Mental Health and Substance Use Part 2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Individual Patient & Medication Factors That Invalidate Morphine
Individual Patient & Medication Factors that Invalidate Morphine Milligram Equivalents Presented on June 7-8, 2021 at FDA Collaborative with various Federal Government Agency Stakeholders Jeffrey Fudin, PharmD, FCCP, FASHP, FFSMB Clinical Pharmacy Specialist & PGY2 Pain Residency Director Stratton VAMC, Albany NY Adjunct Associate Professor Albany College of Pharmacy & Health Sciences, Albany NY Western New England University College of Pharmacy, Springfield MA President, Remitigate Therapeutics, Delmar NY Disclosures Affiliation Role/Activities Abbott Laboratories Speaking, non-speakers bureau AcelRx Pharmaceuticals Acute perioperative pain (speakers bureau, consulting, advisory boards) BioDelivery Sciences International Collaborative publications, consulting, advisory boards Firstox Laboratories Micro serum testing for substances of abuse (consulting) GlaxoSmithKline (GSK) Collaborative non-paid poster presentations) Hisamitsu America Inc Advisory Board Hikma Pharmaceuticals Advisory Board Scilex Pharmaceuticals Collaborative non-paid publications Salix Pharmaceuticals Speakers bureau, consultant, advisory boards Torrent Pharmaceuticals Lecture, non-speakers bureau Learning Objectives At the completion of this activity, participants will be able to: 1. Explain opioid conversion and calculation strategies when developing a care plan for patients with chronic pain. 2. Assess patient-specific factors that warrant adjustment to an opioid regimen. 3. Identify important drug interactions that can affect opioid serum levels. 4. Describe how pharmacogenetic differences can affect opioid efficacy, toxicity, and tolerability. Not All Opioids are Created Equally Issues with MEDD & Opioid Conversion1-4 › Pharmacogenetic variability › Drug interactions › Lack of universal morphine equivalence › Specific opioids that should never have an MEDD – Methadone, Buprenorphine, Tapentadol, Tramadol 1. Fudin J, Marcoux MD, Fudin JA. Mathematical Model For Methadone Conversion Examined. Practical Pain Management. Sept. 2012. 46-51. 2. Donner B, et al. -

Analysis of Oxycodone and Its Metabolites-Noroxycodone, Oxymorphone, and Noroxymorphone in Plasma by LC/MS with an Agilent ZORBAX Stablebond SB -C18 LC Column
Analysis of Oxycodone and Its Metabolites-Noroxycodone, Oxymorphone, and Noroxymorphone in Plasma by LC/MS with an Agilent ZORBAX StableBond SB -C18 LC Column Application Note Pharmaceutical Authors Abstract Linda L. Risler Oxycodone and its oxidative metabolites (noroxycodone, oxymorphone, and Fred Hutchinson Cancer Research noroxymorphone) were analyzed by high performance liquid chromatography/mass Center, spectrometry (HPLC/MS), coupled with chromatographic separation by an Agilent Seattle, WA 98109 ZORBAX Rapid Resolution High Throughput (RRHT) StableBond SB-C18 column. The method used an ammonium acetate/acetonitrile gradient with detection by a mass Anne E. Mack spectrometer in electrospray mode with positive polarity. Spiked human plasma Agilent Technologies, Inc. samples underwent solid phase extraction (SPE) prior to LC/MS analysis. This method provided good linearity (R 2 > 0.9900) and reproducibility (< 10% difference between duplicates) for all compounds, while increasing productivity with a fast, efficient analysis and minimal solvent usage. Introduction Experimental Oxycodone was developed in 1916 as an opioid analgesic An Agilent 1100 Series LC/MS was used for this work: medication intended to replace the far too addictive analgesic at the time, heroin. Today, oxycodone is a Schedule II drug in • Agilent G1312A Binary Pump. Mobile phase A: 20 mM the US, which means, while it has proven medical uses, it is ammonium acetate, pH 4.0 and B: acetonitrile. Flow rate still considered highly addictive with the possibility of both was 0.300 mL/min. Hold 5% B for 2.33 minutes, then physical and psychological dependencies. Figure 1 shows increase B from 5% to 20% from 2.33 to 4.33 minutes, stop oxycodone and its metabolic scheme, yielding noroxycodone, time is 6 minutes, and post time is 4 minutes. -
Presentation Slides (PDF)
