Download Download
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Journal of Pharmaceutical and Scientific Innovation
Anuradha B et al: J. Pharm. Sci. Innov. 2019; 8(5) Journal of Pharmaceutical and Scientific Innovation www.jpsionline.com (ISSN : 2277 –4572) Research Article JIHWA PAREEKSHA IN SAAMA AVASTHA OF AMLAPITTA: A CLINICAL STUDY Anuradha B 1*, Ajantha 2, Anjana3, Geetha Nayak S 1 1Final year PG Scholar, Department of Roga Nidana & Vikruti Vignana, Sri Dharmasthala Manjunatheshwara College of Ayurveda and Hospital, Hassan, India 2Professor, Department of Roga Nidana & Vikruti Vignana, Sri Dharmasthala Manjunatheshwara College of Ayurveda and Hospital, Hassan, India 3Final year PG Scholar, Department of Swasthavritta & Yoga, Sri Dharmasthala Manjunatheshwara College of Ayurveda and Hospital, Hassan *Corresponding Author Email: [email protected] DOI: 10.7897/2277-4572.085149 Received on: 15/06/19 Revised on: 12/07/19 Accepted on: 17/07/19 ABSTRACT Ayurveda emphasizes agni-vaishamya as a cause of manifestation of vyadhi (disease). The undigested food due to vitiated agni results in apakwa-ahara-rasa, that does not get absorbed and transformed is termed as ama, is said to be root cause for diseases. Ama combines with dosha to form amadosha that acquires more shuktatva, further forming amavisha, paving to varied manifestations in diseases. Therefore, analyzing saama and niramavastha is essential for better diagnosis and management. Amlapitta, one among the annavaha-sroto-vikara manifests due to agni-vaishamya. Jihwa pareeksha (tongue examination) plays an important role to assess various changes in jihwa. It reflects the status of annavaha-srotas and ama. Thus, the present study aims at observation of manifestations on jihwa (tongue) by jihwa pareeksha in saama avastha of Amlapitta. Patients of Amlapitta were screened and subjected for jihwa pareeksha. -

S. No. Name of the Ayurveda Medical Colleges
S. NO. NAME OF THE AYURVEDA MEDICAL COLLEGES Dr. BRKR Govt Ayurvedic CollegeOpp. E.S.I Hospital, Erragadda 1. Hyderabad-500038 Andhra Pradesh Dr.NR Shastry Govt. Ayurvedic College, M.G.Road,Vijayawada-520002 2. Urban Mandal, Krishna District Andhra Pradesh Sri Venkateswara Ayurvedic College, 3. SVIMS Campus, Tirupati North-517507Andhra Pradesh Anantha Laxmi Govt. Ayurvedic College, Post Laxmipura, Labour Colony, 4. Tq. & Dist. Warangal-506013 Andhra Pradesh Government Ayurvedic College, Jalukbari, Distt-Kamrup (Metro), 5. Guwahati- 781014 Assam Government Ayurvedic College & Hospital 6. Kadam Kuan, Patna 800003 Bihar Swami Raghavendracharya Tridandi Ayurved Mahavidyalaya and 7. Chikitsalaya,Karjara Station, PO Manjhouli Via Wazirganj, Gaya-823001Bihar Shri Motisingh Jageshwari Ayurved College & Hospital 8. Bada Telpa, Chapra- 841301, Saran Bihar Nitishwar Ayurved Medical College & HospitalBawan Bigha, Kanhauli, 9. P.O. RamanaMuzzafarpur- 842002 Bihar Ayurved MahavidyalayaGhughari Tand, 10. Gaya- 823001 Bihar Dayanand Ayurvedic Medical College & HospitalSiwan- 841266 11. Bihar Shri Narayan Prasad Awathy Government Ayurved College G.E. Road, 12. Raipur- 492001 Chhatisgarh Rajiv Lochan Ayurved Medical CollegeVillage & Post- 13. ChandkhuriGunderdehi Road, Distt. Durg- 491221 Chhatisgarh Chhatisgarh Ayurved Medical CollegeG.E. Road, Village Manki, 14. Dist.-Rajnandgaon 491441 Chhatisgarh Shri Dhanwantry Ayurvedic College & Dabur Dhanwantry Hospital 15. Plot No.-M-688, Sector 46-B Chandigarh- 160017 Ayurved & Unani Tibbia College and HospitalAjmal Khan Road, Karol 16. Bagh New Delhi-110005 Chaudhary Brahm Prakesh Charak Ayurved Sansthan 17. Khera Dabur, Najafgarh, New Delhi-110073 Bharteeya Sanskrit Prabodhini, Gomantak Ayurveda Mahavidyalaya & Research Centre, Kamakshi Arogyadham Vajem, 18. Shiroda Tq. Ponda, Dist. North Goa-403103 Goa Govt. Akhandanand Ayurved College & Hospital 19. Lal Darvaja, Bhadra Ahmedabad- 380001 Gujarat J.S. -

