Fructose Malabsorption Hereditary Condition.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Prevalence of Fructose Malabsorption in Patients with Irritable Bowel Syndrome After Excluding Small Intestinal Bacterial Overgrowth
J Neurogastroenterol Motil, Vol. 24 No. 2 April, 2018 pISSN: 2093-0879 eISSN: 2093-0887 https://doi.org/10.5056/jnm17044 JNM Journal of Neurogastroenterology and Motility Original Article Prevalence of Fructose Malabsorption in Patients With Irritable Bowel Syndrome After Excluding Small Intestinal Bacterial Overgrowth Kee Wook Jung,1 Myeognsook Seo,1 Young Hwan Cho,1 Young-Ok Park,2 So-Yoon Yoon,2 Jungbok Lee,3 Dong-Hoon Yang,1 In Ja Yoon,1 So Young Seo,1 Hyo Jeong Lee,1 Sang Hyoung Park,1 Kyung Jo Kim,1 Byong Duk Ye,1 Jeong-Sik Byeon,1 Hwoon-Yong Jung,1 Suk-Kyun Yang,1 Jin-Ho Kim,1 and Seung-Jae Myung1* Departments of 1Gastroenterology, 2Clinical Nutrition, and 3Clinical Epidemiology and Biostatistics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea Background/Aims Fructose malabsorption (FM) mimics symptoms of irritable bowel syndrome (IBS), and its prevalence has increased. Diagnosing FM in IBS is challenging because of its overlap with small intestinal bacterial overgrowth (SIBO). We assessed the prevalence of FM by comparing patients with IBS with asymptomatic control individuals after excluding SIBO using the glucose hydrogen breath test (HBT). Methods Patients diagnosed with IBS and asymptomatic control individuals were enrolled prospectively. Dietary habits were assessed with the Food Frequency Questionnaire. After excluding SIBO, participants underwent HBTs with both 15 g and 25 g of fructose. Results Thirty-five patients with IBS and 35 age- and sex-matched asymptomatic control individuals were enrolled. The 15-g fructose HBT yielded positive results in 7 of the 35 (20.0%) patients with IBS and in 2 of 35 (5.7%) controls (P = 0.070). -

Limiting Fructose, Fructans Intake May Ease IBS
36 Digestive Disorders FAMILY P RACTICE N EWS • July 1, 2008 Limiting Fructose, Fructans Intake May Ease IBS BY MARY ANN MOON “marked and sustained global improve- of irritable bowel syndrome (IBS) in patients prove symptoms. In the current study, the Contributing Writer ment in gastrointestinal symptoms,” re- who also have fructose malabsorption. researchers focused on osmotic load with- searchers noted. A subsequent study of The results also demonstrate that re- in the lumen and fermentative gas content. atients with irritable bowel syn- the patients revealed that symptom relief stricting intake of these substances may Poorly absorbed short-chain carbohy- drome and fructose malabsorption was not specific to restricted intake of lead to durable symptomatic improve- drates, including fructose and lactose, are Pappeared to benefit from a diet that fructose, but was achieved by limiting the ment, wrote Ms. Shepherd, a dietician at highly fermentable. They exert a strong restricted intake of fructose and fructans, intake of poorly absorbed short-chain Australia’s Monash University, Clayton, osmotic effect in people who have malab- Susan J. Shepherd and her colleagues re- carbohydrates. Victoria, and her colleagues. sorption of these two sugars—about 40% ported in an article appearing in the July These findings “represent the first high- They theorized that, because many ab- of the population in the case of fructose, 2008 issue of Clinical Gastroenterology level evidence” that poorly absorbed short- dominal symptoms may originate from and between 15% to 100% of the popula- and Hepatology. chain carbohydrates—fructose and fruc- bowel distension, addressing factors that tion for lactose. In the 25-patient study, the diet led to tans—are dietary triggers for the symptoms contribute to the distension would im- To minimize or eliminate intake of poor- ly absorbed short-chain carbohydrates, the investigators created a diet that omitted Brief Summary—see package insert for full prescribing information. -

