Standard of Care: Anorectal Disorders ICD 10 Codes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2.04.26 Fecal Analysis in the Diagnosis of Intestinal Dysbiosis and Irritable Bowel Syndrome
MEDICAL POLICY – 2.04.26 Fecal Analysis in the Diagnosis of Intestinal Dysbiosis and Irritable Bowel Syndrome BCBSA Ref. Policy: 2.04.26 Effective Date: July 1, 2021 RELATED MEDICAL POLICIES: Last Revised: June 8, 2021 None Replaces: N/A Select a hyperlink below to be directed to that section. POLICY CRITERIA | DOCUMENTATION REQUIREMENTS | CODING RELATED INFORMATION | EVIDENCE REVIEW | REFERENCES | HISTORY ∞ Clicking this icon returns you to the hyperlinks menu above. Introduction Intestinal dysbiosis is a condition that occurs when the microorganisms in the digestive tract are out of balance. This condition is believed to cause diseases of the digestive tract, including poor nutrient absorption, overgrowth of certain bacteria, and irritable bowel syndrome (IBS). Symptoms of these digestive problems are similar and may include: abdominal pain, excess gas, bloating, and changes in bowel movements (constipation or diarrhea, or both). One method of diagnosing digestive disorders is by testing a fecal sample. Using fecal analysis to diagnose intestinal dysbiosis, IBS, malabsorption, or small intestinal overgrowth of bacteria is unproven (investigational). More studies are needed to see if this testing improves health outcomes. Note: The Introduction section is for your general knowledge and is not to be taken as policy coverage criteria. The rest of the policy uses specific words and concepts familiar to medical professionals. It is intended for providers. A provider can be a person, such as a doctor, nurse, psychologist, or dentist. A provider also can be a place where medical care is given, like a hospital, clinic, or lab. This policy informs them about when a service may be covered. -

Anorectal Disorders Satish S
Gastroenterology 2016;150:1430–1442 Anorectal Disorders Satish S. C. Rao,1 Adil E. Bharucha,2 Giuseppe Chiarioni,3,4 Richelle Felt-Bersma,5 Charles Knowles,6 Allison Malcolm,7 and Arnold Wald8 1Division of Gastroenterology and Hepatology, Augusta University, Augusta, Georgia; 2Department of Gastroenterology and Hepatology, Mayo College of Medicine, Rochester, Minnesota; 3Division of Gastroenterology of the University of Verona, Azienda Ospedaliera Universitaria Integrata di Verona, Verona, Italy; 4Division of Gastroenterology and Hepatology and UNC Center for Functional GI and Motility Disorders, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina; 5Department of Gastroenterology/Hepatology, VU Medical Center, Amsterdam, The Netherlands; 6National Centre for Bowel Research and Surgical Innovation, Blizard Institute, Queen Mary University of London, London, United Kingdom; 7Division of Gastroenterology, Royal North Shore Hospital, and University of Sydney, Sydney, Australia; 8Division of Gastroenterology, University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin This report defines criteria and reviews the epidemiology, questionnaires and bowel diaries are correlated,5 some pathophysiology, and management of the following com- patients may not accurately recall bowel symptoms6; hence, mon anorectal disorders: fecal incontinence (FI), func- symptom diaries may be more reliable. tional anorectal pain, and functional defecation disorders. In this report, we examine the prevalence and patho- FI is defined as the recurrent uncontrolled passage of fecal physiology of anorectal disorders, listed in Table 1,and material for at least 3 months. The clinical features of FI provide recommendations for diagnostic evaluation and are useful for guiding diagnostic testing and therapy. management. These supplement practice guidelines rec- ANORECTAL Anorectal manometry and imaging are useful for evalu- ommended by the American Gastroenterological Associa- fl ating anal and pelvic oor structure and function. -

