are classified as α-proteobacteria. A number of Ehrlichia and Canine Granulocytic Anaplasmosis, Anaplasma species affect animals. A limited number of these organisms have also Equine Granulocytic Ehrlichiosis, been identified in people. Equine Granulocytic Anaplasmosis, Recent changes in taxonomy can make the nomenclature of the Anaplasmataceae Tick-borne Fever, and their diseases somewhat confusing. At one time, ehrlichiosis was a group of Pasture Fever, diseases caused by organisms that mostly replicated in membrane-bound cytoplasmic Human Monocytic Ehrlichiosis, vacuoles of leukocytes, and belonged to the genus Ehrlichia, tribe Ehrlichieae and Human Granulocytic Anaplasmosis, family Rickettsiaceae. The names of the diseases were often based on the host Human Granulocytic Ehrlichiosis, species, together with type of leukocyte most often infected. -

How to Recognize a Suspected Cardiac Defect in the Neonate
Neonatal Nursing Education Brief: How to Recognize a Suspected Cardiac Defect in the Neonate https://www.seattlechildrens.org/healthcare- professionals/education/continuing-medical-nursing-education/neonatal- nursing-education-briefs/ Cardiac defects are commonly seen and are the leading cause of death in the neonate. Prompt suspicion and recognition of congenital heart defects can improve outcomes. An ECHO is not needed to make a diagnosis. Cardiac defects, congenital heart defects, NICU, cardiac assessment How to Recognize a Suspected Cardiac Defect in the Neonate Purpose and Goal: CNEP # 2092 • Understand the signs of congenital heart defects in the neonate. • Learn to recognize and detect heart defects in the neonate. None of the planners, faculty or content specialists has any conflict of interest or will be presenting any off-label product use. This presentation has no commercial support or sponsorship, nor is it co-sponsored. Requirements for successful completion: • Successfully complete the post-test • Complete the evaluation form Date • December 2018 – December 2020 Learning Objectives • Describe the risk factors for congenital heart defects. • Describe the clinical features of suspected heart defects. • Identify 2 approaches for recognizing congenital heart defects. Introduction • Congenital heart defects may be seen at birth • They are the most common congenital defect • They are the leading cause of neonatal death • Many neonates present with symptoms at birth • Some may present after discharge • Early recognition of CHD -

Cutaneous Manifestations of Abdominal Arteriovenous Fistulas
Cutaneous Manifestations of Abdominal Arteriovenous Fistulas Jessica Scruggs, MD; Daniel D. Bennett, MD Abdominal arteriovenous (A-V) fistulas may be edema.1-3 We report a case of abdominal aortocaval spontaneous or secondary to trauma. The clini- fistula presenting with lower extremity edema, ery- cal manifestations of abdominal A-V fistulas are thema, and cyanosis that had been previously diag- variable, but cutaneous findings are common and nosed as venous stasis dermatitis. may be suggestive of the diagnosis. Cutaneous physical examination findings consistent with Case Report abdominal A-V fistula include lower extremity A 51-year-old woman presented to the emergency edema with cyanosis, pulsatile varicose veins, department with worsening lower extremity swelling, and scrotal edema. redness, and pain. Her medical history included a We present a patient admitted to the hospital diagnosis of congestive heart failure, chronic obstruc- with lower extremity swelling, discoloration, and tive pulmonary disease, hepatitis C virus, tobacco pain, as well as renal insufficiency. During a prior abuse, and polysubstance dependence. Swelling, red- hospitalization she was diagnosed with venous ness, and pain of her legs developed several years stasis dermatitis; however, CUTISher physical examina- prior, and during a prior hospitalization she had been tion findings were not consistent with that diagno- diagnosed with chronic venous stasis dermatitis as sis. Imaging studies identified and characterized well as neurodermatitis. an abdominal aortocaval fistula. We propose that On admission, the patient had cool lower extremi- dermatologists add abdominal A-V fistula to the ties associated with discoloration and many crusted differential diagnosis of patients presenting with ulcerations. Aside from obesity, her abdominal exam- lower extremity edema with cyanosis, and we ination was unremarkable and no bruits were noted. -