Chrebp-Knockout Mice Show Sucrose Intolerance and Fructose Malabsorption
nutrients Article ChREBP-Knockout Mice Show Sucrose Intolerance and Fructose Malabsorption Takehiro Kato 1, Katsumi Iizuka 1,2,* ID , Ken Takao 1, Yukio Horikawa 1, Tadahiro Kitamura 3 and Jun Takeda 1 1 Department of Diabetes and Endocrinology, Graduate School of Medicine, Gifu University, Gifu 501-1194, Japan; [email protected] (T.K.); [email protected] (K.T.); [email protected] (Y.H.); [email protected] (J.T.) 2 Gifu University Hospital Center for Nutritional Support and Infection Control, Gifu 501-1194, Japan 3 Metabolic Signal Research Center, Institute for Molecular and Cellular Regulation, Gunma University, Gunma 371-8512, Japan; [email protected] * Correspondence: [email protected]; Tel.: +81-58-230-6564; Fax: +81-58-230-6376 Received: 31 January 2018; Accepted: 9 March 2018; Published: 10 March 2018 Abstract: We have previously reported that 60% sucrose diet-fed ChREBP knockout mice (KO) showed body weight loss resulting in lethality. We aimed to elucidate whether sucrose and fructose metabolism are impaired in KO. Wild-type mice (WT) and KO were fed a diet containing 30% sucrose with/without 0.08% miglitol, an α-glucosidase inhibitor, and these effects on phenotypes were tested. Furthermore, we compared metabolic changes of oral and peritoneal fructose injection. A thirty percent sucrose diet feeding did not affect phenotypes in KO. However, miglitol induced lethality in 30% sucrose-fed KO. Thirty percent sucrose plus miglitol diet-fed KO showed increased cecal contents, increased fecal lactate contents, increased growth of lactobacillales and Bifidobacterium and decreased growth of clostridium cluster XIVa. -

Fructose Malabsorption in Patients with Irritable Bowel Syndrome-Like Symptoms: What Is the Role in the Pathogenesis and Clinical Implication?
J Neurogastroenterol Motil, Vol. 20 No. 2 April, 2014 pISSN: 2093-0879 eISSN: 2093-0887 http://dx.doi.org/10.5056/jnm.2014.20.2.135 JNM Journal of Neurogastroenterology and Motility Editorial Fructose Malabsorption in Patients With Irritable Bowel Syndrome-like Symptoms: What Is the Role in the Pathogenesis and Clinical Implication? Hye-Young Sung and Yong Sung Kim* Division of Gastroenterology, Department of Internal Medicine, Digestive Disease Research Institute, Wonkwang University Sanbon Hospital, Gunpo-si, Gyeonggi-do, Korea Article: Unclear abdominal discomfort: pivotal role of carbohydrate malabsorption Goebel-Stengel M, Stengel A, Schmidtmann M, van der Voort I, Kobelt P, Mönnikes H. (J Neurogastroenterol Motil 2014;20:228-235) Abdominal discomfort with negative medical tests is a com- respectively. Although this was an observational study in a single mon presentation in the gastrointestinal (GI) clinic, and it is usu- center and not an interventional study, the number of enrolled pa- ally diagnosed as irritable bowel syndrome (IBS). However, car- tients was 2,390, making this the largest patient population study bohydrate malabsorption, especially fructose malabsorption (FM), to date.4 has been reported as another cause of unexplained abdominal However, this result could not be applied directly to IBS be- symptoms, and also suggested to have a role in the pathogenesis cause the patients in this study were not exactly diagnosed and of IBS. It has been reported that dietary fructose restriction and a classified by Rome criteria, but simply described as “patients with low fermentable oligosaccharides, disaccharides, monosaccha- IBS-like symptoms.” Even so, the results from this study suggest rides and polyols (FODMAPs) diet effectively reduced GI that the prevalence of FM is high in patients with unexplained symptoms in patients with IBS, suggesting that these restrictions abdominal symptoms, making this an important etiology in func- should be considered as a front-line therapy.1,2 tional GI disorders (FGID) like IBS. -

