Annual Report and Accounts 2012/13
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Derbyshire Gritstone Way
A Walker's Guide By Steve Burton Max Maughan Ian Quarrington TT HHEE DDEE RRBB YYSS HHII RREE GGRRII TTSS TTOONNEE WW AAYY A Walker's Guide By Steve Burton Max Maughan Ian Quarrington (Members of the Derby Group of the Ramblers' Association) The Derbyshire Gritstone Way First published by Thornhill Press, 24 Moorend Road Cheltenham Copyright Derby Group Ramblers, 1980 ISBN 0 904110 88 5 The maps are based upon the relevant Ordnance Survey Maps with the permission of the controller of Her Majesty's Stationery Office, Crown Copyright reserved CONTENTS Foreward.............................................................................................................................. 5 Introduction......................................................................................................................... 6 Derby - Breadsall................................................................................................................. 8 Breadsall - Eaton Park Wood............................................................................................ 13 Eaton Park Wood - Milford............................................................................................... 14 Milford - Belper................................................................................................................ 16 Belper - Ridgeway............................................................................................................. 18 Ridgeway - Whatstandwell.............................................................................................. -

Area News Winter 2011 12 V2
Area News South Yorkshire and North-East Derbyshire Area Winter 2011/12 Annual Report and AGM Annual General Meeting This year the AGM will be hosted by Bolsover Group, and will be held on Saturday 28th January 2012 at 2pm at the Assembly Rooms, Hilltop, Bolsover S44 6NG grid ref SK473705. Bolsover is on the A632 east of Chesterfield. There will be a ramble before the AGM, starting from the Assembly Rooms at 1030. It will return in time for people to eat sandwiches (bring your own) before the meeting starts. Most existing Area officers are willing to stand for re-election, but Lee Farmery, our Chair for the last three years, plans to step down, and we are still looking for someone to do the Footpaths Secretary role. Anyone who would like to propose someone for a post should contact our Secretary David Gadd (address on the back page) or speak to Lee Farmery on 07789 077575. We will also elect the Area’s delegates to the national General Council. This is an impor- tant part of how the Ramblers works as a democratic organisation. We will also have interesting speakers to help us catch up on local and national developments. Chair’s Report I would like to say a big thank you to all of our new and existing volunteers within the SYNED Area for their efforts over the past Page 2 Area News year, be it leading a walk, actively campaigning, keeping us in- formed of issues, promoting the Ramblers and much more. The work of our volunteers often appears to go unnoticed, but they are an essential part of how the Ramblers operate. -

Skidmore Lead Miners of Derbyshire, and Their Descendants 1600-1915
Skidmore Lead Miners of Derbyshire & their descendants 1600-1915 Skidmore/ Scudamore One-Name Study 2015 www.skidmorefamilyhistory.com [email protected] SKIDMORE LEAD MINERS OF DERBYSHIRE, AND THEIR DESCENDANTS 1600-1915 by Linda Moffatt 2nd edition by Linda Moffatt© March 2016 1st edition by Linda Moffatt© 2015 This is a work in progress. The author is pleased to be informed of errors and omissions, alternative interpretations of the early families, additional information for consideration for future updates. She can be contacted at [email protected] DATES Prior to 1752 the year began on 25 March (Lady Day). In order to avoid confusion, a date which in the modern calendar would be written 2 February 1714 is written 2 February 1713/4 - i.e. the baptism, marriage or burial occurred in the 3 months (January, February and the first 3 weeks of March) of 1713 which 'rolled over' into what in a modern calendar would be 1714. Civil registration was introduced in England and Wales in 1837 and records were archived quarterly; hence, for example, 'born in 1840Q1' the author here uses to mean that the birth took place in January, February or March of 1840. Where only a baptism date is given for an individual born after 1837, assume the birth was registered in the same quarter. BIRTHS, MARRIAGES AND DEATHS Databases of all known Skidmore and Scudamore bmds can be found at www.skidmorefamilyhistory.com PROBATE A list of all known Skidmore and Scudamore wills - many with full transcription or an abstract of its contents - can be found at www.skidmorefamilyhistory.com in the file Skidmore/Scudamore One-Name Study Probate. -
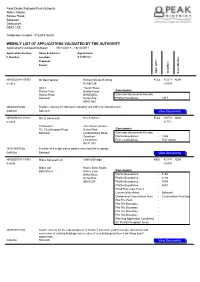
Weekly List of Applications Validated by the Authority
Peak District National Park Authority Aldern House, Baslow Road, Bakewell, Derbyshire, DE45 1AE Telephone number : 01629 816200 WEEKLY LIST OF APPLICATIONS VALIDATED BY THE AUTHORITY Applications validated between 05/10/2011 - 18/10/2011 Application Number: Name & Address: Agent Name P Number: Location: & Address: Proposal: Parish: Appl. type: Grid Ref.: Case Worker: NP/DDD/0911/0953 Mr Don Holland Richard Mundy Building FULL 422213 ADM P 1911 Design Ltd 369034 Unit 3 Travel House Station Yard Buxton Road Constraints Station Road BAKEWELL Sites and Monuments Records - Bakewell Derbyshire Plotfile Boundaries - 1911 DE45 1BZ DESCRIPTION Replace existing fire damaged industrial unit with new industrial unit PARISH Bakewell View Documents NP/DDD/1011/1011 Mrs E Hammond Mrs A Simms FULL 420782 ADM P 1285 367721 Chatsworth Vale Green Houses The Firs Monyash Road Belton Park Constraints Bakewell Londonthorpe Road Sites and Monuments Records - Grantham Plotfile Boundaries - 1285 Lincolnshire FCE Landholdings - FCE 26630 NG31 9SJ DESCRIPTION Erection of a single storey garden room and link to garage PARISH Bakewell View Documents NP/DDD/1011/1043 Midco Bakewell Ltd Oldfield Design REN 421795 ADM P 4158 368590 Midco Ltd Holme Bank Studio Bath Street Holme Lane, Constraints BAKEWELL Plotfile Boundaries - 4158 Derbyshire Plotfile Boundaries - 2194 DE451GF Plotfile Boundaries - 5559 Plotfile Boundaries - 6491 Flood Risk Area Zone 2 - Conservation Areas - Bakewell Designated Conservation Area - Conservation Area Boundary Plot File Point - Plot File Boundary - Plot File Boundary - Plot File Boundary - Plot File Boundary - Planning Application Conditions - EA Fluvial Floodplain areas - DESCRIPTION Retain consent for the redevelopment of builder's merchant yard to include demolition and conversion of existing buildings and erection of new buildings to form 4 dwellings and 5 apartments. -

Election of Police and Crime
46 THE COACHMAN'S OFFICE HERBERT'S TEAROOMS MAIN STREET TISSINGTON ASHBOURNE DE6 1RA ITI 112 ILH 37 ELECTION OF POLICE AND CRIME COMMISSIONER IEA 55 ING 5 47 COACH & HORSES FENNY BENTLEY ASHBOURNE DERBYSHIRE DE6 1LB IFB 133 DERBYSHIRE POLICE REGION - DERBYSHIRE DALES VOTING AREA 48 VILLAGE HALL THORPE ASHBOURNE DERBYSHIRE DE6 2AW ITH 125 49 OKEOVER ARMS MAPPLETON ASHBOURNE DERBYSHIRE DE6 2AB IMA 115 NOTICE OF SITUATION OF POLLING PLACES I should advise you that the DERBYSHIRE POLICE AND CRIME COMMISSIONER Election will take place on Thursday 5 50 TOWN HALL MARKET PLACE ASHBOURNE DERBYSHIRE DE6 1ES AAB 1316 AOU 361 May 2016 and the poll will take place between the hours of 07:00 am to 10:00 pm. Notice is hereby given that the polling 51 MOBILE UNIT AT SHAWCROFT CAR PARK ADJ PUBLIC CONVENIENCES SHAWCROFT CAR PARK OFF AAP 925 places and the voters assigned to each in this election shall be as follows: PARK ROAD ASHBOURNE DE6 1GH Polling Polling Place and address Polling District with 52 THE IMPERIAL ROOMS IMPERIAL ROAD MATLOCK DERBYSHIRE DE4 3NL QMB 1352 Station No No of Electors 53 ALL SAINTS CHURCH HALL SMEDLEY STREET MATLOCK DERBYSHIRE DE4 3JG QMA 1230 1 HATHERSAGE MEMORIAL HALL ODDFELLOWS ROAD HATHERSAGE HOPE VALLEY S32 1DU JHA 1275 JHI 19 JOF 4 JAB 32 54 HIGHFIELDS SCHOOL - WHEELDON HALL UPPER LUMSDALE MATLOCK DERBYSHIRE DE4 5NA QMC 982 2 BISHOP PAVILION THE BRIDGE FIELD GRINDLEFORD HOPE VALLEY S32 2AA JGR 612 55 HIGHFIELDS SCHOOL - WHEELDON HALL UPPER LUMSDALE MATLOCK DERBYSHIRE DE4 5NA PMC 564 3 EYAM MECHANIC'S INSTITUTE CHURCH STREET -