Pedal Edema in Older Adults Jennifer M
www.aging.arizona.edu July 2013 (updated May2015) ELDER CARE A Resource for Interprofessional Providers Pedal Edema in Older Adults Jennifer M. Vesely, MD, Teresa Quinn, MD, and Donald Pine, MD, Family Medicine Residency, University of Minnesota Pedal edema is the accumulation of fluid in the feet and pedal edema, which is more common in older adults, is lower legs. It is typically caused by one of two mechanisms. often multifactorial and may reflect a systemic process. The first is venous edema, caused by increased capillary Treating the underlying cause can often lessen the edema. filtration and retention of protein-poor fluid from the Table 1 lists common and less common causes of bilateral venous system into the interstitial space. The other pedal edema. mechanism is lymphatic edema, caused by obstruction or In addition to seeking evidence for the conditions listed in dysfunction of lymphatic outflow from the legs resulting in Table 1, certain clues in the patient’s presentation might accumulation of protein-rich interstitial fluid. These two point to a particular cause of edema. In particular, the mechanisms can operate independently or together. duration of edema and presence of pain should be noted. Regardless of the mechanism, chronic bilateral pedal Acute onset and presence of edema for less than 72 hours edema is detrimental to the health and quality of life of suggests the possibility of venous thrombosis and steps older adults. Besides alterations in cosmetic appearance or should be taken to exclude that diagnosis. Edema due to the discomfort it may cause, older adults with pedal edema chronic venous insufficiency is often associated with a dull often experience gait disturbance with decreased mobility aching pain. -

Review of Systems Health History Sheet Patient: ______DOB: ______Age: ______Gender: M / F
603 28 1/4 Road Grand Junction, CO 81506 (970) 263-2600 Review of Systems Health History Sheet Patient: _________________ DOB: ____________ Age: ______ Gender: M / F Please mark any symptoms you are experiencing that are related to your complaint today: Allergic/ Immunologic Ears/Nose/Mouth/Throat Genitourinary Men Only Frequent Sneezing Bleeding Gums Pain with Urinating Pain/Lump in Testicle Hives Difficulty Hearing Blood in Urine Penile Itching, Itching Dizziness Difficulty Urinating Burning or Discharge Runny Nose Dry Mouth Incomplete Emptying Problems Stopping or Sinus Pressure Ear Pain Urinary Frequency Starting Urine Stream Cardiovascular Frequent Infections Loss of Urinary Control Waking to Urinate at Chest Pressure/Pain Frequent Nosebleeds Hematologic / Lymphatic Night Chest Pain on Exertion Hoarseness Easy Bruising / Bleeding Sexual Problems / Irregular Heart Beats Mouth Breathing Swollen Glands Concerns Lightheaded Mouth Ulcers Integumentary (Skin) History of Sexually Swelling (Edema) Nose/Sinus Problems Changes in Moles Transmitted Diseases Shortness of Breath Ringing in Ears Dry Skin Women Only When Lying Down Endocrine Eczema Bleeding Between Shortness of Breath Increased Thirst / Growth / Lesions Periods When Walking Urination Itching Heavy Periods Constitutional Heat/Cold Intolerance Jaundice (Yellow Extreme Menstrual Pain Exercise Intolerance Gastrointestinal Skin or Eyes) Vaginal Itching, Fatigue Abdominal Pain Rash Burning or Discharge Fever Black / Tarry Stool Respiratory Waking to Urinate at Weight Gain (___lbs) Blood -