Fructose Malabsorption: Causes, Diagnosis and Treatment
Downloaded from British Journal of Nutrition, page 1 of 9 doi:10.1017/S0007114521001215 https://www.cambridge.org/core © The Author(s), 2021. Published by Cambridge University Press on behalf of The Nutrition Society. This is an Open Access article, distributed under the terms of the Creative Commons Attribution licence (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted re-use, distribution, and reproduction in any medium, provided the original work is properly cited. Fructose malabsorption: causes, diagnosis and treatment . IP address: Miles Benardout1*, Adam Le Gresley1, Amr ElShaer2 and Stephen P. Wren1* 1Department of Chemical and Pharmaceutical Sciences, Faculty of Science, Engineering and Computing, Kingston University London, Penryhn Road, Surrey KT12EE, UK 170.106.35.229 2Department of Pharmacy, Faculty of Science, Engineering and Computing, Kingston University London, Penryhn Road, Surrey KT12EE, UK (Submitted 14 October 2020 – Final revision received 19 February 2021 – Accepted 28 March 2021) , on 25 Sep 2021 at 13:47:17 Abstract This review intends to act as an overview of fructose malabsorption (FM) and its role in the aetiology of diseases including, but not limited to, irritable bowel syndrome (IBS) and infantile colic and the relationship between fructose absorption and the propagation of some cancers. IBS results in a variety of symptoms including stomach pains, cramps and bloating. Patients can be categorised into two groups, depending on whether the patients’ experiences either constipation (IBS-C) or diarrhoea (IBS-D). FM has been proposed as a potential cause of IBS-D , subject to the Cambridge Core terms of use, available at and other diseases, such as infantile colic. -

Low Fructose Diet
Low Fructose Diet What is Fructose? Fructose is a natural sugar found in fruit, fruit juices, honey, and agave syrup. It is also found in some vegetables and wheat products in another form called fructans (fructose sugars in a long chain). High fructose corn syrup (HFCS) is another form of fructose commonly used in processed foods. What is Fructose Intolerance? Fructose intolerance, also called dietary fructose intolerance or fructose malabsorption, happens when a person cannot properly absorb normal amounts of fructose (>25 grams per meal). What are common symptoms? Unabsorbed fructose that reaches the large intestine can be fermented (converted into gas) by bacteria causing symptoms like abdominal pain, gas, belching, and bloating. Unabsorbed fructose can also pull water back into the colon, increasing gut motility and causing diarrhea. Less common symptoms of fructose intolerance can include reflux, depression, fatigue, brain fog, headache, weight loss, and sugar cravings. How is Fructose Intolerance diagnosed? Anyone can develop fructose intolerance, but it is more common among individuals with irritable bowel syndrome (IBS) or other gastrointestinal disorders. A Hydrogen Breath Test is used to diagnosis fructose intolerance. An abnormal (positive) test indicates the need for a low fructose diet. What is a Low Fructose Diet? A low fructose diet reduces the amount of fructose consumed by limiting or avoiding foods with excess fructose (foods that contain more than half of their natural sugar as fructose), foods with high fructose (more than 3 grams), and foods that are a significant source of fructans (chains of fructose). How long does this diet need to be followed? A low fructose diet should be followed until symptoms improve, typically 2-6 weeks. -
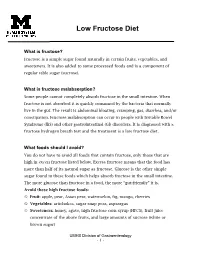
Low Fructose Diet
Low Fructose Diet What is fructose? Fructose is a simple sugar found naturally in certain fruits, vegetables, and sweeteners. It is also added to some processed foods and is a component of regular table sugar (sucrose). What is fructose malabsorption? Some people cannot completely absorb fructose in the small intestine. When fructose is not absorbed it is quickly consumed by the bacteria that normally live in the gut. The result is abdominal bloating, cramping, gas, diarrhea, and/or constipation. Fructose malabsorption can occur in people with Irritable Bowel Syndrome (IBS) and other gastrointestinal (GI) disorders. It is diagnosed with a fructose hydrogen breath test and the treatment is a low fructose diet. What foods should I avoid? You do not have to avoid all foods that contain fructose, only those that are high in excess fructose listed below. Excess fructose means that the food has more than half of its natural sugar as fructose. Glucose is the other simple sugar found in these foods which helps absorb fructose in the small intestine. The more glucose than fructose in a food, the more “gut-friendly” it is. Avoid these high fructose foods: Fruit: apple, pear, Asian pear, watermelon, fig, mango, cherries Vegetables: artichokes, sugar snap peas, asparagus Sweeteners: honey, agave, high fructose corn syrup (HFCS), fruit juice concentrate of the above fruits, and large amounts of sucrose (white or brown sugar) UMHS Division of Gastroenterology - 1 - Beverages: juices of the fruit listed above, regular soda and drinks that are sweetened with fructose or HFCS, rum General guidelines: Read labels and avoid products that contain fructose, crystalline fructose, HFCS, honey, agave, and fruit juice concentrates (i.e. -