Overlap in Patient with Functional Dyspepsia and Unspecified Functional Anorectal Pain
Acta Interna The Journal of Internal Medicine Vol. 6 No. 2 December 2016 Website Journal : http://jurnal.ugm.ac.id/jain Overlap in Patient with Functional Dyspepsia and Unspecified Functional Anorectal Pain Suharjo Broto Cahyono,1 Putut Bayupurnama,2 Neneng Ratnasari,2 Siti Nurdjanah2 1Department of Internal Medicine, Charitas Hospital, Palembang 2Division of Gastroenterology and Hepatology, Department of Internal Medicine, Faculty of Medicine, Gadjah Mada University-Sardjito General Hospital, Yogyakarta ABSTRAK Gangguan gastrointestinal fungsional (GGIF) mewakili gangguan yang sering dijumpai dan perlu mendapatkan perhatian dalam bidang gastroenterologi. Gangguan ini menyebabkan kecemasan, distress dan morbiditas. Pasien dengan gangguan ini sering memperlihatkan manifestasi klinis secara tumpang tindih. Pasien dispepsia fungsional seringkali tumang tindih dengan gangguan gastrointestinal lain, termasuk nyeri anorektal fungsional. Keadaan tumpang tindih ini dapat menimbulkan keluhan yang makin berat, kualitas hidup yang lebih buruk dan skor somatisasi yang lebih tinggi, dan pasien mengalami kecemasan, depresi atau insomnia lebih sering dibandingkan pasien yang tanpa problem tumpah tindih. GGIF ditegakkan berdasarkan kriteria Rome III dan eksklusi penyakit organik. Pendekatan multimodalitas dibutuhkan dalam mengatasi pasien yang menderita gangguan gastrointestinal fungsional. Pada tinjaun kasus ini, dilaporkan seorang pasien laki laki menderita gangguan dispepsia fungsional dan nyeri anorektal fungsional tidak spesifik. Kata kunci : gangguan -

Prevalence of Functional Disorders of the Bowel, Rectum, and Anus in a Tertiary Urogynecology Population
200 Jelovsek J E1, Barber M D1, Walters M D1, Paraiso M F1 1. The Cleveland Clinic Foundation PREVALENCE OF FUNCTIONAL DISORDERS OF THE BOWEL, RECTUM, AND ANUS IN A TERTIARY UROGYNECOLOGY POPULATION Hypothesis / aims of study Straining is frequently mentioned as a possible etiologic factor in pelvic floor disorders and pelvic denervation. Constipation is a disease that results in frequent straining often seen in patients with pelvic floor disorders. The overall prevalence of constipation in the U.S. population is 14.7%, with 4.6% being functional constipation, 4.6% outlet subtype, 2.1% IBS- constipation subtype, and 3.4% IBS-outlet[1]. The prevalence and clinical subtypes of constipation and other functional bowel, rectal and anal disorders have not been well characterized in women with urinary incontinence (UI) and pelvic organ prolapse (POP). The specific aims of this study were: (1) to determine the prevalence of functional bowel disorders as defined by the Rome II criteria in a tertiary urogynecology clinic, (2) to determine the prevalence of subtypes of constipation, and (3) to determine whether demographic, clinical, or physical exam factors are associated with different types functional bowel, anal, and rectal disorders in patients with prolapse and incontinence. Study design, materials and methods This was a cross-sectional study design. One hundred and fifty consecutive female subjects presenting to a tertiary referral, urogynecology clinic were identified. Demographic, general medical, and physical exam information were collected. The prevalence of functional bowel disorders and functional disorders of the anus and rectum as defined by the Rome II criteria[2] were collected. -

An Osteopathic Approach to Reduction of Readmissions for Neonatal Jaundice
Osteopathic Family Physician (2013) 5, 17–23 REVIEW ARTICLE An osteopathic approach to reduction of readmissions for neonatal jaundice Rachel Click, DO,a Julie Dahl-Smith, DO,a Lindsay Fowler, DO,a Jacqueline DuBose, MD,a Margi Deneau-Saxton, RN, CCCE, CIMI, CLC, CPD,b Jennifer Herbert, MDc From aGeorgia Health Sciences University, Medical College of Georgia, Department of Family Medicine, GA; bGeorgia Health System, OB Labor and Delivery, GA; and cUniversity Primary Care, Evans, GA. KEYWORDS: Jaundice is a potentially life-threatening condition that continues to affect at-risk newborns, accounting Breastfeeding; for continued hospital readmissions. As family physicians, we should be cognizant of neonates who may Jaundice; be at risk for jaundice, including those with pathologic jaundice as well as newborns of breastfeeding Prevention; mothers, and ensure sufficient intervention is taken to help prevent further elevations in bilirubin levels. Hyperbilirubinemia; Interventions are likely to include evaluation for sepsis, education regarding feeding frequencies for both Neonatal massage breast- and bottle-fed neonates, reviewing maternal and hematologic risk factors for neonatal jaundice, and considering inborn errors of metabolism. An additional measure family physicians may consider is that of neonatal massage for those with elevated bilirubin levels. Neonatal massage, though not widely used, has been proven to promote excess bilirubin excretion, thus decreasing length of hospital stay; all the while, providing an intervention that allows parents to take an active role. r 2013 Elsevier Inc. All rights reserved. Introduction morbidity rate with bilirubin 4 20 mg/dL. “It has been estimated that the risk of kernicterus in infants with total Jaundice is a product of excess bilirubin (a product of serum bilirubin (TSB) greater than 30 mg/dL is about 1 in broken down red blood cells), which manifests as a 7 infants”.1 Less serious complications of hyperbilirubine- yellowing of the skin and eyes. -