The Ultimate Peak District & Derbyshire Bucket List
The Ultimate Peak District & Derbyshire Bucket List: 101 Great Things To Do 1. Embrace the great outdoors in the UK’s first National Park Established in 1951, the Peak District is the country’s oldest National Park. If you love the outdoors, this protected area of natural beauty - which covers 555 square miles in total - offers over 200 square miles of stunning open access land to explore. 2. Visit the ‘jewel in the Peak District’s crown’ at Chatsworth House Home to the Duke and Duchess of Devonshire, Chatsworth is one of the UK’s favourite stately homes. Discover over 30 magnificent rooms, a 105-acre garden, parkland, a farmyard and playground, and one of Britain’s best farm shops. 3. Conquer the tallest ‘Peak’ in the Peak District At 636 metres above sea level, you’ll feel like you’re standing on top of the world when you conquer the Kinder Scout plateau. It’s the highest point in the National Park and was also the site of the 1932 Mass Trespass, a landmark event which sparked a debate about the right to roam in the countryside, leading to the establishment of the Peak District as the first National Park two decades later. 4. Discover the UK’s oldest Ice Age cave art at Creswell Crags Walk in the footsteps of Ice Age hunters, uncover the secrets of early man, discover incredible Ice Age cave art and marvel at the UK’s largest discovery of ritual protection marks at this picturesque limestone gorge on the Derbyshire/Nottinghamshire border. 5. -

DERBYSHIRE. IYS Byron Christphr
TBA.D.ES DIBECTOBY,] DERBYSHIRE. IYS Byron Christphr. :n5 Bath st. Ilkeston Gadsby H. F. r6 Tenant street, Derby Jackson Hy. 13 Spring gardens, Buxton Calvert A. M. King street, Bel per Gallimore J. O.Smith's Bank,LongEaton Jackson J oseph, Albert terrace, Bel per Capon George :L\1. Church street, Ripley Gamble\Villiam, Camphill street, Helper Jones John '1'. jun. Southgate, Ecking- CaponJ. T. Ripley Gandy F. H. 40 St. Mary's gate, Derby ton, Chesterfield Carnt W. G. r St. John's terrace,Bridge GascoyneEdwd.StonyMiddleton,Shefild Jordan W . .Matlock Bath street, Derby Gibson A. I Argyle street, Derby Joseph F. no Friar gate, Darby Carter George Edward, 4 Tythe Barn Glossop Charles Henry, Sheffield & Kelly P. J. Whittington moor, Chestrfld lane, Long Eaton, Nottingham Rotherham Bank, Bakewell Kerr John Hamilton, Sheffield & Union Case Robt. Hy. Ray st. Heanor R.S.O GlossopT.A. West view,Ambergate,Drby Bank, Chesterfield ChambersFrederick,2orAwsworthroad, Gooch H. E. Commercial Bank, Derby Kilford Henry James, Ilkeston Ilkeston R.S.O Goodwin Frank S.Bridge house,Bakewell Kitching Wm. The Terr.:tce, SJ.ltergate, Chambers James, Stanton-by-Dale Goodwin James H. Risley Chesterfield Chaplain Thomas,3 Clarence villas,Mat- Gratton & Marsden, Knifesmith gate, Knuwles W. Brassington, Wirksworth lock Bath, Derby Chesterfield Laban G. E. Hilton fields, Hilton Clark Geo. H. Holywell st. Chesterfield Gratton B. Church veiw, South Church Lancaster W. G. 10 Higl1 st. Chesterfld Clark Joseph, Hasland, Chesterfield street, Bakewell Lane Charles F. Old Hall road, New Clarke J .H.Canal tltreet ironworks, Drby GravesHorace,Derby & DerbyshireBank, Brampton, Chesterfield Clarke J. -
Web-A4-OA-ARTISTS-PRICE-LIST
