Traveller's Diarrhoea (TD) Is the Commonest Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2.04.26 Fecal Analysis in the Diagnosis of Intestinal Dysbiosis and Irritable Bowel Syndrome
MEDICAL POLICY – 2.04.26 Fecal Analysis in the Diagnosis of Intestinal Dysbiosis and Irritable Bowel Syndrome BCBSA Ref. Policy: 2.04.26 Effective Date: July 1, 2021 RELATED MEDICAL POLICIES: Last Revised: June 8, 2021 None Replaces: N/A Select a hyperlink below to be directed to that section. POLICY CRITERIA | DOCUMENTATION REQUIREMENTS | CODING RELATED INFORMATION | EVIDENCE REVIEW | REFERENCES | HISTORY ∞ Clicking this icon returns you to the hyperlinks menu above. Introduction Intestinal dysbiosis is a condition that occurs when the microorganisms in the digestive tract are out of balance. This condition is believed to cause diseases of the digestive tract, including poor nutrient absorption, overgrowth of certain bacteria, and irritable bowel syndrome (IBS). Symptoms of these digestive problems are similar and may include: abdominal pain, excess gas, bloating, and changes in bowel movements (constipation or diarrhea, or both). One method of diagnosing digestive disorders is by testing a fecal sample. Using fecal analysis to diagnose intestinal dysbiosis, IBS, malabsorption, or small intestinal overgrowth of bacteria is unproven (investigational). More studies are needed to see if this testing improves health outcomes. Note: The Introduction section is for your general knowledge and is not to be taken as policy coverage criteria. The rest of the policy uses specific words and concepts familiar to medical professionals. It is intended for providers. A provider can be a person, such as a doctor, nurse, psychologist, or dentist. A provider also can be a place where medical care is given, like a hospital, clinic, or lab. This policy informs them about when a service may be covered. -

Traveler's Diarrhea
Traveler’s Diarrhea JOHNNIE YATES, M.D., CIWEC Clinic Travel Medicine Center, Kathmandu, Nepal Acute diarrhea affects millions of persons who travel to developing countries each year. Food and water contaminated with fecal matter are the main sources of infection. Bacteria such as enterotoxigenic Escherichia coli, enteroaggregative E. coli, Campylobacter, Salmonella, and Shigella are common causes of traveler’s diarrhea. Parasites and viruses are less common etiologies. Travel destination is the most significant risk factor for traveler’s diarrhea. The efficacy of pretravel counseling and dietary precautions in reducing the incidence of diarrhea is unproven. Empiric treatment of traveler’s diarrhea with antibiotics and loperamide is effective and often limits symptoms to one day. Rifaximin, a recently approved antibiotic, can be used for the treatment of traveler’s diarrhea in regions where noninvasive E. coli is the predominant pathogen. In areas where invasive organisms such as Campylobacter and Shigella are common, fluoroquinolones remain the drug of choice. Azithromycin is recommended in areas with qui- nolone-resistant Campylobacter and for the treatment of children and pregnant women. (Am Fam Physician 2005;71:2095-100, 2107-8. Copyright© 2005 American Academy of Family Physicians.) ILLUSTRATION BY SCOTT BODELL ▲ Patient Information: cute diarrhea is the most com- mised and those with lowered gastric acidity A handout on traveler’s mon illness among travelers. Up (e.g., patients taking histamine H block- diarrhea, written by the 2 author of this article, is to 55 percent of persons who ers or proton pump inhibitors) are more provided on page 2107. travel from developed countries susceptible to traveler’s diarrhea. -

Amoebic Dysentery
University of Nebraska Medical Center DigitalCommons@UNMC MD Theses Special Collections 5-1-1934 Amoebic dysentery H. C. Dix University of Nebraska Medical Center This manuscript is historical in nature and may not reflect current medical research and practice. Search PubMed for current research. Follow this and additional works at: https://digitalcommons.unmc.edu/mdtheses Part of the Medical Education Commons Recommended Citation Dix, H. C., "Amoebic dysentery" (1934). MD Theses. 320. https://digitalcommons.unmc.edu/mdtheses/320 This Thesis is brought to you for free and open access by the Special Collections at DigitalCommons@UNMC. It has been accepted for inclusion in MD Theses by an authorized administrator of DigitalCommons@UNMC. For more information, please contact [email protected]. A MOE B leD Y SEN T E R Y By H. c. Dix University of Nebraska College of Medicine Omaha, N~braska April 1934 Preface This paper is presented to the University of Nebraska College of MediCine to fulfill the senior requirements. The subject of amoebic dysentery wa,s chosen due to the interest aroused from the previous epidemic, which started in Chicago la,st summer (1933). This disea,se has previously been considered as a tropical disease, B.nd was rarely seen and recognized in the temperate zone. Except in indl vidu8,ls who had been in the tropics previously. In reviewing the literature, I find that amoebio dysentery may be seen in any part of the world, and from surveys made, the incidence is five in every hun- dred which harbor the Entamoeba histolytlca, it being the only pathogeniC amoeba of the human gastro-intes tinal tract. -