Drug Eruptions- When to Worry
3/17/2017 Drug reactions: Drug Eruptions‐ When to Worry 3 things you need to know 1. Type of drug reaction 2. Statistics: – Which drugs are most likely to cause that type of Lindy P. Fox, MD reaction? Associate Professor 3. Timing: Director, Hospital Consultation Service – How long after the drug started did the reaction Department of Dermatology University of California, San Francisco begin? [email protected] I have no conflicts of interest to disclose 1 Drug Eruptions: Common Causes of Cutaneous Drug Degrees of Severity Eruptions • Antibiotics Simple Complex • NSAIDs Morbilliform drug eruption Drug hypersensitivity reaction Stevens-Johnson syndrome •Sulfa (SJS) Toxic epidermal necrolysis (TEN) • Allopurinol Minimal systemic symptoms Systemic involvement • Anticonvulsants Potentially life threatening 1 3/17/2017 Morbilliform (Simple) Drug Eruption Morbilliform (Simple) Drug Eruption Per the drug chart, the most likely culprit is: Per the drug chart, the most likely culprit is: Day Day Day ‐> ‐8 ‐7 ‐6 ‐5 ‐4 ‐3 ‐2 ‐1 0 1 Day ‐> ‐8 ‐7 ‐6 ‐5 ‐4 ‐3 ‐2 ‐1 0 1 A vancomycin x x x x A vancomycin x x x x B metronidazole x x B metronidazole x x C ceftriaxone x x x C ceftriaxone x x x D norepinephrine x x x D norepinephrine x x x E omeprazole x x x x E omeprazole x x x x F SQ heparin x x x x F SQ heparin x x x x trimethoprim/ trimethoprim/ G xxxxxxx G xxxxxxx sulfamethoxazole sulfamethoxazole Admit day Rash onset Admit day Rash onset Morbilliform (Simple) Drug Eruption Drug Induced Hypersensitivity Syndrome • Begins 5‐10 days after drug started -
Practical Approach to Lower Extremity Edema
Practical Approach to Lower Extremity Edema BRETT C. STOLL, MD, FACC, FCCP FEB 22, 2014 Not Everything that Swells is Heart Failure BRETT C. STOLL, MD, FACC, FCCP FEB 22, 2014 Overview A common challenge for primary care physicians and cardiologists alike Goal is to determine the cause and find an effective treatment for leg edema Despite the prevalence, no formal existing practice guidelines at present Definition Edema is defined as a palpable swelling caused by an increase in interstitial fluid volume. Edema, other than localized edema, does not become clinically apparent until the interstitial volume has increased by 2.5 to 3 liters. Etiology of Edema Increase in intravascular pressure Increase in capillary vessel wall permeability Decrease in the intravascular osmotic pressure Excess bodily fluids Lymphatic obstruction Local injury Infection Medication effect Anatomy and Pathophysiology Anatomy and Pathophysiology Starling's Law of Capillaries Anatomy and Pathophysiology Introduction The most likely cause of leg edema in patients over age 50 is venous insufficiency Venous insufficiency affects up to 30% of the population Heart failure affects only approximately 1% Introduction The most likely cause of leg edema in women under age 50 is idiopathic edema (formerly known as cyclic edema). Introduction Most patients can be assumed to have one of these diseases unless another cause is suspected after a history and physical examination. However, there are at least 2 exceptions to this rule: pulmonary hypertension early heart failure Both conditions can both cause leg edema before they become clinically obvious in other ways. Classification There are two types of leg edema: Venous edema consists of excess low-viscosity, protein-poor interstitial fluid resulting from increased capillary filtration that cannot be accommodated by a normal lymphatic system. -

DRESS Syndrome: Improvement of Acute Kidney Injury and Rash with Corticosteroids Dawnielle Endly, DO,* Jonathan Alterie, BS,** David Esguerra, DO,*** Richard A
DRESS Syndrome: Improvement of Acute Kidney Injury and Rash with Corticosteroids Dawnielle Endly, DO,* Jonathan Alterie, BS,** David Esguerra, DO,*** Richard A. Miller, DO**** *Co-lead Author, Dermatology Resident, Nova Southeastern University College of Osteopathic Medicine/Largo Medical Center, Largo, FL **Co-lead Author, 4th-year Medical Student, Chicago College of Osteopathic Medicine, Chicago, IL ***Clinical Professor, Nova Southeastern University College of Osteopathic Medicine, Largo, FL ****Program Director, Dermatology Residency Program, Nova Southeastern University College of Osteopathic Medicine/Largo Medical Center, Largo, FL Abstract DRESS syndrome (drug rash with eosinophilia and systemic symptoms) is a rare and potentially life-threatening idiosyncratic drug reaction that may involve a number of visceral organs. This syndrome often mimics other serious systemic disease processes, making the diagnosis complicated and often delayed. Herein, we present a unique case of DRESS syndrome accompanied by acute interstitial nephritis that responded to oral prednisone during a hospital stay. Introduction superficial dermis. The patient reported minimal negative. An echocardiogram revealed a decrease DRESS syndrome is a drug reaction that symptomatic relief, but the rash progressed and in EF from 25% at baseline to 10% to 20% with usually manifests with fever, a pruritic macular became generalized with total body involvement. severe diffuse hypokinesis and severe biatrial and papular rash, hematologic abnormalities Due to clinical suspicion for a cutaneous drug enlargement. All clinical data was entered into (leukocytosis, eosinophilia, and/or atypical reaction, her primary care provider stopped the the RegiSCAR group diagnosis chart for DRESS lymphocytes), and internal organ involvement. furosemide and prescribed spironolactone a few syndrome and revealed a total of 7 (see Table 1), This drug reaction is characterized by a delayed days prior to her hospitalization. -