Urine toxicology testing to support pain management and treatment for substance use disorder Yifei Yang, PhD, DABCC Medical Director, Toxicology, ARUP Laboratories Assistant Professor, University of Utah Learning Objectives and Presentation Outline • Describe the general analytical workflow of urine drug testing • Understand the testing approaches for medication compliance in pain management and treatment for substance use disorder (SUD) settings • Recognize the utilities and limitations of qualitative and quantitative test results • Discuss case-based unexpected urine drug testing results and considerations for results interpretation Urine toxicology testing to support controlled substance prescription and monitoring • Pain management and SUD treatment • Long-term prescription of controlled substances • Various opiates: hydrocodone, oxycodone, etc. at various doses • Buprenorphine, with naloxone (Suboxone) • Co-medication with benzodiazepines, heroin, and other opiates can increase risk for over-dose • Urine toxicology testing is recommended: • Baseline testing prior to prescription • Annual monitoring (minimal), interval up to clinician discretion • Detect undisclosed medication use • Confirm expected medication use CDC Guideline for Prescribing Opioids for Chronic Pain. (2016) Centers for Disease Control and Prevention. Urine toxicology testing is used to confirm the presence of prescribed medications • Drug presence prevalence: • High positivity rate • Patients are mostly taking medications • Appropriate positive cutoffs are needed -

Drug Plasma Half-Life and Urine Detection Window | January 2019
500 Chipeta Way | Salt Lake City, UT 84108-1221 Phone: (800) 522-2787 | Fax: (801) 583-2712 www.aruplab.com | www.arupconsult.com DRUG PLASMA HALF-LIFE AND URINE DETECTION WINDOW | JANUARY 2019 URINE- PLASMA DRUG, DRUG METABOLITE(S)* COMMON TRADE AND STREET NAMES, NOTES DETECTION HALF-LIFEt WINDOWt STIMULANTS Benzedrine, dexedrine, Adderall, Vyvanse, speed; could be methamphetamine Amphetamine 7–34 hours 1–5 days metabolite; if so, typically < 30 percent of parent Cocaine Coke, crack; parent drug rarely observed due to short half-life 0.7–1.5 hours < 1 day Benzoylecgonine Cocaine metabolite 5.5–7.5 hours 1–2 days Desoxyn, methedrine, Vicks inhaler (D- and L-isomers not resolved; low concentrations Methamphetamine expected if the source is Vicks); selegeline (Atapryl, Carbex, Eldepryl, Zelapar) 6–17 hours 1–5 days metabolite Methylenedioxyamphetamine (MDA) MDA 11–17 hours 1–3 days Methylenedioxyethylamphetamine (MDEA) MDEA, MDE, Eve 6–11 hours 1–3 days Methylenedioxymethamphetamine (MDMA) MDMA, XTC, ecstasy, Molly 6–10 hours 1–3 days Methylphenidate Ritalin, Concerta, Focalin, Metadate, Methylin 1.4–4.2 hours < 1 day Ritalinic acid Methylphenidate metabolite 1.8–2.5 hours < 1 day Phentermine Adipex-P, Lomaira, Qsymia 19–24 hours 1–5 days OPIOIDS Buprenorphine Belbuca, Buprenex, Butrans, Suboxone, Subutex, Sublocade, Zubsolv 26–42 hours 1–7 days Norbuprenorphine, Glucuronides Buprenorphine metabolites 15–150 hours 1–14 days Included in many preparations; morphine metabolite; may be a contaminant if < 2 Codeine 1.9–3.9 hours 1–3 days percent of morphine Fentanyl Actiq, Duragesic, Fentora, Lazanda, Sublimaze, Subsys, Ionsys 3–12 hours 1–3 days Norfentanyl Fentanyl metabolite 9–10 hours 1–3 days Heroin Diacetylmorphine, dope, smack, dust; parent drug not detected. -

NIDA Drug Supply Program Catalog, 25Th Edition
RESEARCH RESOURCES DRUG SUPPLY PROGRAM CATALOG 25TH EDITION MAY 2016 CHEMISTRY AND PHARMACEUTICS BRANCH DIVISION OF THERAPEUTICS AND MEDICAL CONSEQUENCES NATIONAL INSTITUTE ON DRUG ABUSE NATIONAL INSTITUTES OF HEALTH DEPARTMENT OF HEALTH AND HUMAN SERVICES 6001 EXECUTIVE BOULEVARD ROCKVILLE, MARYLAND 20852 160524 On the cover: CPK rendering of nalfurafine. TABLE OF CONTENTS A. Introduction ................................................................................................1 B. NIDA Drug Supply Program (DSP) Ordering Guidelines ..........................3 C. Drug Request Checklist .............................................................................8 D. Sample DEA Order Form 222 ....................................................................9 E. Supply & Analysis of Standard Solutions of Δ9-THC ..............................10 F. Alternate Sources for Peptides ...............................................................11 G. Instructions for Analytical Services .........................................................12 H. X-Ray Diffraction Analysis of Compounds .............................................13 I. Nicotine Research Cigarettes Drug Supply Program .............................16 J. Ordering Guidelines for Nicotine Research Cigarettes (NRCs)..............18 K. Ordering Guidelines for Marijuana and Marijuana Cigarettes ................21 L. Important Addresses, Telephone & Fax Numbers ..................................24 M. Available Drugs, Compounds, and Dosage Forms ..............................25 -