INFORMED CARING JAUNDICE Neonatal Jaundice BILIARY
1 INFORMED CARING Situations with Adults and Children with Gallbladder, Liver and Pancreatic Disorders 2 JAUNDICE ä Does NOT mean hepatitis ä Increased breakdown of RBCs ä Altered bilirubin breakdown ä Impeded flow through liver or bile duct ä First seen in sclera, then skin 3 Neonatal Jaundice ä Not liver failure ä RBC breakdown ä Phototherapy 4 BILIARY ATRESIA ä Jaundice 2-3 weeks after birth ä Easy bruising ä Stools putty like ä Tea colored urine ä Abdominal/organ distension 5 4 F’s of Gallbladder ä Fair ä Fat X size of person X amount in diet ä Fertile X BCP X Multiparity ä Forty 6 Cholelithiasis ä Calculi within the duct or gallbladder ä Severe colicky, cramp-like pain X radiates to shoulder blade X Murphy's sign ä Cholecystitis: inflammation X Can be caused by trauma, fasting, TPN or abdominal surgery 7 Diagnostic Studies ä Ultrasound of abdomen 1 X not for the obese ä HIDA scan X nuclear medicine ä Cholangiograms X endoscopic X transvenous X intraoperative 8 Post-op Care ä High abdominal incision X respiratory compromise ä T-tube X patients need to know how to empty it X may clamp it prior to removal X caution not dislodged with movements ä NO Morphine X spasms of sphincter of Oddi 9 Post-op Nutrition ä Limited fat in diet X can have rapid transit times ä Potential fat soluble vitamin deficit X A, D, E and K ä Weight loss diet 10 LIVER FAILURE ä Cirrhosis ä Drug toxicity X acetaminophen, anesthetics, HCTZ, chemotherapy ä Infection ä Cancer ä ETOH is single most linked cause 11 LIVER FAILURE S/S ä Don’t show up until 80-90% failed -

Exponential Increase in Stool Crosslinking Is Mirrored in Systemic Inflammation and Associated to Fecal Acetate and Methionine
H OH metabolites OH Article The Importance of Objective Stool Classification in Fecal 1H-NMR Metabolomics: Exponential Increase in Stool Crosslinking Is Mirrored in Systemic Inflammation and Associated to Fecal Acetate and Methionine Leon Deutsch 1 and Blaz Stres 1,2,3,4,* 1 Biotechnical Faculty, University of Ljubljana, Jamnikarjeva 101, SI-1000 Ljubljana, Slovenia; [email protected] 2 Faculty of Civil and Geodetic Engineering, University of Ljubljana, Jamova 2, SI-1000 Ljubljana, Slovenia 3 Department of Automation, Jožef Stefan Institute, Biocybernetics and Robotics, Jamova 39, SI-1000 Ljubljana, Slovenia 4 Department of Microbiology, University of Innsbruck, Technikerstrasse 25d, A-6020 Innsbruck, Austria * Correspondence: [email protected]; Tel.: +386-41-567-633 Abstract: Past studies strongly connected stool consistency—as measured by Bristol Stool Scale (BSS)—with microbial gene richness and intestinal inflammation, colonic transit time and metabolome characteristics that are of clinical relevance in numerous gastro intestinal conditions. While retention time, defecation rate, BSS but not water activity have been shown to account for BSS-associated Citation: Deutsch, L.; Stres, B. The inflammatory effects, the potential correlation with the strength of a gel in the context of intestinal Importance of Objective Stool forces, abrasion, mucus imprinting, fecal pore clogging remains unexplored as a shaping factor for Classification in Fecal 1H-NMR intestinal inflammation and has yet to be determined. Our study introduced a minimal pressure ap- Metabolomics: Exponential Increase proach (MP) by probe indentation as measure of stool material crosslinking in fecal samples. Results in Stool Crosslinking Is Mirrored in reported here were obtained from 170 samples collected in two independent projects, including males Systemic Inflammation and and females, covering a wide span of moisture contents and BSS. -

