Safe and Effective Pain Control After Surgery Brochure
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medications to Treat Opioid Use Disorder Research Report
Research Report Revised Junio 2018 Medications to Treat Opioid Use Disorder Research Report Table of Contents Medications to Treat Opioid Use Disorder Research Report Overview How do medications to treat opioid use disorder work? How effective are medications to treat opioid use disorder? What are misconceptions about maintenance treatment? What is the treatment need versus the diversion risk for opioid use disorder treatment? What is the impact of medication for opioid use disorder treatment on HIV/HCV outcomes? How is opioid use disorder treated in the criminal justice system? Is medication to treat opioid use disorder available in the military? What treatment is available for pregnant mothers and their babies? How much does opioid treatment cost? Is naloxone accessible? References Page 1 Medications to Treat Opioid Use Disorder Research Report Discusses effective medications used to treat opioid use disorders: methadone, buprenorphine, and naltrexone. Overview An estimated 1.4 million people in the United States had a substance use disorder related to prescription opioids in 2019.1 However, only a fraction of people with prescription opioid use disorders receive tailored treatment (22 percent in 2019).1 Overdose deaths involving prescription opioids more than quadrupled from 1999 through 2016 followed by significant declines reported in both 2018 and 2019.2,3 Besides overdose, consequences of the opioid crisis include a rising incidence of infants born dependent on opioids because their mothers used these substances during pregnancy4,5 and increased spread of infectious diseases, including HIV and hepatitis C (HCV), as was seen in 2015 in southern Indiana.6 Effective prevention and treatment strategies exist for opioid misuse and use disorder but are highly underutilized across the United States. -

The Opioid Epidemic: What Labs Have to Do with It?
The Opioid Epidemic: What labs have to do with it? Ewa King, Ph.D. Associate Director of Health RIDOH State Health Laboratories Analysis. Answers. Action. www.aphl.org Overview • Overdose trends • Opioids and their effects • Analytical testing approaches • Toxicology laboratories Analysis. Answers. Action. www.aphl.org Opioid overdose crisis 1 Analysis. Answers. Action. www.aphl.org Opioid overdose crisis 2 Analysis. Answers. Action. www.aphl.org Opiates and Opioids • Opiates vs. Opioids • Opiates: Naturally occurring, derived from the poppy plant • Opioids: “Opiate-like” drugs in effects, not chemical structure Includes opiates • Narcotic analgesics • CNS depressants • DEA Schedule I or II controlled substances • Additive effect with other CNS depressant drugs Analysis. Answers. Action. www.aphl.org Efficacy of Opioids • How do opioids work? • Bind with opioid receptors • Brain, spinal cord, GI tract, and throughout the body • Pain, emotion, breathing, movement, and digestion Opioid Receptor Analysis. Answers. Action. www.aphl.org Effects of Opioids Physiological Psychological • Pain relief • Drowsiness/ sedation • Cough suppression • Mental confusion • GI motility • Loss of memory • Respiratory depression • Lethargy/ apathy • Pupillary constriction • Euphoria/ tranquility • Itching • Mood swings • Constipation • Depression • Dependence • Withdrawal • Dependence Analysis. Answers. Action. www.aphl.org Opiates 1 Opiates • Naturally occurring alkaloids Opium • Latex from the opium poppy plant Codeine: • Mild to moderate pain • Antitussive Morphine: • Severe pain • Metabolite of codeine and heroin Analysis. Answers. Action. www.aphl.org Opiates 2 Semi-synthetic Opiates: • Synthesized from a natural opiate Heroin: • Schedule I narcotic Hydrocodone (Vicodin): • Mild to moderate pain • Metabolizes to hydromorphone (Dilaudid) Oxycodone (Oxycontin/Percocet): • Moderate to severe pain • Metabolizes to oxymorphone (Opana) Analysis. Answers. Action. -
Update on the Management of Pain, Agitation, and Delirium in the ICU
Update on the Management of Pain, Agitation, and Delirium in the ICU Kevin E. Anger, Pharm.D., BCPS Gilles Fraser, Pharm.D., MCCM Paul M. Szumita, Pharm.D., BCCCP, Manager Investigational Drug Clinical Pharmacist in Critical BCPS, FCCM Service Brigham and Women’s Care Clinical Pharmacy Practice Manager Hospital Maine Medical Center Brigham and Women’s Hospital Boston, Massachusetts Portland, Maine Boston, Massachusetts Disclosures • Faculty have nothing to disclose. Objectives • Describe recent literature on management of pain, agitation, and delirium (PAD) in the intensive care unit (ICU). • Apply key concepts in the selection of sedatives, analgesics, and antipsychotic agents in critically ill patients. • Recommend methods to overcome key barriers to optimizing pain, sedation, and delirium pharmacotherapy in critically ill patients. Case-Based Approach to Pain Management in the ICU Kevin E. Anger, Pharm.D., BCPS Manager Investigational Drug Service Brigham and Women’s Hospital Boston, Massachusetts Time for a Poll How to vote via the web or text messaging From any browser From a text message Pollev.com/ashp 22333 152964 How to vote via text message How to vote via the web Question #1 DT is a 70 yo male w/ COPD, S/P XRT for NSC lung CA, now admitted to the medical ICU for respiratory failure secondary to pneumonia meeting ARDS criteria. Significant home medications include oxycodone sustained release 40mg TID, oxycodone 10- 20mg Q4hrs PRN pain, Advair 500/50mcg BID, ASA 81mg QD, and albuterol neb Q4hrs PRN. DT is intubated is currently -