Prediction of Drug Interactions with Methadone, Buprenorphine and Oxycodone from in Vitro Inhibition of Metabolism
The author(s) shown below used Federal funds provided by the U.S. Department of Justice and prepared the following final report: Document Title: Prediction of Drug Interactions with Methadone, Buprenorphine and Oxycodone from In Vitro Inhibition of Metabolism Author(s): David E. Moody, Ph.D. Document No.: 250127 Date Received: July 2016 Award Number: 2011-DN-BX-K532 This report has not been published by the U.S. Department of Justice. To provide better customer service, NCJRS has made this federally funded grant report available electronically. Opinions or points of view expressed are those of the author(s) and do not necessarily reflect the official position or policies of the U.S. Department of Justice. February 2016 Research and Development in Forensic Toxicology Prediction of drug interactions with methadone, buprenorphine and oxycodone from in vitro inhibition of metabolism Final Technical Report Submitted electronically to: U.S. Department of Justice Office of Justice Programs National Institute of Justice Prepared by: David E. Moody. Ph.D. Director of the Center for Human Toxicology, and Research Professor of Pharmacology and Toxicology [email protected] / 801-581-5117 NIJ Award Number: 2011-DN-BX-K532 Reporting Period: January 1, 2012 to December 31, 2015 Recipient Organization: University of Utah 75 South 2000 East, Room 222 Salt Lake City, UT 84112-8930 Organizational DUNS: 0090953650000 EIN: 876000525 This document is a research report submitted to the U.S. Department of Justice. This report has not been published by the Department. Opinions or points of view expressed are those of the author(s) and do not necessarily reflect the official position or policies of the U.S. -
Interpretation of Drug Testing Results in Medication Assisted Treatment
Interpretation of Drug Testing Results in Medication Assisted Treatment By: Paul L. Cary Independent Forensic Toxicology Consultant What Does This Result Mean? Two-Step Testing Approach ■ screening test – designed to separate negative samples from samples that are “presumptively” positive ■ confirmation test – follow-up procedure designed to validate positive test results ■ why can’t you adjudicate based on the screening test results? ■ FALSE POSITIVES Drug tests & cross reactivity: ■ screening tests can and do react to “non-target” compounds ◆ amphetamines ◆ benzodiazepines ■ obtain list of interfering compounds from lab or on-site test vendor ■ study results have demonstrated accuracy rates for initial screening tests as low as 70% ■ confirm positive results Typical Cutoff Levels screening & confirmation ■ amphetamines * 500 ng/mL 250 ng/mL ■ benzodiazepines 300 ng/mL variable ■ cannabinoids * 20 & 50 ng/mL 15 ng/mL ■ cocaine (crack)* 150 ng/mL 100 ng/mL ■ opiates (heroin) * 300/2000 ng/mL variable ■ phencyclidine (PCP) * 25 ng/mL 25 ng/mL ■ alcohol 20 mg/dL 10 mg/dL ◆ * SAMHSA (formerly NIDA) drugs What is a “cutoff” level ? ■ cutoffs are not designed to frustrate CJ professionals ■ a drug concentration, administratively established for a drug test that allows the test to distinguish between negative and positive sample - “threshold” ■ cutoffs provide important safeguards: ◆ scientific purposes (detection accuracy) ◆ legal protections (evidentiary admissibility) ■ measured in ng/mL = ppb Cutoffs and False Positives as you lower you -

Review Memorandum