Symptomatic Approach to Gas, Belching and Bloating 21
20 Osteopathic Family Physician (2019) 20 - 25 Osteopathic Family Physician | Volume 11, No. 2 | March/April, 2019 Gennaro, Larsen Symptomatic Approach to Gas, Belching and Bloating 21 Review ARTICLE to escape. This mechanism prevents the stomach from becoming IRRITABLE BOWEL SYNDROME (IBS) Symptomatic Approach to Gas, Belching and Bloating damaged by excessive dilation.2 IBS is abdominal pain or discomfort associated with altered with OMT Treatment Options Many patients with GERD report increased belching. Transient bowel habits. It is the most commonly diagnosed GI disorder lower esophageal sphincter (LES) relaxation is the major and accounts for about 30% of all GI referrals.7 Criteria for IBS is recurrent abdominal pain at least one day per week in the Carly Gennaro, DO1; Helaine Larsen, DO1 mechanism for both belching and GERD. Recent studies have shown that the number of belches is related to the number of last three months associated with at least two of the following: times someone swallows air. These studies have concluded that 1) association with defecation, 2) change in stool frequency, 1 Good Samaritan Hospital Medical Center, West Islip, NY patients with GERD swallow more air in response to heartburn and 3) change in stool form. Diagnosis should be made using these therefore belch more frequently.3 There is no specific treatment clinical criteria and limited testing. Common symptoms are for belching in GERD patients, so for now, physicians continue to abdominal pain, bloating, alternating diarrhea and constipation, treat GERD with proton pump inhibitors (PPIs) and histamine-2 and pain relief after defecation. Pain can be present anywhere receptor antagonists with the goal of suppressing heartburn and in the abdomen, but the lower abdomen is the most common KEYWORDS: ABSTRACT: Intestinal gas production is a normal physiologic progress. -
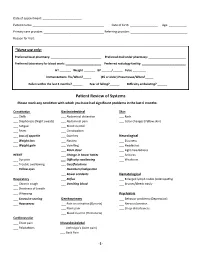
Patient Review of Systems Please Mark Any Condition with Which You Have Had Significant Problems in the Last 6 Months
Date of appointment: ________________________ Patient name: ____________________________________________ Date of birth: _________________ Age: ___________ Primary care provider: _____________________________________ Referring provider: ___________________________________ Reason for Visit: _____________________________________________________________________________________________ *Nurse use only: Preferred local pharmacy: _______________________________ Preferred mail order pharmacy: _______________________ Preferred laboratory for blood work: ______________________ Preferred radiology facility: ___________________________ HT _______ Weight _______ BP ______/______ Pulse ________ Immunizations: Flu/When?_____ (65 or older) Pneumovax/When?_____ Fallen within the last 3 months? ______ Fear of falling?______ Difficulty ambulating? ______ Patient Review of Systems Please mark any condition with which you have had significant problems in the last 6 months: Constitution Gastrointestinal Skin ___ Chills ___ Abdominal distention ___ Rash ___ Diaphoresis (Night sweats) ___ Abdominal pain ___ Color changes (Yellow skin) ___ Fatigue ___ Blood in stool ___ Fever ___ Constipation ___ Loss of appetite ___ Diarrhea Neurological ___ Weight loss ___ Nausea ___ Dizziness ___ Weight gain ___ Vomiting ___ Headaches ___ Black stool ___ Light-headedness HEENT ___ Change in bowel habits ___ Seizures ___ Eye pain ___ Difficulty swallowing ___ Weakness ___ Trouble swallowing ___ Gas/flatulence ___ Yellow eyes ___ Heartburn/indigestion ___ Bowel accidents Hematological -

Anorectal Disorders
View metadata, citation and similar papers at core.ac.uk brought to you by CORE HHS Public Access provided by Carolina Digital Repository Author manuscript Author ManuscriptAuthor Manuscript Author Gastroenterology Manuscript Author . Author Manuscript Author manuscript; available in PMC 2017 September 25. Anorectal Disorders Satish S. C. Rao1, Adil E. Bharucha2, Giuseppe Chiarioni3,4, Richelle Felt-Bersma5, Charles Knowles6, Allison Malcolm7, and Arnold Wald8 1Division of Gastroenterology and Hepatology, Augusta University, Augusta, Georgia 2Department of Gastroenterology and Hepatology, Mayo College of Medicine, Rochester, Minnesota 3Division of Gastroenterology of the University of Verona, Azienda Ospedaliera Universitaria Integrata di Verona, Verona, Italy 4Division of Gastroenterology and Hepatology and UNC Center for Functional GI and Motility Disorders, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina 5Department of Gastroenterology/Hepatology, VU Medical Center, Amsterdam, The Netherlands 6National Centre for Bowel Research and Surgical Innovation, Blizard Institute, Queen Mary University of London, London, United Kingdom 7Division of Gastroenterology, Royal North Shore Hospital, and University of Sydney, Sydney, Australia 8Division of Gastroenterology, University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin Abstract This report defines criteria and reviews the epidemiology, pathophysiology, and management of the following common anorectal disorders: fecal incontinence (FI), functional anorectal pain, and functional defecation disorders. FI is defined as the recurrent uncontrolled passage of fecal material for at least 3 months. The clinical features of FI are useful for guiding diagnostic testing and therapy. Anorectal manometry and imaging are useful for evaluating anal and pelvic floor structure and function. Education, antidiarrheals, and biofeedback therapy are the mainstay of management; surgery may be useful in refractory cases. -