An Osteopathic Approach to Reduction of Readmissions for Neonatal Jaundice
Osteopathic Family Physician (2013) 5, 17–23 REVIEW ARTICLE An osteopathic approach to reduction of readmissions for neonatal jaundice Rachel Click, DO,a Julie Dahl-Smith, DO,a Lindsay Fowler, DO,a Jacqueline DuBose, MD,a Margi Deneau-Saxton, RN, CCCE, CIMI, CLC, CPD,b Jennifer Herbert, MDc From aGeorgia Health Sciences University, Medical College of Georgia, Department of Family Medicine, GA; bGeorgia Health System, OB Labor and Delivery, GA; and cUniversity Primary Care, Evans, GA. KEYWORDS: Jaundice is a potentially life-threatening condition that continues to affect at-risk newborns, accounting Breastfeeding; for continued hospital readmissions. As family physicians, we should be cognizant of neonates who may Jaundice; be at risk for jaundice, including those with pathologic jaundice as well as newborns of breastfeeding Prevention; mothers, and ensure sufficient intervention is taken to help prevent further elevations in bilirubin levels. Hyperbilirubinemia; Interventions are likely to include evaluation for sepsis, education regarding feeding frequencies for both Neonatal massage breast- and bottle-fed neonates, reviewing maternal and hematologic risk factors for neonatal jaundice, and considering inborn errors of metabolism. An additional measure family physicians may consider is that of neonatal massage for those with elevated bilirubin levels. Neonatal massage, though not widely used, has been proven to promote excess bilirubin excretion, thus decreasing length of hospital stay; all the while, providing an intervention that allows parents to take an active role. r 2013 Elsevier Inc. All rights reserved. Introduction morbidity rate with bilirubin 4 20 mg/dL. “It has been estimated that the risk of kernicterus in infants with total Jaundice is a product of excess bilirubin (a product of serum bilirubin (TSB) greater than 30 mg/dL is about 1 in broken down red blood cells), which manifests as a 7 infants”.1 Less serious complications of hyperbilirubine- yellowing of the skin and eyes. -

Ulcerative Post-Dysenteric Colitis
Gut: first published as 10.1136/gut.7.5.438 on 1 October 1966. Downloaded from Gut, 1966, 7, 438 Ulcerative post-dysenteric colitis S. J. POWELL AND A. J. WILMOT From the Amoebiasis Research Unit' and the Department ofMedicine, University ofNatal, Durban, South Africa EDITORIAL COMMENT Better treatment is resulting in more severe cases of amoebic colitis surviving and these patients may have severe residual damage to the bowel resulting in ulcerative post-dysenteric colitis. This is considered to be a distinct entity. The term 'post-dysenteric colonic irritability' was thousand patients who attend this hospital annually introduced by Sir Arthur Hurst (1943) to describe with acute amoebic dysentery complications are persistent irritability of the bowel following an acute common and we have had the opportunity to study attack of bacillary or amoebic dysentery. The early them (Wilmot, 1962). It is from this material that we symptoms were attributed to a non-specific chronic have based the following report of ulcerative post- colitis occurring after the specific infection had died dysenteric colitis in 33 African patients observed in out, but in the later stages were thought to be due to recent years. 'functional irritability' of the colon. Stewart (1950) found that post-dysenteric colitis was more common- CLINICAL FINDINGS ly a sequel to acute amoebic dysentery and was able All patients presented initially with severe amoebic to recognize two forms in his patients: 1 Those with dysentery, sigmoidoscopic examination showing a mild symptoms and no colonic ulceration, which he congested, oedematous mucosa with extensive rectal named 'functional post-dysenteric colitis', and (2) ulcers the surfaces of which were covered by sloughs http://gut.bmj.com/ Those with colonic ulceration and more severe and exudate. -