Pharmacists' Roles on the Pain Management Team, Fall 2014
Fall 2014, Volume 8, Issue 2 Canadian Pharmacy > Research > Health Policy > Practice > Better Health Pharmacists’ Roles on the Pain Management Team harmacists are an important resource for managing pain in their patients, in order to both optimize treatment and Pprevent the unintended consequences of potent analgesics. While the role of pharmacists in pain management was first addressed inthe Translator Summer 2012 edition1, this rapidly evolving area of pharmacy practice has generated a number of innovative models that highlight the unique role of the pharmacist. As Canadian pharmacists embrace expanded scopes of practice, there is an opportunity to specifically leverage their services to assist patients in managing their pain. This issue of the Translator highlights four different approaches to enhanced involvement of pharmacists in the management of chronic pain: n Pharmacist-led management of chronic pain: a randomized controlled exploratory trial from the UK n A pharmacist-initiated intervention trial in osteoarthritis n A pharmacist-led pain consultation for patients with concomitant substance use disorders n The impact of pharmacists in translating evidence to patients with low back pain 1 The Translator, Summer 2012, 6:3 Pharmacist-led management of chronic pain in primary care: results from a randomized controlled exploratory trial Bruhn H, Bond CM, Elliott AM, et al. Pharmacist-led management of chronic pain in primary care; results from a randomized controlled exploratory trial. BMJ Open 2013;3:e002361. Issue: In the UK, an estimated 80% of medication review of each patient’s medical chronic pain sufferers still report pain after Pharmacist prescribing and records, followed by a face-to-face consul- four years of follow-up.1 Most patients refer reviewing pain medication may tation. -

Pain Management in People Who Have OUD; Acute Vs. Chronic Pain
Pain Management in People Who Have OUD; Acute vs. Chronic Pain Developer: Stephen A. Wyatt, DO Medical Director, Addiction Medicine Carolinas HealthCare System Reviewer/Editor: Miriam Komaromy, MD, The ECHO Institute™ This project is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under contract number HHSH250201600015C. This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government. Disclosures Stephen Wyatt has nothing to disclose Objectives • Understand the complexities of treating acute and chronic pain in patients with opioid use disorder (OUD). • Understand the various approaches to treating the OUD patient on an agonist medication for acute or chronic pain. • Understand how acute and chronic pain can be treated when the OUD patient is on an antagonist medication. Speaker Notes: The general Outline of the module is to first address the difficulties surrounding treating pain in the opioid dependent patient. Then to address the ways that patients with pain can be approached on either an agonist of antagonist opioid use disorder treatment. Pain and Substance Use Disorder • Potential for mutual mistrust: – Provider • drug seeking • dependency/intolerance • fear – Patient • lack of empathy • avoidance • fear Speaker Notes: It is the provider that needs to be well educated and skillful in working with this population. Through a better understanding of opioid use disorders as a disease, the prejudice surrounding the encounter with the patient may be reduced. -