510(k) SUBSTANTIAL EQUIVALENCE DETERMINATION DECISION SUMMARY ASSAY AND INSTRUMENT COMBINATION TEMPLATE A. 510(k) Number: K130082 B. Purpose for Submission: New Device C. Measurand: Amphetamine, Barbiturates, Cocaine, Marijuana, Methadone, Methamphetamine, Morphine, Oxycodone, Phencyclidine D. Type of Test: Qualitative immunochromatographic tests for drugs of abuse in urine E. Applicant: GenPrime Inc. F. Proprietary and Established Names: The GenPrime Drugs of Abuse (DOA) Reader System G. Regulatory Information: 1. Regulation section: 21 CFR §862.3100, Amphetamine Test System 21 CFR §862.3150, Barbiturate Test System 21 CFR §862.3250, Cocaine and cocaine metabolite Test System 21 CFR §862.3870, Cannabinoid Test System 21 CFR §862.3620, Methadone Test System 21 CFR §862.3610, Methamphetamine Test System 21 CFR §862.3640, Morphine test system 21 CFR §862.3650, Opiate Test System Phencyclidine, Unclassified 21 CFR §862.2400, Densitometer/Scanner (integrating, reflectance, TLC, or radiochromatogram) for clinical use 2. Classification: Class II – for all except Phencyclidine and the Densitometer/Scanner Phencyclidine – Unclassified Densitometer/Scanner – Class I 3. Product code: DKZ, DIS, DIO, LDJ, DJR, DJC, DJG, LCM, DNK, JQT 4. Panel: Clinical Toxicology (91) and Clinical Chemistry (75) H. Intended Use: 1. Intended use(s): See Indications for Use below. 2. Indication(s) for use: The GenPrime Drugs of Abuse (DOA) Reader System consists of the GenPrime DOA Reader, GenPrime DOA Windows®-compatible Software and compatible qualitative immunochromatographic, OS Cup and Split Key Cup (SK Cup) test devices. The GenPrime DOA Reader System is for in vitro diagnostic use and is intended for prescription use in laboratories, point-of-care, and workplaces by trained users. -

Number: K040257 B. Analyte: THC An
510(k) SUBSTANTIAL EQUIVALENCE DETERMINATION DECISION SUMMARY DEVICE ONLY TEMPLATE A. 510(k) Number: k040257 B. Analyte: THC and carboxy-THC C. Type of Test: Qualitative screening test: immunoassay Quantitative confirmatory test: GC-MS-MS D. Applicant: Quest Diagnostics, Inc. E. Proprietary and Established Names: Quest Diagnostics Haircheck-DT (THC) F. Regulatory Information: 1. Regulation section: 21 CFR § 862.3870 2. Classification: II 3. Product Code: LDJ 4. Panel: Toxicology (91) G. Intended Use: 1. Intended use(s): Refer to Indications for use. 2. Indication(s) for use: The Quest Diagnostics HairCheck-DT (THC-COOH) is a bipartite device employing enzyme-linked immunosorbent assay (ELISA) for qualitative screening at 1.0 pg/mg hair of THC-COOH and Gas Chromatography – Mass Spectroscopy – Mass Spectroscopy (GC-MS-MS) for confirmation and the final quantitative reporting of THC-COOH in human hair samples for the purpose of identifying chronic marijuana use. This process has not been evaluated with hair specimens other than head. This process is intended exclusively for in-house professional use only. The process is not intended for sale to anyone. Clinical consideration and professional judgement should be applied to any drug of abuse test result. Page 2 of 16 The device is for in vitro diagnostic use. The device is for prescription use only. 3. Special condition for use statement(s): The Quest Diagnostics HairCheck-DT (THC-COOH) combines a screening method (immunoassay) with a confirmation method (GC-MS-MS) in one test system. A negative screening result is reported as negative. A presumptive positive screening result is not reported until it has been confirmed by GC- MS-MS. -

Federal Register/Vol. 85, No. 230/Monday, November 30, 2020
76604 Federal Register / Vol. 85, No. 230 / Monday, November 30, 2020 / Notices notifications disclosing all changes in Act on September 18, 2020 (85 FR DEPARTMENT OF JUSTICE membership. 58390). Drug Enforcement Administration On September 10, 2018, CONFERS Suzanne Morris, [Docket No. DEA–688E] filed its original notification pursuant to Chief, Premerger and Division Statistics, Section 6(a) of the Act. The Department Antitrust Division. Established Aggregate Production of Justice published a notice in the [FR Doc. 2020–26362 Filed 11–27–20; 8:45 am] Federal Register pursuant to Section Quotas for Schedule I and II Controlled BILLING CODE P Substances and Assessment of 6(b) of the Act on October 19, 2018 (83 Annual Needs for the List I Chemicals FR 53106). Ephedrine, Pseudoephedrine, and The last notification was filed with DEPARTMENT OF JUSTICE Phenylpropanolamine for 2021 the Department on May 1, 2020. A notice was published in the Federal