Fructose Intolerance in IBS and Utility of Fructose-Restricted Diet Young K
ORIGINAL ARTICLE Fructose Intolerance in IBS and Utility of Fructose-Restricted Diet Young K. Choi, MD,* Nancy Kraft, RD, LD,w Bridget Zimmerman, PhD,z Michelle Jackson,w and Satish S. C. Rao, MD, PhD, FRCPw ructose is naturally present in fruits and vegetables, Introduction: Whether dietary fructose intolerance causes Fbut today it is avidly consumed in beverages and symptoms of irritable bowel syndrome (IBS) is unclear. We canned products as high fructose corn syrup.1 In the examined the prevalence of fructose intolerance in IBS and long- United States, the consumption of fructose has increased term outcome of fructose-restricted diet. several fold during the last 2 decades. A United States Methods: Two hundred and nine patients with suspected IBS Department of Agriculture study estimated that the annual consumption of fructose has risen from less than were retrospectively evaluated for organic illnesses. Patients 2 with IBS (Rome II) and positive fructose breath test received a ton in 1966 to 8.8 million tons in 2003. Unlike other instructions regarding fructose-restricted diet. One year later, sugars such as sucrose or lactose which are digested by their symptoms, compliance with, and effects of dietary sucrase or lactase enzymes produced by the intestinal brush border, the gut does not appear to have a specific modification on lifestyle were assessed using a structured 3,4 interview. enzyme for digesting or transporting fructose. Recent studies have shown that GLUT-5 and GLUT-2 which Results: Eighty patients (m/f = 26/54) fulfilled Rome II criteria. actively transport glucose across the mucosa may also Of 80 patients, 31 (38%) had positive breath test. -

Fructose Malabsorption in Asymptomatic Children and in Patients with Functional Chronic Abdominal Pain: a Prospective Comparative Study
European Journal of Pediatrics https://doi.org/10.1007/s00431-019-03418-4 ORIGINAL ARTICLE Fructose malabsorption in asymptomatic children and in patients with functional chronic abdominal pain: a prospective comparative study Oihana Martínez-Azcona1 & Ana Moreno-Álvarez 2 & Teresa Seoane-Pillado3 & Inés Niño-Grueiro4 & Ana Ramiro-Comesaña4 & María Menéndez-Riera4 & Marta Pérez-Domínguez4 & Alfonso Solar-Boga2 & Rosaura Leis-Trabazo5 Received: 6 February 2019 /Revised: 18 June 2019 /Accepted: 19 June 2019 # Springer-Verlag GmbH Germany, part of Springer Nature 2019 Abstract The objective of this prospective cohort study was to compare fructose malabsorption in patients with functional chronic abdominal pain and in healthy children. The sample was divided into two groups: asymptomatic children and pain- predominant functional gastrointestinal disorders according to the Rome IV criteria. All children were tested for fructose malabsorption by a standardized breath hydrogen test. Hydrogen and methane were measured and the test was presumed positive when it exceeded 20 ppm above baseline. If positive, patients were given a low-fructose diet and the response was evaluated. One hundred five children were included (34 healthy children, 71 with functional chronic abdominal pain), with similar demographic characteristics in both groups (35.2% male, age 9.5 ± 2.8 years). Hydrogen levels in breath were tested through a hydrogen test for fructose demonstrating malabsorption in 58.8% of healthy children (95%CI 40.8%–76.8%) and in 40.8% of children with chronic abdominal pain (95%CI 28.7%–53.0%), removing those who had bacterial overgrowth. Twenty-one of 31 patients with symptoms and a positive test (72.4%) reported an improvement on a low-fructose diet. -