ACT Early Milestone Moments
Milestone Moments Learn the Signs. Act Early. Learn the Signs. Act Early. www.cdc.gov/milestones 1-800-CDC-INFO Adapted from CARING FOR YOUR BABY AND YOUNG CHILD: BIRTH TO AGE 5, Fifth Edition, edited by Steven Shelov and Tanya Remer Altmann © 1991, 1993, 1998, 2004, 2009 by the American Academy of Pediatrics and You can follow your child’s development by watching how he or BRIGHT FUTURES: GUIDELINES FOR HEALTH SUPERVISION OF INFANTS, CHILDREN, AND ADOLESCENTS, Third she plays, learns, speaks, and acts. Edition, edited by Joseph Hagan, Jr., Judith S. Shaw, and Paula M. Duncan, 2008, Elk Grove Village, IL: American Academy of Pediatrics. Special acknowledgements to Susan P. Berger, PhD; Jenny Burt, PhD; Margaret Greco, MD; Katie Green, MPH, Look inside for milestones to watch for in your child and how you CHES; Georgina Peacock, MD, MPH; Lara Robinson, PhD, MPH; Camille Smith, MS, EdS; Julia Whitney, BS; and can help your child learn and grow. Rebecca Wolf, MA. Centers for Disease Centers for Disease Control and Prevention Control and Prevention www.cdc.gov/milestones www.cdc.gov/milestones 1-800-CDC-INFO 1-800-CDC-INFO 220788 Milestone Moments How your child plays, learns, speaks, and acts offers important clues about your child’s development. Developmental milestones are things most children can do by a certain age. The lists that follow have milestones to look for when your child is: 2 Months ............................................................... page 3 – 6 Check the milestones your child has reached at each age. 4 Months ............................................................... page 7 –10 Take this with you and talk with your child’s doctor at every visit about the milestones your child has reached and what to 6 Months .............................................................. -

The Opioid Crisis and the Black/African American Population: an Urgent Issue
THE OPIOID CRISIS AND THE BLACK/AFRICAN AMERICAN POPULATION: AN URGENT ISSUE THE OPIOID CRISIS AND THE BLACK/AFRICAN AMERICAN POPULATION: AN URGENT ISSUE U.S. Department of Health and Human Services Substance Abuse and Mental Health Services Administration Office of Behavioral Health Equity Table of Contents Introduction ...................................................................................................................................................... 3 i. Purpose of the Issue Brief ........................................................................................................................ 3 ii. Sources of Information ............................................................................................................................ 4 Opioids in Black/African American Communities: Context .................................................................. 4 i. What Do the National Data Show? ........................................................................................................ 4 ii. Routes to Opioid Misuse and Overdose Deaths: Pain Management, Illicit Drug Use, and Opioid Comorbidities in Black/African American Communities .................................................... 6 iii. Challenges to Prevention, Treatment, and Recovery .......................................................................... 7 Strategies to Address Opioid Misuse and OUD in Black/African American Communities ............ 9 i. Standard Treatment ................................................................................................................................ -