Remarks on Pelvic Peritonitis and Pelvic Cellulitis, with Illustrative Cases
Article IV.- Remarks on Pelvic Peritonitis and Pelvic Cellulitis, with Illustrative Cases. By Lauchlan Aitken, M.D. Rather moie than a year ago there appeared from the pen of a well- known of this a gynecologist city very able monograph on the two forms of pelvic inflammation whose names head this article; and it cannot have escaped the recollection of the reader that Dr M. Dun- can, adopting the nomenclature first proposed by Yirchow, has used on his different terms title-page1 than those older appellations I still to retain. Under these propose ^ circumstances I feel at to compelled least to attempt justify my preference for the original names: and I trust to be able to show that are they preferable to, and less con- others that fusing than, any have as yet been proposed, even though we cannot consider them absolutely perfect. 1 Treatise on A Practical Perimetritis and Parametritis (Edin. 1869). 1870.] DR LAUCI1LAN AITKEN ON PELVIC FERITONITIS, ETC. 889 Passing over, then, such terms as 'periuterine cellulitis or phleg- mons periuterins as bad compounds ; others, as inflammation of the broad ligaments, as too limited in meaning ; and others, again, as engorgement periutdrin, as only indicating one of the stages of the affection,?I shall endeavour as succinctly as possible to state my reasons for preferring the older names to those proposed by Virchow. ls?. The two Greek prepositions, peri and para, are employed somewhat arbitrarily to indicate inflammatory processes which are essentially distinct. I say arbitrarily, because I am not aware that para has been generally employed in the form of a compound to ex- press inflammation of the cellular tissue elsewhere.1 By those who remember that the cellular tissue not only separates the serous membrane from the uterus at that part where the cervix and body of the organ meet, but is even abundant there,2 perimetritis might readily be taken to indicate one of the varieties, though indeed not a in for which very common one, of pelvic cellulitis?a variety, fact, the term perimetric cellulitis has been proposed. -

INFORMED CARING JAUNDICE Neonatal Jaundice BILIARY
1 INFORMED CARING Situations with Adults and Children with Gallbladder, Liver and Pancreatic Disorders 2 JAUNDICE ä Does NOT mean hepatitis ä Increased breakdown of RBCs ä Altered bilirubin breakdown ä Impeded flow through liver or bile duct ä First seen in sclera, then skin 3 Neonatal Jaundice ä Not liver failure ä RBC breakdown ä Phototherapy 4 BILIARY ATRESIA ä Jaundice 2-3 weeks after birth ä Easy bruising ä Stools putty like ä Tea colored urine ä Abdominal/organ distension 5 4 F’s of Gallbladder ä Fair ä Fat X size of person X amount in diet ä Fertile X BCP X Multiparity ä Forty 6 Cholelithiasis ä Calculi within the duct or gallbladder ä Severe colicky, cramp-like pain X radiates to shoulder blade X Murphy's sign ä Cholecystitis: inflammation X Can be caused by trauma, fasting, TPN or abdominal surgery 7 Diagnostic Studies ä Ultrasound of abdomen 1 X not for the obese ä HIDA scan X nuclear medicine ä Cholangiograms X endoscopic X transvenous X intraoperative 8 Post-op Care ä High abdominal incision X respiratory compromise ä T-tube X patients need to know how to empty it X may clamp it prior to removal X caution not dislodged with movements ä NO Morphine X spasms of sphincter of Oddi 9 Post-op Nutrition ä Limited fat in diet X can have rapid transit times ä Potential fat soluble vitamin deficit X A, D, E and K ä Weight loss diet 10 LIVER FAILURE ä Cirrhosis ä Drug toxicity X acetaminophen, anesthetics, HCTZ, chemotherapy ä Infection ä Cancer ä ETOH is single most linked cause 11 LIVER FAILURE S/S ä Don’t show up until 80-90% failed -