Gas and Diet
Gas and Diet The body produces gas in the stomach and intestines during the normal digestion of food. Swallowed air also causes gas. Rapid introduction of any high-fiber foods to the diet will lead to gas. If you want to begin eating a higher-fiber diet, begin slowly and make sure you drink plenty of fluids. The following foods and beverages are the ones most likely to cause gas. Vegetables • Cabbage • Sauerkraut • Brussels sprouts • Broccoli • Asparagus • Artichokes • Eggplant • Radishes • Cauliflower • Cucumbers • Peas • Celery • Carrots • Onions • Rutabaga • Turnips Fruits • Apples • Pears • Melons • Peaches • Bananas • Apricots • Raisins • Prune juice • Citrus fruits • Fruit juices Other foods • Dried beans, peas, and lentils • Whole grains • Most starches, including potatoes, corn, pasta, and wheat • Foods containing sugar alcohols, such as sorbitol or xylitol • Carbonated beverages • Beer • Red wine • Eggs • High-fat diets (tend to cause more gas because the gas does not move into the small intestine for a longer period of time after eating) • Fructose, if a person malabsorbs fructose* • Lactose, if a person is lactose intolerant (common cause of gas)* *If you believe you are not digesting fructose or lactose correcting, speak with your health care professional, who may request a breath test. Foods to avoid You do not need to avoid all of the foods just listed. Many of the foods that lead to gas formation are the healthiest foods. The best idea is to figure out which foods you started eating more of before you got excessive gas. Eliminate them from the diet, and then slowly add them back into your diet, one at a time, to help you figure out which food is the culprit. -

Irritable Bowel Syndrome: Clinical Manifestations, Dietary Influences, and Management
Rowan University Rowan Digital Works Cooper Medical School of Rowan University Faculty Scholarship Cooper Medical School of Rowan University 4-26-2017 Irritable Bowel Syndrome: Clinical Manifestations, Dietary Influences, and Management. Ronald Ikechi Bradford D Fischer Joshua DeSipio Sangita Phadtare Follow this and additional works at: https://rdw.rowan.edu/cmsru_facpub Part of the Medicine and Health Sciences Commons Recommended Citation Ikechi R, Fischer BD, DeSipio J, Phadtare S. Irritable Bowel Syndrome: Clinical Manifestations, Dietary Influences, and Management. Healthcare. 2017; 5(2):21. https://doi.org/10.3390/healthcare5020021 This Article is brought to you for free and open access by the Cooper Medical School of Rowan University at Rowan Digital Works. It has been accepted for inclusion in Cooper Medical School of Rowan University Faculty Scholarship by an authorized administrator of Rowan Digital Works. healthcare Review Irritable Bowel Syndrome: Clinical Manifestations, Dietary Influences, and Management Ronald Ikechi 1, Bradford D. Fischer 1, Joshua DeSipio 2 and Sangita Phadtare 1,* 1 Department of Biomedical Sciences, Cooper Medical School of Rowan University, Camden, NJ 08103, USA; [email protected] (R.I.); fi[email protected] (B.D.F.) 2 Department of Medicine, Gastroenterology/Liver Diseases Division, Cooper Medical School of Rowan University, Camden, NJ 08103, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-856-956-2791 Academic Editor: Sampath Parthasarathy Received: 23 December 2016; Accepted: 18 April 2017; Published: 26 April 2017 Abstract: Irritable bowel syndrome (IBS) is a functional gastrointestinal disorder that is characterized by symptoms of chronic abdominal pain and altered bowel habits in the absence of an overtly identifiable cause. -

How Common Is Celiac Disease?
FAQ – General What is celiac disease? How common is celiac disease? Who gets celiac disease? What are the symptoms of celiac disease? When does celiac disease usually develop? What is the difference between celiac disease, gluten intolerance, and wheat or gluten allergy? When will I feel better? Are there any concerns about pregnancy and celiac disease? Are there any unique considerations for children with celiac disease, or children of celiac disease patients? How does having a problem with candida affect celiac disease (CD)? Are high eosinophil levels connected to celiac disease (CD) and/or allergies (such as pollen, mold, mildew and dust mites) or asthma? Can a person with celiac disease donate blood? What is celiac disease? Celiac disease is an autoimmune disorder. In people with celiac disease, the body responds to gluten, the protein that comes from certain grains, by causing damage to the small intestine. Specifically, the body's immune system reacts to the gluten by causing inflammation of the lining of the small intestine, leading to malnutrition and other conditions. Other terms for celiac disease are celiac sprue, non-tropical sprue, and gluten-sensitive enteropathy. Classically, the disease is described by villous atrophy (a wasting away of intestinal villi), malabsorptive symptoms like steatorrhea (fat globules in the bowel movement), weight loss, or nutritional deficiencies (like low levels of iron or calcium), and a resolution of symptoms and intestinal damage after stopping the ingestion of gluten-containing foods. Looking under a microscope you would see a loss in height of the villi (finger-like projections in the intestine which are important for digestion).