No Correlation Between Positive Fructose Hydrogen Breath Test And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Prevalence of Fructose Malabsorption in Patients with Irritable Bowel Syndrome After Excluding Small Intestinal Bacterial Overgrowth
J Neurogastroenterol Motil, Vol. 24 No. 2 April, 2018 pISSN: 2093-0879 eISSN: 2093-0887 https://doi.org/10.5056/jnm17044 JNM Journal of Neurogastroenterology and Motility Original Article Prevalence of Fructose Malabsorption in Patients With Irritable Bowel Syndrome After Excluding Small Intestinal Bacterial Overgrowth Kee Wook Jung,1 Myeognsook Seo,1 Young Hwan Cho,1 Young-Ok Park,2 So-Yoon Yoon,2 Jungbok Lee,3 Dong-Hoon Yang,1 In Ja Yoon,1 So Young Seo,1 Hyo Jeong Lee,1 Sang Hyoung Park,1 Kyung Jo Kim,1 Byong Duk Ye,1 Jeong-Sik Byeon,1 Hwoon-Yong Jung,1 Suk-Kyun Yang,1 Jin-Ho Kim,1 and Seung-Jae Myung1* Departments of 1Gastroenterology, 2Clinical Nutrition, and 3Clinical Epidemiology and Biostatistics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea Background/Aims Fructose malabsorption (FM) mimics symptoms of irritable bowel syndrome (IBS), and its prevalence has increased. Diagnosing FM in IBS is challenging because of its overlap with small intestinal bacterial overgrowth (SIBO). We assessed the prevalence of FM by comparing patients with IBS with asymptomatic control individuals after excluding SIBO using the glucose hydrogen breath test (HBT). Methods Patients diagnosed with IBS and asymptomatic control individuals were enrolled prospectively. Dietary habits were assessed with the Food Frequency Questionnaire. After excluding SIBO, participants underwent HBTs with both 15 g and 25 g of fructose. Results Thirty-five patients with IBS and 35 age- and sex-matched asymptomatic control individuals were enrolled. The 15-g fructose HBT yielded positive results in 7 of the 35 (20.0%) patients with IBS and in 2 of 35 (5.7%) controls (P = 0.070). -

Limiting Fructose, Fructans Intake May Ease IBS
36 Digestive Disorders FAMILY P RACTICE N EWS • July 1, 2008 Limiting Fructose, Fructans Intake May Ease IBS BY MARY ANN MOON “marked and sustained global improve- of irritable bowel syndrome (IBS) in patients prove symptoms. In the current study, the Contributing Writer ment in gastrointestinal symptoms,” re- who also have fructose malabsorption. researchers focused on osmotic load with- searchers noted. A subsequent study of The results also demonstrate that re- in the lumen and fermentative gas content. atients with irritable bowel syn- the patients revealed that symptom relief stricting intake of these substances may Poorly absorbed short-chain carbohy- drome and fructose malabsorption was not specific to restricted intake of lead to durable symptomatic improve- drates, including fructose and lactose, are Pappeared to benefit from a diet that fructose, but was achieved by limiting the ment, wrote Ms. Shepherd, a dietician at highly fermentable. They exert a strong restricted intake of fructose and fructans, intake of poorly absorbed short-chain Australia’s Monash University, Clayton, osmotic effect in people who have malab- Susan J. Shepherd and her colleagues re- carbohydrates. Victoria, and her colleagues. sorption of these two sugars—about 40% ported in an article appearing in the July These findings “represent the first high- They theorized that, because many ab- of the population in the case of fructose, 2008 issue of Clinical Gastroenterology level evidence” that poorly absorbed short- dominal symptoms may originate from and between 15% to 100% of the popula- and Hepatology. chain carbohydrates—fructose and fruc- bowel distension, addressing factors that tion for lactose. In the 25-patient study, the diet led to tans—are dietary triggers for the symptoms contribute to the distension would im- To minimize or eliminate intake of poor- ly absorbed short-chain carbohydrates, the investigators created a diet that omitted Brief Summary—see package insert for full prescribing information. -