Swavalamban Yojana
Presentation On for Subscribers PENSION A pension provides people with a monthly income when they are no longer earning. NEED FOR PENSION One is not as productive in the old age as in the young age. The rise of nuclear family –Migration of younger earning members. Rise in cost of living Increasing longevity Assured monthly income ensures dignified life in old age THE INDIAN PENSION STORY Prior to 2004 Only available to 12% of the population– mainly for government employees Eligible for Based on defined benefits Pension 3 After 2004 PFRDA has been established by the Government of India. Paradigm shift from Defined Benefit to Defined Contribution PFRDA has made Govt. of India’s available NPS option Swavalamban Scheme: to all citizens of India Special focus towards to avail pension Economically through NPS w.e.f 01st Disadvantaged and May, 2009 Unorganized Sector 4 NPS - SWAVALAMBAN YOJANA Government to contribute Rs.1000 to each NPS account If : Subscriber is not covered under any other social security schemes like PF, Pension – only self declaration is required NPS -Swavalamban account opened in year 2010-11 , 2011-12 , 2012-2013 will get the benefit for 5 yrs . NPS - Swavalamban account opened in 2013 –2014 and subsequent years till 2016-2017 will get the benefit up to 2016-2017. Annual contribution to be the range of Rs.1000-Rs.12000 5 NPS -SWAVALAMBAN YOJNA Catering to Unorganized Sector Special Focus on economically disadvantaged/marginal investors Easy entry through aggregator for opening NPS-Swavalamban account Ultra low charge structure • Account Opening – Rs 35 (One Time). -

List of Shortlisted Institutes for Full Survey 2019
List of Shortlisted Institutes for Full Survey 2019 Current Application Permanent Institute S.No Number Id Institute Name Region Institute State 1- A & M INSTITUTE OF COMPUTER & North- 1 4271191322 1-10575231 TECHNOLOGY West Punjab 1- A & M INSTITUTE OF MANAGEMENT AND North- 2 4261494300 1-11477181 TECHNOLOGY West Punjab 1- South- 3 4266342520 1-5305236 A M C . ENGINEERING COLLEGE West Karnataka 1- A R INSTITUTE OF MANAGEMENT & 4 4263354761 1-35645144 TECHNOLOGY Northern Uttar Pradesh 1- South- 5 4261153813 1-10850261 A S N PHARMACY COLLEGE Central Andhra Pradesh 1- South- 6 4262023721 1-2819951 A. J. INSTITUTE OF MANAGEMENT West Karnataka 1- 1- 7 4259173969 1524174547 A. P. SHAH INSTITUTE OF TECHNOLOGY Western Maharashtra 1- 1- South- 8 4261341262 399048571 A.A.N.M. & V.V.R.S.R. POLYTECHNIC Central Andhra Pradesh A.J.M.V.P.S., INSTITUTE OF HOTEL 1- MANAGEMENT AND CATERING 9 4259303314 1-12373983 TECHNOLOGY. Western Maharashtra 1- South- 10 4267249931 1-5220016 A.M.C. ENGINEERING COLLEGE West Karnataka 1- A.N.A COLLEGE OF ENGINEERING AND 11 4263362545 1-7162981 MANAGEMENT STUDIES Northern Uttar Pradesh 1- 1- A.P.GOVERNMENT INSTITUTE OF LEATHER South- 12 4263467276 463865741 TECHNOLOGY Central Telangana 1- 1- A.R COLLEGE OF ENGINEERING & 13 4260666745 452090031 TECHNOLOGY Southern Tamil Nadu 1- A.R.COLLEGE OF PHARMACY & G.H.PATEL 14 4259686586 1-5747631 INSTITUTE OF PHARMACY Central Gujarat 1- 15 4260511025 1-5883726 A.R.J INSTITUTE OF MANAGEMENT STUDIES Southern Tamil Nadu 1- North- 16 4261153304 1-5483831 A.S.GROUP OF INSTITUTIONS West -