A Deep Learning Approach to Human Stool Recognition And
Augmenting Gastrointestinal Health: A Deep Learning Approach to Human Stool Recognition and Characterization in Macroscopic Images David Hachuel Akshay Jha Deborah Estrin, PhD Cornell Tech Cornell Tech Cornell Tech Cornell University Cornell University Cornell University New York, NY, USA New York, NY, USA New York, NY, USA [email protected] [email protected] [email protected] Alfonso Martinez Kyle Staller, MD, MPH Christopher Velez, MD Massachusetts Institute Massachusetts General Massachusetts General of Technology Hospital Hospital Cambridge, MA, USA Boston, MA, USA Boston, MA, USA [email protected] [email protected] [email protected] ABSTRACT Results - In terms of inter-rater reliability, the Kappa score UPDATED—4 December 2018. Purpose - Functional was κ = 0.5840. Regarding the stool detection task, our bowel diseases, including irritable bowel syndrome, chronic modified SegNet produced a 71.93% mIoU on a test set of constipation, and chronic diarrhea, are some of the most 282 images when trained on 651 images. Current common diseases seen in clinical practice. Many patients state-of-the-art segmentation models reach 83.2% mIoU describe a range of triggers for altered bowel consistency when trained on significantly larger datasets. As for BSS and symptoms. However, characterization of the classification using the ResNet architecture, our mean relationship between symptom triggers using bowel diaries accuracy is 74.26% on a test set of 272 images when trained is hampered by poor compliance and lack of objective stool on 614 images. In comparison, the ResNet trained on the consistency measurements. We sought to develop a stool secondary dataset achieved 99.4% accuracy in classifying detection and tracking system using computer vision and BSS on a test set of 10800 images when trained on 25200 deep convolutional neural networks (CNN) that could be images. -

And Sulphate-Rich Natural Mineral Water in Functional Constipation
Nutrition 65 (2019) 167À172 Contents lists available at ScienceDirect Nutrition journal homepage: www.nutritionjrnl.com Applied nutritional investigation Time to treatment response of a magnesium- and sulphate-rich natural mineral water in functional constipation Christophe Dupont M.D., Ph.D. a,*, Florence Constant M.D., Ph.D. b, Aurelie Imbert M.Sc. b, Guillaume Hebert Ph.D., M.B.A. c, Othar Zourabichvili M.D., Ph.D. d, Nathalie Kapel Pharm.D., Ph.D. e a Service d'Explorations Fonctionnelles Digestives Pediatriques, AP-HP, Hopital^ Necker Enfant Malade, Universite Paris Descartes, Paris, France b Nestle Waters M.T., Issy-les-Moulineaux, France c SC Partners, Paris, France d Quanta Medical, Rueil-Malmaison, France e Laboratoire de Coprologie Fonctionnelle, Hopitaux^ Universitaires Pitie Salp^etriere - Charles Foix, APHP, Paris, France ARTICLE INFO ABSTRACT Article History: Objectives: First-line recommendations for the management of functional constipation include nutritional- Received 11 June 2018 hygienic measures. We previously showed that a natural mineral water rich in sulphates and magnesium Received in revised form 22 February 2019 (Hepar) is efficient in the treatment of functional constipation. The aim of this study was to consolidate those Accepted 24 February 2019 first results and determine a precise time to respond to Hepar. Keywords: Methods: This multicenter, randomized, double-blind, controlled study of the effect of Hepar on stool consis- Bowel movement tency and frequency in functional constipation included 226 outpatients. After washout, patients used 1.5 L Functional constipation of water daily, including 1 L of Hepar or of low-mineral water, during 14 d. In addition to a daily reporting of Clinical trial stool consistency by the patient, an expert investigator blindly analyzed stool consistency (Bristol stool scale) Natural mineral water based on photographs taken by the patient.