2.04.26 Fecal Analysis in the Diagnosis of Intestinal Dysbiosis and Irritable Bowel Syndrome
MEDICAL POLICY – 2.04.26 Fecal Analysis in the Diagnosis of Intestinal Dysbiosis and Irritable Bowel Syndrome BCBSA Ref. Policy: 2.04.26 Effective Date: July 1, 2021 RELATED MEDICAL POLICIES: Last Revised: June 8, 2021 None Replaces: N/A Select a hyperlink below to be directed to that section. POLICY CRITERIA | DOCUMENTATION REQUIREMENTS | CODING RELATED INFORMATION | EVIDENCE REVIEW | REFERENCES | HISTORY ∞ Clicking this icon returns you to the hyperlinks menu above. Introduction Intestinal dysbiosis is a condition that occurs when the microorganisms in the digestive tract are out of balance. This condition is believed to cause diseases of the digestive tract, including poor nutrient absorption, overgrowth of certain bacteria, and irritable bowel syndrome (IBS). Symptoms of these digestive problems are similar and may include: abdominal pain, excess gas, bloating, and changes in bowel movements (constipation or diarrhea, or both). One method of diagnosing digestive disorders is by testing a fecal sample. Using fecal analysis to diagnose intestinal dysbiosis, IBS, malabsorption, or small intestinal overgrowth of bacteria is unproven (investigational). More studies are needed to see if this testing improves health outcomes. Note: The Introduction section is for your general knowledge and is not to be taken as policy coverage criteria. The rest of the policy uses specific words and concepts familiar to medical professionals. It is intended for providers. A provider can be a person, such as a doctor, nurse, psychologist, or dentist. A provider also can be a place where medical care is given, like a hospital, clinic, or lab. This policy informs them about when a service may be covered. -

An Osteopathic Approach to Reduction of Readmissions for Neonatal Jaundice
Osteopathic Family Physician (2013) 5, 17–23 REVIEW ARTICLE An osteopathic approach to reduction of readmissions for neonatal jaundice Rachel Click, DO,a Julie Dahl-Smith, DO,a Lindsay Fowler, DO,a Jacqueline DuBose, MD,a Margi Deneau-Saxton, RN, CCCE, CIMI, CLC, CPD,b Jennifer Herbert, MDc From aGeorgia Health Sciences University, Medical College of Georgia, Department of Family Medicine, GA; bGeorgia Health System, OB Labor and Delivery, GA; and cUniversity Primary Care, Evans, GA. KEYWORDS: Jaundice is a potentially life-threatening condition that continues to affect at-risk newborns, accounting Breastfeeding; for continued hospital readmissions. As family physicians, we should be cognizant of neonates who may Jaundice; be at risk for jaundice, including those with pathologic jaundice as well as newborns of breastfeeding Prevention; mothers, and ensure sufficient intervention is taken to help prevent further elevations in bilirubin levels. Hyperbilirubinemia; Interventions are likely to include evaluation for sepsis, education regarding feeding frequencies for both Neonatal massage breast- and bottle-fed neonates, reviewing maternal and hematologic risk factors for neonatal jaundice, and considering inborn errors of metabolism. An additional measure family physicians may consider is that of neonatal massage for those with elevated bilirubin levels. Neonatal massage, though not widely used, has been proven to promote excess bilirubin excretion, thus decreasing length of hospital stay; all the while, providing an intervention that allows parents to take an active role. r 2013 Elsevier Inc. All rights reserved. Introduction morbidity rate with bilirubin 4 20 mg/dL. “It has been estimated that the risk of kernicterus in infants with total Jaundice is a product of excess bilirubin (a product of serum bilirubin (TSB) greater than 30 mg/dL is about 1 in broken down red blood cells), which manifests as a 7 infants”.1 Less serious complications of hyperbilirubine- yellowing of the skin and eyes. -

INFORMED CARING JAUNDICE Neonatal Jaundice BILIARY
1 INFORMED CARING Situations with Adults and Children with Gallbladder, Liver and Pancreatic Disorders 2 JAUNDICE ä Does NOT mean hepatitis ä Increased breakdown of RBCs ä Altered bilirubin breakdown ä Impeded flow through liver or bile duct ä First seen in sclera, then skin 3 Neonatal Jaundice ä Not liver failure ä RBC breakdown ä Phototherapy 4 BILIARY ATRESIA ä Jaundice 2-3 weeks after birth ä Easy bruising ä Stools putty like ä Tea colored urine ä Abdominal/organ distension 5 4 F’s of Gallbladder ä Fair ä Fat X size of person X amount in diet ä Fertile X BCP X Multiparity ä Forty 6 Cholelithiasis ä Calculi within the duct or gallbladder ä Severe colicky, cramp-like pain X radiates to shoulder blade X Murphy's sign ä Cholecystitis: inflammation X Can be caused by trauma, fasting, TPN or abdominal surgery 7 Diagnostic Studies ä Ultrasound of abdomen 1 X not for the obese ä HIDA scan X nuclear medicine ä Cholangiograms X endoscopic X transvenous X intraoperative 8 Post-op Care ä High abdominal incision X respiratory compromise ä T-tube X patients need to know how to empty it X may clamp it prior to removal X caution not dislodged with movements ä NO Morphine X spasms of sphincter of Oddi 9 Post-op Nutrition ä Limited fat in diet X can have rapid transit times ä Potential fat soluble vitamin deficit X A, D, E and K ä Weight loss diet 10 LIVER FAILURE ä Cirrhosis ä Drug toxicity X acetaminophen, anesthetics, HCTZ, chemotherapy ä Infection ä Cancer ä ETOH is single most linked cause 11 LIVER FAILURE S/S ä Don’t show up until 80-90% failed -