Artist Title Media Price 1. Baker, Mags Hellebore W/C £100 2. Baker, Mags Poppy W/C £100 3. Broad, Hilary Colourful Calla A £60 4. Broad, Hilary Modest Magnolia A £60 5. Broad, Hilary Manarola - Italy T £60 6. Broad, Hilary Riber Castle T £60 7. Calvert, Pauline Over the Tops O £250 8. Calvert, Pauline Winter at Yeld Farm, Baslow A £295 9. Calvert, Pauline Winter Sun A £300 10. Calvert, Pauline Cornish Sea Shore A/MM £325 11. Crump, Amanda Portia (Warthog) C £390 12. Crump, Amanda Chulsum (Buffalo) C £650 13. Crump, Amanda Wangari (Leopard) C £585 14. Crump, Amanda Cayman (Aligator) C £675 15. Dodd, Susan Infanta and her Ape MM £390 16. Dodd, Susan Forget-Me-Not MM £390 17. Dodd, Susan Ancestors PE £500 18. Duvall, Judith Tulip Moon PR £150 19. Duvall, Judith Entry PR £160 20. Duvall, Judith Chime PR £160 21. Fearn, Judith Apples ‘5 A Day’ W/C £95 22. Fearn, Judith Pears ‘5 A Day’ W/C £95 23. Fearn, Judith Flowers (1) W/C £95 24. Fearn, Judith Flowers (2) W/C £95 25. Fearne, Peggy Summer of 18 T £220 26. Fearne, Peggy Meadow T £220 27. Fearne, Peggy Study in Blue T £350 28. Fearne, Peggy Summer Meadow T £325 29. Gilder, Diane Meadow in Pink T/A £650 30. Gilder, Diane Autumn (October 2016) T/A £950 31. Gilder, Diane Poppy Field W/C&G £350 32. Gilder, Diane Sea Birds W/C&G £200 33. Harpham, Angela Coast Re - Imagined 1 MM £120 34. -
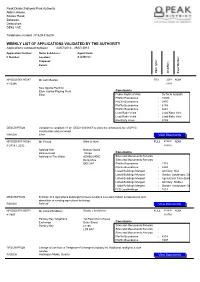
Weekly List of Applications Validated by the Authority
Peak District National Park Authority Aldern House, Baslow Road, Bakewell, Derbyshire, DE45 1AE Telephone number : 01629 816200 WEEKLY LIST OF APPLICATIONS VALIDATED BY THE AUTHORITY Applications validated between 03/07/2013 - 09/07/2013 Application Number: Name & Address: Agent Name P Number: Location: & Address: Proposal: Parish: Appl. type: Grid Ref.: Case Worker: NP/DDD/0513/0387 Mr John Buxton S73 2253 ADM P 10386 6108 New Sports Pavillion Elton Jubilee Playing Field Constraints Elton Public Rights of Way - De facto footpath Plotfile Boundaries - 10386 Plotfile Boundaries - 2975 Plotfile Boundaries - 6145 Plotfile Boundaries - 9261 Lead Rake Veins - Lead Rake Vein Lead Rake Veins - Lead Rake Vein Electricity Lines - 6733 DESCRIPTION Variation to condition 11 on DDD/1003/0687 to allow the windows to be of UPVC construction and not wood PARISH Elton View Documents NP/DDD/0713/0568 Mr P Hunt Allen & Hunt FULL 419991 ADM P 2718 + 2232 369765 Ashford Hall Narlow Works Baslow Road Thorpe Constraints Ashford-In-The-Water ASHBOURNE Sites and Monuments Records - Derbyshire Sites and Monuments Records - DE6 2AT Plotfile Boundaries - 2718 Plotfile Boundaries - 2232 Listed Buildings Merged - Ancillary: Wall Listed Buildings Merged - Garden Landscape: Gate Listed Buildings Merged - Agricultural: Farm Building Listed Buildings Merged - Ancillary: Stables Listed Buildings Merged - Garden Landscape: Garden Building FCE Landholdings - 1014 DESCRIPTION Erection of 4 agricultural buildings to house livestock & to store fodder & implements and demolition of existing agricultural buildings PARISH Ashford View Documents NP/DDD/0713/0571 Mr James Bradbury Studio J Architects FULL 414638 ADM P 7997 363758 Parsley Hay Telephone 1st Floor Munri House Exchange Duke Street Constraints Parsley Hay Leeds Sites and Monuments Records - LS9 8AG Sites and Monuments Records - Sites and Monuments Records - Plotfile Boundaries - 4218 Plotfile Boundaries - 7997 DESCRIPTION Change of use from a Telephone Exchange to holiday let. -

Statement of Persons Nominated Election of Parish Councillors
Derbyshire Dales District Council ELECTION OF PARISH COUNCILLORS FOR THE ALKMONTON PARISH STATEMENT OF PERSONS NOMINATED The following is a statement of the persons nominated for election as Parish Councillor for the said Electoral Division Persons Nominated 1 2 3 4 5 6 Surname Other Names Home Address Description Names of Proposer Reason why the person and Seconder nominated no longer stands nominated SUNNYCROFT PRO : JOSEPH D ALKMONTON NR. ARCHER BERESFORD MICHAEL J0HN ASHBOURNE SEC : JOSEPHINE M DERBYS DE6 3DH ARCHER The above persons have been and stand validly nominated. Dated:Friday 05 April 2019 Paul Wilson Returning Officer MATLOCK DERBYSHIRE DE4 3NN PRINTED AND PUBLISHED BY RETURNING OFFICER MATLOCK DERBYSHIRE DE4 3NN Derbyshire Dales District Council ELECTION OF PARISH COUNCILLORS FOR THE ASHBOURNE - BELLE VUE WARD PARISH STATEMENT OF PERSONS NOMINATED The following is a statement of the persons nominated for election as Parish Councillor for the said Electoral Division Persons Nominated 1 2 3 4 5 6 Surname Other Names Home Address Description Names of Proposer Reason why the person and Seconder nominated no longer stands nominated PRO : CHRISTOPHER DERBYSHIRE BERESFORD MOON DANNY DALES SEC : JOHN K BERESFORD 96 THE GREEN PRO : HELEN LYONS SPENCER MARTIN ROY ROAD ASHBOURNE SEC : JOHN C HARRISON DE6 1EE 96 THE GREEN SANDRA ROAD ASHBOURNE PRO : JOHN G BUCKLEY SPENCER MARION DERBYSHIRE DE6 SEC : JOHN C HARRISON 1EE The above persons have been and stand validly nominated. Dated:Friday 05 April 2019 Paul Wilson Returning Officer -