Symptomatic Approach to Gas, Belching and Bloating 21
20 Osteopathic Family Physician (2019) 20 - 25 Osteopathic Family Physician | Volume 11, No. 2 | March/April, 2019 Gennaro, Larsen Symptomatic Approach to Gas, Belching and Bloating 21 Review ARTICLE to escape. This mechanism prevents the stomach from becoming IRRITABLE BOWEL SYNDROME (IBS) Symptomatic Approach to Gas, Belching and Bloating damaged by excessive dilation.2 IBS is abdominal pain or discomfort associated with altered with OMT Treatment Options Many patients with GERD report increased belching. Transient bowel habits. It is the most commonly diagnosed GI disorder lower esophageal sphincter (LES) relaxation is the major and accounts for about 30% of all GI referrals.7 Criteria for IBS is recurrent abdominal pain at least one day per week in the Carly Gennaro, DO1; Helaine Larsen, DO1 mechanism for both belching and GERD. Recent studies have shown that the number of belches is related to the number of last three months associated with at least two of the following: times someone swallows air. These studies have concluded that 1) association with defecation, 2) change in stool frequency, 1 Good Samaritan Hospital Medical Center, West Islip, NY patients with GERD swallow more air in response to heartburn and 3) change in stool form. Diagnosis should be made using these therefore belch more frequently.3 There is no specific treatment clinical criteria and limited testing. Common symptoms are for belching in GERD patients, so for now, physicians continue to abdominal pain, bloating, alternating diarrhea and constipation, treat GERD with proton pump inhibitors (PPIs) and histamine-2 and pain relief after defecation. Pain can be present anywhere receptor antagonists with the goal of suppressing heartburn and in the abdomen, but the lower abdomen is the most common KEYWORDS: ABSTRACT: Intestinal gas production is a normal physiologic progress. -

Molecular Characterization of Enterotoxigenic Escherichia Coli
iolog ter y & c P a a B r f a o s i l t o a l n o r Yameen et al., J Bacteriol Parasitol 2018, 9:3 g u y o J Bacteriology and Parasitology DOI: 10.4172/2155-9597.1000339 ISSN: 2155-9597 Research Article Open Access Molecular Characterization of Enterotoxigenic Escherichia coli: Effect on Intestinal Nitric Oxide in Diarrheal Disease Muhammad Arfat Yameen1, Ebuka Elijah David2*, Humphrey Chukwuemeka Nzelibe3, Muhammad Nasir Shuaibu3, Rabiu Abdussalam Magaji4, Amakaeze Jude Odugu5 and Ogamdi Sunday Onwe6 1Department of Pharmacy, COMSATS Institute of Information Technology, Abbottabad, Pakistan 2Department of Biochemistry, Federal University, Ndufu-Alike, Ikwo, Ebonyi State, Nigeria 3Department of Biochemistry, Ahmadu Bello University, Zaria, Kaduna State, Nigeria 4Department of Human Physiology, Ahmadu Bello University, Zaria, Kaduna State, Nigeria 5Medical Laboratory, Ahmadu Bello University, Teaching Hospital, Zaria, Kaduna State, Nigeria 6Laboratory Service Unit, Federal Teaching Hospital, Abakiliki, Ebonyi State, Nigeria *Corresponding author: Ebuka Elijah David, Department of Biochemistry, Federal University, Ndufu-Alike, Ikwo, Ebonyi State, Nigeria, Tel: +2348033188823; E-mail: [email protected] Received date: May 01, 2018; Accepted date: May 25, 2018; Published date: May 30, 2018 Copyright: ©2018 Yameen MA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract This study was aimed to investigate the effect of enterotoxigenic E. coli (ETEC)-induced diarrhea on fecal nitric oxide (NO) and intestinal inducible nitric oxide synthase (iNOS) expression in rats. -
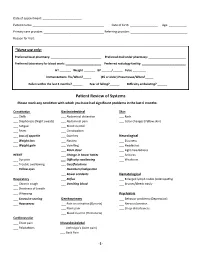
Patient Review of Systems Please Mark Any Condition with Which You Have Had Significant Problems in the Last 6 Months
Date of appointment: ________________________ Patient name: ____________________________________________ Date of birth: _________________ Age: ___________ Primary care provider: _____________________________________ Referring provider: ___________________________________ Reason for Visit: _____________________________________________________________________________________________ *Nurse use only: Preferred local pharmacy: _______________________________ Preferred mail order pharmacy: _______________________ Preferred laboratory for blood work: ______________________ Preferred radiology facility: ___________________________ HT _______ Weight _______ BP ______/______ Pulse ________ Immunizations: Flu/When?_____ (65 or older) Pneumovax/When?_____ Fallen within the last 3 months? ______ Fear of falling?______ Difficulty ambulating? ______ Patient Review of Systems Please mark any condition with which you have had significant problems in the last 6 months: Constitution Gastrointestinal Skin ___ Chills ___ Abdominal distention ___ Rash ___ Diaphoresis (Night sweats) ___ Abdominal pain ___ Color changes (Yellow skin) ___ Fatigue ___ Blood in stool ___ Fever ___ Constipation ___ Loss of appetite ___ Diarrhea Neurological ___ Weight loss ___ Nausea ___ Dizziness ___ Weight gain ___ Vomiting ___ Headaches ___ Black stool ___ Light-headedness HEENT ___ Change in bowel habits ___ Seizures ___ Eye pain ___ Difficulty swallowing ___ Weakness ___ Trouble swallowing ___ Gas/flatulence ___ Yellow eyes ___ Heartburn/indigestion ___ Bowel accidents Hematological -