Symptomatic Approach to Gas, Belching and Bloating 21
20 Osteopathic Family Physician (2019) 20 - 25 Osteopathic Family Physician | Volume 11, No. 2 | March/April, 2019 Gennaro, Larsen Symptomatic Approach to Gas, Belching and Bloating 21 Review ARTICLE to escape. This mechanism prevents the stomach from becoming IRRITABLE BOWEL SYNDROME (IBS) Symptomatic Approach to Gas, Belching and Bloating damaged by excessive dilation.2 IBS is abdominal pain or discomfort associated with altered with OMT Treatment Options Many patients with GERD report increased belching. Transient bowel habits. It is the most commonly diagnosed GI disorder lower esophageal sphincter (LES) relaxation is the major and accounts for about 30% of all GI referrals.7 Criteria for IBS is recurrent abdominal pain at least one day per week in the Carly Gennaro, DO1; Helaine Larsen, DO1 mechanism for both belching and GERD. Recent studies have shown that the number of belches is related to the number of last three months associated with at least two of the following: times someone swallows air. These studies have concluded that 1) association with defecation, 2) change in stool frequency, 1 Good Samaritan Hospital Medical Center, West Islip, NY patients with GERD swallow more air in response to heartburn and 3) change in stool form. Diagnosis should be made using these therefore belch more frequently.3 There is no specific treatment clinical criteria and limited testing. Common symptoms are for belching in GERD patients, so for now, physicians continue to abdominal pain, bloating, alternating diarrhea and constipation, treat GERD with proton pump inhibitors (PPIs) and histamine-2 and pain relief after defecation. Pain can be present anywhere receptor antagonists with the goal of suppressing heartburn and in the abdomen, but the lower abdomen is the most common KEYWORDS: ABSTRACT: Intestinal gas production is a normal physiologic progress. -
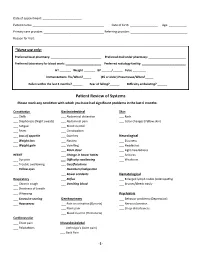
Patient Review of Systems Please Mark Any Condition with Which You Have Had Significant Problems in the Last 6 Months
Date of appointment: ________________________ Patient name: ____________________________________________ Date of birth: _________________ Age: ___________ Primary care provider: _____________________________________ Referring provider: ___________________________________ Reason for Visit: _____________________________________________________________________________________________ *Nurse use only: Preferred local pharmacy: _______________________________ Preferred mail order pharmacy: _______________________ Preferred laboratory for blood work: ______________________ Preferred radiology facility: ___________________________ HT _______ Weight _______ BP ______/______ Pulse ________ Immunizations: Flu/When?_____ (65 or older) Pneumovax/When?_____ Fallen within the last 3 months? ______ Fear of falling?______ Difficulty ambulating? ______ Patient Review of Systems Please mark any condition with which you have had significant problems in the last 6 months: Constitution Gastrointestinal Skin ___ Chills ___ Abdominal distention ___ Rash ___ Diaphoresis (Night sweats) ___ Abdominal pain ___ Color changes (Yellow skin) ___ Fatigue ___ Blood in stool ___ Fever ___ Constipation ___ Loss of appetite ___ Diarrhea Neurological ___ Weight loss ___ Nausea ___ Dizziness ___ Weight gain ___ Vomiting ___ Headaches ___ Black stool ___ Light-headedness HEENT ___ Change in bowel habits ___ Seizures ___ Eye pain ___ Difficulty swallowing ___ Weakness ___ Trouble swallowing ___ Gas/flatulence ___ Yellow eyes ___ Heartburn/indigestion ___ Bowel accidents Hematological -