Curbar Parish Council 56 Upperthorpe Road Killamarsh
Curbar Parish Council 56 Upperthorpe Road Killamarsh Shefffield S21 1EJ Peak District National Park Authority Aldern House Baslow Road Bakewell Derbyshire DE45 1AE 19 November 2019 Dear Sirs Application Number: NP/DDD/0919/0987 Broughton Caravan Park Baslow Road Calver Curbar Change of use from grassland to a caravan park extension for 21 pitches. Alteration to the main road (A623) Curbar Parish Council resolved to object to the above planning application at its meeting on 12/11/2019. The access to Curbar and Calver coming along the A623 from Baslow, is a traditional picture of pasture land on the left, and gritstone buildings including the school, church, Bridge Inn and the Craft Centre complex, on the right. All these buildings are included in a Conservation Area. The extension of the static caravan site up to the roadside would destroy what the National Park Authority are trying to protect and is contrary to Policy GSP2; in that the scheme does not in anyway enhance a valued part of the village, the scheme offers no benefit at all to the natural beauty of the area and does not respect the character of the area. The proposed changes to the existing access fall within Calver Conservation Area No. 1 which extends into Curbar and includes the road frontage immediately adjoining the site up to the site boundary wall. The Core Strategy Policy RT3, relating to camping and caravans is very clear. RT3 B. states “Static caravans, chalets or lodges will not be permitted.” The impact of static caravans adjacent to the highway, which this will be, can be seen on High Street, Stoney Middleton where they have impacted on the street scene. -

Pedal Peak District Final Report
Pedal Peak District Final Report December 2009 – March 2011 Description Pedal Peak District was the Peak District National Park Authority’s premier cycling development project, funded and supported by the Department for Transport and Cycling England, from December 2009 to 31 March 2011. The project was fully supported by Derbyshire County Council, High Peak Borough Council, Derbyshire Dales District Council and Visit Peak District. Pedal Peak District has delivered significant infrastructure development and a social marketing programme. The Infrastructure work constituted a major element of this project. At the time of writing a great deal has been achieved and the works are still continuing for a late spring 2011 opening. The four closed tunnels have been cleared, surveyed and repaired and the entrance doors removed. Work is currently taking place to install a power supply and lighting. The tunnels, structures and a large proportion of the trail is also to be resurfaced and the access improved at Blackwell Mill Cottages, Great Longstone and Coombs Road. New signs will be put up on the trail, along with interpretation about the new route. This will include listening posts outlining the history of the tunnels. This work has involved the balancing of a large number of needs including detailed consideration of the unique landscape, conservation and heritage features of the trail, tunnels and the surrounding area. These features, and the issues that they raise, together with the limited project timescale have meant that the full link to Buxton through Woo Dale cannot be achieved in the project term. Planning consent has been achieved, through Peak Cycle Links, for a section of route to the north of Buxton at Staker Hill.