The Global View of Campylobacteriosis
FOOD SAFETY THE GLOBAL VIEW OF CAMPYLOBACTERIOSIS REPORT OF AN EXPERT CONSULTATION UTRECHT, NETHERLANDS, 9-11 JULY 2012 THE GLOBAL VIEW OF CAMPYLOBACTERIOSIS IN COLLABORATION WITH Food and Agriculture of the United Nations THE GLOBAL VIEW OF CAMPYLOBACTERIOSIS REPORT OF EXPERT CONSULTATION UTRECHT, NETHERLANDS, 9-11 JULY 2012 IN COLLABORATION WITH Food and Agriculture of the United Nations The global view of campylobacteriosis: report of an expert consultation, Utrecht, Netherlands, 9-11 July 2012. 1. Campylobacter. 2. Campylobacter infections – epidemiology. 3. Campylobacter infections – prevention and control. 4. Cost of illness I.World Health Organization. II.Food and Agriculture Organization of the United Nations. III.World Organisation for Animal Health. ISBN 978 92 4 156460 1 _____________________________________________________ (NLM classification: WF 220) © World Health Organization 2013 All rights reserved. Publications of the World Health Organization are available on the WHO web site (www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications –whether for sale or for non-commercial distribution– should be addressed to WHO Press through the WHO web site (www.who.int/about/licensing/copyright_form/en/index. html). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. -

Unusual Presentation of Shigellosis: Acute Perforated Appendicitis And
Case Report 45 Unusual Presentation of Shigellosis: Acute Perforated Appendicitis and Peritonitis Gülsüm İclal Bayhan1, Gönül Tanır1, Haşim Ata Maden2, Şengül Özkan3 1Pediatric Infection Clinic, Dr. Sami Ulus Gynecology, Child Care and Treatment Training and Research Hospital, Ankara, Turkey 2Department of Pediatric Surgery, Dr. Sami Ulus Gynecology, Child Care and Treatment Training and Research Hospital, Ankara, Turkey 3Microbiology Clinic. Dr. Sami Ulus Gynecology, Child Care and Treatment Training and Research Hospital, Ankara, Turkey Abstract Shigella spp. is one of the most common agents that cause bacterial diarrhea and dysentery in developing coun- tries. Clinical presentation of shigellosis may vary over a wide spectrum from mild diarrhea to severe dysentery. We report the case of 5.5-year-old previously healthy boy, who presented to our clinic with abdominal pain, vomiting, and constipation. On examination, we noticed abdominal tenderness with guarding at the right lower quadrant. With the diagnosis of acute appendicitis, open appendectomy was performed. Exploration of the abdominal cavity revealed perforated appendicitis and generalized peritonitis. Shigella sonnei was isolated from the peritoneal fluid culture. The patient completely recovered without any complications. Surgical complications, including appendicitis, could have developed during shigellosis. There are few reported cases of perforated appendicitis associated with Shigella. Prompt surgical intervention can be beneficial to prevent morbidity and mortality if it is performed early in the course of the disease. (J Pediatr Inf 2015; 9: 45-8) Keywords: Shigella spp., acute appendicitis, peritonitis, surgical complication Introduction intestinal and extra-intestinal complications. There are few reported cases of perforated Shigella spp., a group of Gram-negative, appendicitis complicated with peritonitis due to Received: 04.10.2013 Accepted: 03.02.2014 small, non-motile, non-spore forming, and rod- Shigella spp.