Chrebp-Knockout Mice Show Sucrose Intolerance and Fructose Malabsorption
nutrients Article ChREBP-Knockout Mice Show Sucrose Intolerance and Fructose Malabsorption Takehiro Kato 1, Katsumi Iizuka 1,2,* ID , Ken Takao 1, Yukio Horikawa 1, Tadahiro Kitamura 3 and Jun Takeda 1 1 Department of Diabetes and Endocrinology, Graduate School of Medicine, Gifu University, Gifu 501-1194, Japan; [email protected] (T.K.); [email protected] (K.T.); [email protected] (Y.H.); [email protected] (J.T.) 2 Gifu University Hospital Center for Nutritional Support and Infection Control, Gifu 501-1194, Japan 3 Metabolic Signal Research Center, Institute for Molecular and Cellular Regulation, Gunma University, Gunma 371-8512, Japan; [email protected] * Correspondence: [email protected]; Tel.: +81-58-230-6564; Fax: +81-58-230-6376 Received: 31 January 2018; Accepted: 9 March 2018; Published: 10 March 2018 Abstract: We have previously reported that 60% sucrose diet-fed ChREBP knockout mice (KO) showed body weight loss resulting in lethality. We aimed to elucidate whether sucrose and fructose metabolism are impaired in KO. Wild-type mice (WT) and KO were fed a diet containing 30% sucrose with/without 0.08% miglitol, an α-glucosidase inhibitor, and these effects on phenotypes were tested. Furthermore, we compared metabolic changes of oral and peritoneal fructose injection. A thirty percent sucrose diet feeding did not affect phenotypes in KO. However, miglitol induced lethality in 30% sucrose-fed KO. Thirty percent sucrose plus miglitol diet-fed KO showed increased cecal contents, increased fecal lactate contents, increased growth of lactobacillales and Bifidobacterium and decreased growth of clostridium cluster XIVa. -

Fructose Malabsorption in Patients with Irritable Bowel Syndrome-Like Symptoms: What Is the Role in the Pathogenesis and Clinical Implication?
J Neurogastroenterol Motil, Vol. 20 No. 2 April, 2014 pISSN: 2093-0879 eISSN: 2093-0887 http://dx.doi.org/10.5056/jnm.2014.20.2.135 JNM Journal of Neurogastroenterology and Motility Editorial Fructose Malabsorption in Patients With Irritable Bowel Syndrome-like Symptoms: What Is the Role in the Pathogenesis and Clinical Implication? Hye-Young Sung and Yong Sung Kim* Division of Gastroenterology, Department of Internal Medicine, Digestive Disease Research Institute, Wonkwang University Sanbon Hospital, Gunpo-si, Gyeonggi-do, Korea Article: Unclear abdominal discomfort: pivotal role of carbohydrate malabsorption Goebel-Stengel M, Stengel A, Schmidtmann M, van der Voort I, Kobelt P, Mönnikes H. (J Neurogastroenterol Motil 2014;20:228-235) Abdominal discomfort with negative medical tests is a com- respectively. Although this was an observational study in a single mon presentation in the gastrointestinal (GI) clinic, and it is usu- center and not an interventional study, the number of enrolled pa- ally diagnosed as irritable bowel syndrome (IBS). However, car- tients was 2,390, making this the largest patient population study bohydrate malabsorption, especially fructose malabsorption (FM), to date.4 has been reported as another cause of unexplained abdominal However, this result could not be applied directly to IBS be- symptoms, and also suggested to have a role in the pathogenesis cause the patients in this study were not exactly diagnosed and of IBS. It has been reported that dietary fructose restriction and a classified by Rome criteria, but simply described as “patients with low fermentable oligosaccharides, disaccharides, monosaccha- IBS-like symptoms.” Even so, the results from this study suggest rides and polyols (FODMAPs) diet effectively reduced GI that the prevalence of FM is high in patients with unexplained symptoms in patients with IBS, suggesting that these restrictions abdominal symptoms, making this an important etiology in func- should be considered as a front-line therapy.1,2 tional GI disorders (FGID) like IBS. -