Perioperative Pain Management for the Chronic Pain Patient with Long-Term Opioid Use
1.5 ANCC Contact Hours Perioperative Pain Management for the Chronic Pain Patient With Long-Term Opioid Use Carina Jackman In the United States nearly one in four patients present- patterns of preoperative opioid use. Approximately one ing for surgery reports current opioid use. Many of these in four patients undergoing surgery in the study re- patients suffer from chronic pain disorders and opioid ported preoperative opioid use (23.1% of the 34,186-pa- tolerance or dependence. Opioid tolerance and preexisting tient study population). Opioid use was most common chronic pain disorders present unique challenges in regard in patients undergoing orthopaedic spinal surgery to postoperative pain management. These patients benefi t (65%). This was followed by neurosurgical spinal sur- geries (55.1%). Hydrocodone bitartrate was the most from providers who are not only familiar with multimodal prevalent medication. Tramadol and oxycodone hydro- pain management and skilled in the assessment of acute pain, chloride were also common ( Hilliard et al., 2018 ). but also empathetic to their specifi c struggles. Chronic pain Given this signifi cant population of surgical patients patients often face stigmas surrounding their opioid use, with established opioid use, it is imperative for both and this may lead to underestimation and undertreatment nurses and all other providers to gain an understanding of their pain. This article aims to review the challenges of the complex challenges chronic pain patients intro- presented by these complex patients and provide strate- duce to the postoperative setting. gies for treating acute postoperative pain in opioid-tolerant patients. Defi nitions Common pain terminology as defined by the Chronic Pain and Long-Term International Association for the Study of Pain, a joint Opioid Use consensus statement by the American Society of Addiction Medicine, the American Academy of Pain The burden of chronic pain in the United States is stag- Medicine and the American Pain Society (2001 ), and the gering. -

Phencyclidine: an Update
Phencyclidine: An Update U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES • Public Health Service • Alcohol, Drug Abuse and Mental Health Administration Phencyclidine: An Update Editor: Doris H. Clouet, Ph.D. Division of Preclinical Research National Institute on Drug Abuse and New York State Division of Substance Abuse Services NIDA Research Monograph 64 1986 DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Alcohol, Drug Abuse, and Mental Health Administratlon National Institute on Drug Abuse 5600 Fishers Lane Rockville, Maryland 20657 For sale by the Superintendent of Documents, U.S. Government Printing Office Washington, DC 20402 NIDA Research Monographs are prepared by the research divisions of the National lnstitute on Drug Abuse and published by its Office of Science The primary objective of the series is to provide critical reviews of research problem areas and techniques, the content of state-of-the-art conferences, and integrative research reviews. its dual publication emphasis is rapid and targeted dissemination to the scientific and professional community. Editorial Advisors MARTIN W. ADLER, Ph.D. SIDNEY COHEN, M.D. Temple University School of Medicine Los Angeles, California Philadelphia, Pennsylvania SYDNEY ARCHER, Ph.D. MARY L. JACOBSON Rensselaer Polytechnic lnstitute National Federation of Parents for Troy, New York Drug Free Youth RICHARD E. BELLEVILLE, Ph.D. Omaha, Nebraska NB Associates, Health Sciences Rockville, Maryland REESE T. JONES, M.D. KARST J. BESTEMAN Langley Porter Neuropsychiatric lnstitute Alcohol and Drug Problems Association San Francisco, California of North America Washington, D.C. DENISE KANDEL, Ph.D GILBERT J. BOTV N, Ph.D. College of Physicians and Surgeons of Cornell University Medical College Columbia University New York, New York New York, New York JOSEPH V. -

The Impact of Cannabis Access Laws on Opioid Prescribing
Journal of Health Economics 69 (2020) 102273 Contents lists available at ScienceDirect Journal of Health Economics j ournal homepage: www.elsevier.com/locate/econbase The impact of cannabis access laws on opioid prescribing a,∗ b c Benjamin J. McMichael , R. Lawrence Van Horn , W. Kip Viscusi a Assistant Professor of Law, University of Alabama School of Law, Box 870382, 101 Paul W. Bryant Drive East, Tuscaloosa, AL, 35487, United States b Associate Professor of Management and Law, Executive Director of Health Affairs, Owen Graduate School of Management, Vanderbilt University, 401 21st Avenue South, Nashville, TN, 37203, United States c University Distinguished Professor of Law, Economics, and Management, Vanderbilt University Law School. 131 21st Avenue South, Nashville, TN, 37203, United States a r a t i c l e i n f o b s t r a c t Article history: While recent research has shown that cannabis access laws can reduce the use of prescrip- Received 5 October 2018 tion opioids, the effect of these laws on opioid use is not well understood for all dimensions Received in revised form 17 July 2019 of use and for the general United States population. Analyzing a dataset of over 1.5 bil- Accepted 7 December 2019 lion individual opioid prescriptions between 2011 and 2018, which were aggregated to the Available online 14 December 2019 individual provider-year level, we find that recreational and medical cannabis access laws reduce the number of morphine milligram equivalents prescribed each year by 11.8 and 4.2 JEL classification: percent, respectively. These laws also reduce the total days’ supply of opioids prescribed, I180 the total number of patients receiving opioids, and the probability a provider prescribes K19 any opioids net of any offsetting effects. -