History & Physical Format
History & Physical Format SUBJECTIVE (History) Identification name, address, tel.#, DOB, informant, referring provider CC (chief complaint) list of symptoms & duration. reason for seeking care HPI (history of present illness) - PQRST Provocative/palliative - precipitating/relieving Quality/quantity - character Region - location/radiation Severity - constant/intermittent Timing - onset/frequency/duration PMH (past medical /surgical history) general health, weight loss, hepatitis, rheumatic fever, mono, flu, arthritis, Ca, gout, asthma/COPD, pneumonia, thyroid dx, blood dyscrasias, ASCVD, HTN, UTIs, DM, seizures, operations, injuries, PUD/GERD, hospitalizations, psych hx Allergies Meds (Rx & OTC) SH (social history) birthplace, residence, education, occupation, marital status, ETOH, smoking, drugs, etc., sexual activity - MEN, WOMEN or BOTH CAGE Review Ever Feel Need to CUT DOWN Ever Felt ANNOYED by criticism of drinking Ever Had GUILTY Feelings Ever Taken Morning EYE OPENER FH (family history) age & cause of death of relatives' family diseases (CAD, CA, DM, psych) SUBJECTIVE (Review of Systems) skin, hair, nails - lesions, rashes, pruritis, changes in moles; change in distribution; lymph nodes - enlargement, pain bones , joints muscles - fractures, pain, stiffness, weakness, atrophy blood - anemia, bruising head - H/A, trauma, vertigo, syncope, seizures, memory eyes- visual loss, diplopia, trauma, inflammation glasses ears - deafness, tinnitis, discharge, pain nose - discharge, obstruction, epistaxis mouth - sores, gingival bleeding, teeth, -

4 Edema in Childhood
Kidney International, Vol. 51, Suppl. 59 (1997). pp. S-100-S-104 (1) Red Hypo Ne] Liv Edema in childhood Ma Pre Sev SATOSHI HISANO, SEUNGHOON HAHN, NANCY B. KUEMMERLE, JAMES CM. CHAN, (2) Incr. and NATALE G. DESANTO Cardi He: h Pediatric Nephrology Division, Virginia Commonwealth University's Medical College of Virginia, Richmond, Virginia, USA, and Divisione di Nefrologia Art dell' Adulto e del Bambino, Seconda Universita'degli Studi di Napoli, Naples, Italy Renal Act ACt Idiops Fan Edema in childhood. There are two types of edema: localized edema sympathetic nervous system (SNS) activity; and (3) antidiuretic Nor and generalized edema. The causes ofgeneralized edema in childhoodare hormone (ADH) release [4-6]. These forces and perhaps as yet diverse. Formation of generalizededema involves retention of sodium and Prej unidentified factors give rise to the consequential water and water in the kidney. The treatment of generalized edema depends on the (3) Incre primary etiology. Supportive nutritional and medicaltherapies are needed sodium retention, which promotes the development of edema, Allerg to prevent further edema. These and related features of edema in The sodium and water retention leads to further decreased Vascu childhood are discussed in this review. den plasma oncotic pressure, setting up a vicious cycle perpetuating dise the edema formation. The movement of water from intracellular space to interstitial space by itself also contributes to the devel opment of edema formation [1, 3]. Edema can be defined as the presence of excess fluid in the In contrast, the mechanism of "overfilling edema" is expanded interstitial space of the body. Edema is divided into two types, extracellular volume that results from primary renal sodium localized edema and generalized edema. -
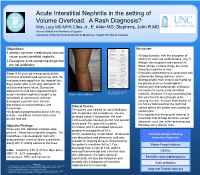
Acute Interstitial Nephritis in the Seeting of Volume Overload
Acute Interstitial Nephritis in the setting of Volume Overload. A Rash Diagnosis? Witt, Lucy MD MPH; Liles Jr., E. Allen MD; Stephens, John R MD Internal Medicine Residency Program University of North Carolina School of Medicine. Chapel Hill, North Carolina Objectives: Discussion: 1.Identify common medications that can cause acute interstitial nephritis. • All loop diuretics, with the exception of ethacrynic acid, are sulfonamides. (Fig 1) 2.Recognize sulfa-containing drugs that Allergic skin eruptions are common in are not antibiotics. those allergic to these drugs, but acute interstitial nephritis is rare.1 Case: A 49 year-old man presented with • Exfoliative erythroderma is associated with shortness of breath and worsening rash. He sulfonamide allergy reaction, and is had been discharged from the hospital four distinguishable from chronic dermatitis by days earlier after a nine day admission for the predominance of eosinophils.2 cellulitis and heart failure. During that • Vancomycin and sulfonamide antibiotics are known to cause acute interstitial admission he had been diagnosed with Fig 1. Structure of sulfonamide 3 acute interstitial nephritis thought to be Image 1. Rash and Edema antibiotics and diuretics nephritis, therefore it is not surprising that secondary to vancomycin and had this was the first drug thought to be developed a pruritic rash. He was causing his rash. A closer examination of his history indicated that the rash had discharged on oral prednisone and Clinical Course: furosemide. started before the patient was started on The patient was treated for atrial fibrillation vancomycin. His dyspnea progressed to occur with any with metoprolol and amiodarone. He was activity.