Fructose Malabsorption: Causes, Diagnosis and Treatment
Downloaded from British Journal of Nutrition, page 1 of 9 doi:10.1017/S0007114521001215 https://www.cambridge.org/core © The Author(s), 2021. Published by Cambridge University Press on behalf of The Nutrition Society. This is an Open Access article, distributed under the terms of the Creative Commons Attribution licence (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted re-use, distribution, and reproduction in any medium, provided the original work is properly cited. Fructose malabsorption: causes, diagnosis and treatment . IP address: Miles Benardout1*, Adam Le Gresley1, Amr ElShaer2 and Stephen P. Wren1* 1Department of Chemical and Pharmaceutical Sciences, Faculty of Science, Engineering and Computing, Kingston University London, Penryhn Road, Surrey KT12EE, UK 170.106.35.229 2Department of Pharmacy, Faculty of Science, Engineering and Computing, Kingston University London, Penryhn Road, Surrey KT12EE, UK (Submitted 14 October 2020 – Final revision received 19 February 2021 – Accepted 28 March 2021) , on 25 Sep 2021 at 13:47:17 Abstract This review intends to act as an overview of fructose malabsorption (FM) and its role in the aetiology of diseases including, but not limited to, irritable bowel syndrome (IBS) and infantile colic and the relationship between fructose absorption and the propagation of some cancers. IBS results in a variety of symptoms including stomach pains, cramps and bloating. Patients can be categorised into two groups, depending on whether the patients’ experiences either constipation (IBS-C) or diarrhoea (IBS-D). FM has been proposed as a potential cause of IBS-D , subject to the Cambridge Core terms of use, available at and other diseases, such as infantile colic. -

Traveller's Diarrhoea (TD) Is the Commonest Health
Diarrhoea • THEME Traveller's diarrhoea BACKGROUND There has been little if any Traveller's diarrhoea (TD) is the commonest health change in the incidence of traveller's diarrhoea problem facing travellers to less developed countries over the past 20 years. of the world. It is costly to both the traveller (time lost) and the host country (eg. cancelled activities). OBJECTIVE This article aims to provide a basic understanding on why travellers are more likely to Definition experience diarrhoea during travel. Classic TD is described as three or more loose bowel DISCUSSION In a 20 minute pretravel actions with at least one of the following accompanying consultation time is precious, and providing symptoms: nausea, vomiting, abdominal cramps or information on traveller's diarrhoea often has pain, fever or blood in the stools. Lesser degrees a low priority over prescribing the necessary vaccinations and discussing antimalarials. (moderate or mild) of TD are also described. Severity is Bob Kass, Travellers do not follow the rules of eating and usually defined by the number of bowel actions per 24 drinking safely, and diarrhoea is common. 'What hour period (severe >6). According to the World Health MBBS, MRCP (UK), MScMCH, Organisation, symptoms lasting less than 14 days may to do in the event of illness' is an important DCH, FAFPHM, consideration. Presumptive treatment should be defined as 'acute diarrhoea', and those lasting more is a consultant, be offered to all travellers whose itinerary and than 14 days 'persistent diarrhoea'.1 International Public activities put them at risk. Between 30 and 50% of travellers will be affected Health Medicine, Rede-Health in a 2 week overseas stay, with approximately 12% International. -

Low Fructose Diet
Low Fructose Diet What is Fructose? Fructose is a natural sugar found in fruit, fruit juices, honey, and agave syrup. It is also found in some vegetables and wheat products in another form called fructans (fructose sugars in a long chain). High fructose corn syrup (HFCS) is another form of fructose commonly used in processed foods. What is Fructose Intolerance? Fructose intolerance, also called dietary fructose intolerance or fructose malabsorption, happens when a person cannot properly absorb normal amounts of fructose (>25 grams per meal). What are common symptoms? Unabsorbed fructose that reaches the large intestine can be fermented (converted into gas) by bacteria causing symptoms like abdominal pain, gas, belching, and bloating. Unabsorbed fructose can also pull water back into the colon, increasing gut motility and causing diarrhea. Less common symptoms of fructose intolerance can include reflux, depression, fatigue, brain fog, headache, weight loss, and sugar cravings. How is Fructose Intolerance diagnosed? Anyone can develop fructose intolerance, but it is more common among individuals with irritable bowel syndrome (IBS) or other gastrointestinal disorders. A Hydrogen Breath Test is used to diagnosis fructose intolerance. An abnormal (positive) test indicates the need for a low fructose diet. What is a Low Fructose Diet? A low fructose diet reduces the amount of fructose consumed by limiting or avoiding foods with excess fructose (foods that contain more than half of their natural sugar as fructose), foods with high fructose (more than 3 grams), and foods that are a significant source of fructans (chains of fructose). How long does this diet need to be followed? A low fructose diet should be followed until symptoms improve, typically 2-6 weeks.