Antitrust Division AGENCY: Drug Enforcement Register pursuant to Section 6(b) of the Administration, Department of Justice. Act on May 28, 2020 (85 FR 32049). Notice Pursuant to the National ACTION: Final order. Cooperative Research and Production Suzanne Morris, Act of 1993—Cooperative Research SUMMARY: This final order establishes Chief, Premerger and Division Statistics, Group on AC2AT–II the initial 2021 aggregate production Antitrust Division. quotas for controlled substances in [FR Doc. 2020–26358 Filed 11–27–20; 8:45 am] Notice is hereby given that, on schedules I and II of the Controlled Substances Act and the assessment of BILLING CODE 4410–11–P November 19, 2020, pursuant to Section 6(a) of the National Cooperative annual needs for the list I chemicals Research and Production Act of 1993, ephedrine, pseudoephedrine, and DEPARTMENT OF JUSTICE 15 U.S.C. -
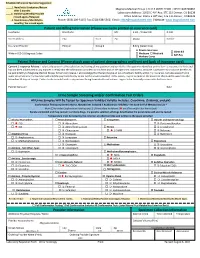
Patient and Billing Information (Please Use Name Printed on Insurance Card) Last Name First Name M.I
Schedule Adherence Specialist Suggestion: 1. New/Initial Evaluation/Return Magnolia Medical Group | CLIA # 06D2121590 | NPI# 1043769862 after 2 months. th 2. Stabilizing/Weekly/Possible Laboratory Address: 10515 E 40 Ave, STE 115 Denver, CO 80239 th missed appts./Relapsed Office Address: 10515 E 40 Ave, STE 115 Denver, CO80239 3. Maintenance/Monthly/2x Phone: (303) 209-5115| Fax: (720) 638-5562| Email: [email protected] | Website: www.magnoliamed.com monthly/ No missed appts. Patient and Billing Information (Please use name printed on insurance card) Last Name First Name M.I. S.S.N. / Patient ID D.O.B. Street Address City State Zip Phone Gender Insurance Provider Policy # Group # Billing (Select One) Private Insurance Client Bill Write in ICD-10 Diagnosis Codes Medicare Medicaid Self-Pay Workers Comp Patient Release and Consent (Please attach copy of patient demographics and front and back of insurance card) Consent / Insurance Release: I voluntarily consent to the collection and testing of my specimen and certify that the specimen identified on this form is my own; it is fresh and has not been adulterated in any manner. I certify that the information provided on this form and on the specimen container is accurate. I authorize my insurance benefits to be paid directly to Magnolia Medical Group, for service I receive. I acknowledge that the lab may be an out-of-network facility within my insurance. I am also aware that in some circumstances my insurance will send the payment directly to me for the service provided. If this occurs, I agree to endorse the insurance check and forward it to the lab within 30 days of receipt. -

Pharmacopoeial Reference Standards and Their Current Lot Numbers EP, EPISA, ICRS, USP, BP December 2016
Pharmacopoeial reference standards and their current lot numbers EP, EPISA, ICRS, USP, BP December 2016 New: LGCon Standards LinkedIn Pharma Dear user, This catalogue includes all pharmacopoeial reference materials from EP, EPISA, ICRS, USP and BP available at LGC, as well as their current lot numbers. We update the catalogue on a monthly basis so that you can use the lot numbers to easily track the expiry dates of your stocked reference materials. We took the lot information from actual data from the Pharmacopoeias and correct at the time of production. We retained all spelling and information as provided by the Pharmacopoeias. The list was compiled with caution, however errors in this list may be possible, and LGC is not responsible for any consequences as a result of these errors, may it be errors in the original Pharmacopoeia data, or from LGC during compilation of this list. For any questions or orders please contact your local LGC office. You will find all contact details on the last page of this list. Alternatively, you can browse and buy pharmaceutical reference materials online at www.lgcstandards.com. Stay connected via LinkedIn (LGC Standards Pharma) or Twitter @LGCStdsPharma Kind regards Your LGC Standards Team LGC, Queens Road, Teddington, Middlesex, TW11 0LY, United Kingdom Tel.: +44 (0)20 8943 8480, Fax: +44 (0)20 8943 7554 E-Mail: [email protected] European Pharmacopoeia (EP) Available Current Unit Cat. No. Name What is new? since Batch No. Quantity 24.10.2016 EPY0001912 Erythromycin A 4 250 mg New batch! EPY0001561