Menu of Pain Management Clinic Regulation
Menu of Pain Management Clinic Regulation The United States is in the midst of an unprecedented epidemic of prescription drug overdose deaths.1 More than 38,000 people died of drug overdoses in 2010, and most of these deaths (22,134) were caused by overdoses involving prescription drugs.2 Three-quarters of prescription drug overdose deaths in 2010 (16,651) involved a prescription opioid pain reliever (OPR), which is a drug derived from the opium poppy or synthetic versions of it such as oxycodone, hydrocodone, or methadone.3 The prescription drug overdose epidemic has not affected all states equally, and overdose death rates vary widely between states. States have the primary responsibility to regulate and enforce prescription drug practice. Although state laws are commonly used to prevent injuries and their benefits have been demonstrated for a variety of injury types,4 there is little information on the effectiveness of state statutes and regulations designed to prevent prescription drug abuse and diversion. This menu is a first step in assessing pain management clinic laws by creating an inventory of state legal strategies in this domain. Introduction One type of law aimed at preventing inappropriate prescribing is regulation of pain management clinics, often called “pill mills” when they are sources of large quantities of prescriptions. Pill mills have become an increasing problem in the prescription drug epidemic, and laws have been enacted to prevent these facilities from prescribing controlled substances inappropriately. A law was included in this resource as a pain management clinic regulation if it requires state oversight and contains other requirements concerning ownership and operation of pain management clinics, facilities, or practice locations. -
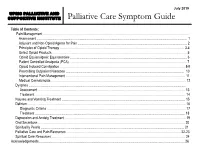
Palliative Care Symptom Guide
July 2019 UPMC PALLIATIVE AND SUPPORTIVE INSTITUTE Palliative Care Symptom Guide Table of Contents: Pain Management ……………………………………………………………………………………………………………………….. Assessment …………………………………………………………………………………………………………………………… 1 Adjuvant and Non-Opioid Agents for Pain ……………………………………………………………………………………….... 2 Principles of Opioid Therapy ……………………………………………………………………………………………….….…. 3-4 Select Opioid Products ……………………………………………………………………………………………………………… 5 Opioid Equianalgesic Equivalencies ………………………………………………………………………...…………………..… 6 Patient Controlled Analgesia (PCA) ……………………………………………………………………………………………….. 7 Opioid Induced Constipation ……………………………………………………………………………………………………… 8-9 Prescribing Outpatient Naloxone ………………………………………………………………………………………………… 10 Interventional Pain Management …………………………………………………………………………………………………. 11 Medical Cannabinoids ……………………………………………………………………………………………………………… 12 Dyspnea ………………………………………………………………………………………………………………………………… Assessment ………………………………………………………………………………………………………………………… 13 Treatment …………………………………………………………………………………………………………………………… 14 Nausea and Vomiting Treatment ……………………………………………………………………………………………..……… 15 Delirium …………………………………………………………………………………………………………………………………. 16 Diagnostic Criteria ……………………………………………………………………………….……………………….………... 17 Treatment ………………………………………………………………………………..…………………………………………. 18 Depression and Anxiety Treatment ……………………………………………………..…………..…………………………….…. 19 Oral Secretions ……………………………………………………..…………………………………………………………………. 20 Spirituality Pearls ……………………………………………………..………………………………………………………………. 21 Palliative