By Greenark Industries
PALMVERA -• The Arecaware WE CARE TO CONSERVE! -• BY GREENARK INDUSTRIES OUR VISION WE WISH TO PROMOTE ECO-EDUCATION! Be aware and create awareness by choosing to use things that do NO harm to our nature! COMPANY PROFILE : 1. Name of the Industry : M/s GREENARK INDUSTRIES 2. Address : Registered Office : Greenark Industries 66, Silver Town, Gokul Road, HUBLI – 580 030 Works / Factory : Greenark Industries 5 – A/1, Hublikar’s Compound, Panchayat No. 229, Opp. HP Petrol Pump, Anchatgeri, Karwar Road, HUBLI – 580 024 3. Constitution : PROPRIETOR (WOMAN ENTREPRENEUR) 4. License : UAM # KR13B0006064 : GSTN – 29BNLPD5256J1ZM 5. Name of Proprietor : VRUSHALI DESHPANDE 6. Products : PALM VERA – ECO FRIENDLY PLATES ( ROUND / SQUARE / RECTANGLE / TRIANGLE / OVAL / TAILOR- MADE (Example – HEART / HEXAGON / BOAT), BOWLS, TRAYS, CUTLERY, ETC... 7. Product Application : Disposable tableware for Exports, Domestic, Corporates (Ex: ISO – 14001 Companies), Caterers, Individual end users (Picnic / Party / Ceremonies), Hospital Canteens (Lilavati), Industrial Canteens (Ex: Siemens, Tata Motors, IT Companies, Trusts (Dharmasthala, Tirupati, Shirdi, ISCKON), Flight Catering, Retails 7. Raw materials : ARECANUT LEAF SHEATHS from KARNATAKA – Yellapur, Sirsi, Siddapur, Mundgod, Hangal, Sagar, Hosadurga, Davangere, Shimoga, Tirthhalli, Chikmagalur. 8. Market : EXPORT, CORPORATE SECTORS GLOBALLY, NICHE SECTION OF NATURAL PRODUCT ENTHUSIASTS, INDIVIDUAL PARTY / EVENT ORGANISERS, HOTELIERS & DOMESTIC END USERS. INTRODUCTION : The Palm Vera Areca leaf products are being produced with sustainable resource, essentially meaning that the products are made from FALLEN LEAVES AND ARE 100% NATURAL, through eco-friendly process with stringent principle that NO CHEMICALS, LACQUERS, WAX OR ANY OTHER ADDITIVES USED. And making doubly sure it is acceptable to Earth when disposed qualifying to be 100% BIODEGRADABLE AND COMPOSTABLE. -
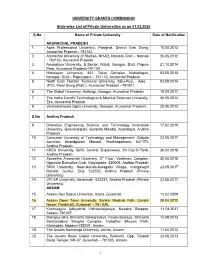
UNIVERSITY GRANTS COMMISSION State-Wise List of Private
UNIVERSITY GRANTS COMMISSION State-wise List of Private Universities as on 01.02.2020 S.No Name of Private University Date of Notification ARUNACHAL PRADESH 1. Apex Professional University, Pasighat, District East Siang, 10.05.2013 Arunachal Pradesh - 791102. 2. Arunachal University of Studies, NH-52, Namsai, Distt – Namsai 26.05.2012 - 792103, Arunachal Pradesh. 3. Arunodaya University, E-Sector, Nirjuli, Itanagar, Distt. Papum 21.10.2014 Pare, Arunachal Pradesh-791109 4. Himalayan University, 401, Takar Complex, Naharlagun, 03.05.2013 Itanagar, Distt – Papumpare – 791110, Arunachal Pradesh. 5. North East Frontier Technical University, Sibu-Puyi, Aalo 03.09.2014 (PO), West Siang (Distt.), Arunachal Pradesh –791001. 6. The Global University, Hollongi, Itanagar, Arunachal Pradesh. 18.09.2017 7. The Indira Gandhi Technological & Medical Sciences University, 26.05.2012 Ziro, Arunachal Pradesh. 8. Venkateshwara Open University, Itanagar, Arunachal Pradesh. 20.06.2012 S.No Andhra Pradesh 9. Bharatiya Engineering Science and Technology Innovation 17.02.2019 University, Gownivaripalli, Gorantla Mandal, Anantapur, Andhra Pradesh 10. Centurian University of Technology and Management, Gidijala 23.05.2017 Junction, Anandpuram Mandal, Visakhapatnam- 531173, Andhra Pradesh. 11. KREA University, 5655, Central, Expressway, Sri City-517646, 30.04.2018 Andhra Pradesh 12. Saveetha Amaravati University, 3rd Floor, Vaishnavi Complex, 30.04.2018 Opposite Executive Club, Vijayawada- 520008, Andhra Pradesh 13. SRM University, Neerukonda-Kuragallu Village, mangalagiri 23.05.2017 Mandal, Guntur, Dist- 522502, Andhra Pradesh (Private University) 14. VIT-AP University, Amaravati- 522237, Andhra Pradesh (Private 23.05.2017 University) ASSAM 15. Assam Don Bosco University, Azara, Guwahati 12.02.2009 16. Assam Down Town University, Sankar Madhab Path, Gandhi 29.04.2010 Nagar, Panikhaiti, Guwahati – 781 036. -

RTI Handbook
PREFACE The Right to Information Act 2005 is a historic legislation in the annals of democracy in India. One of the major objective of this Act is to promote transparency and accountability in the working of every public authority by enabling citizens to access information held by or under the control of public authorities. In pursuance of this Act, the RTI Cell of National Archives of India had brought out the first version of the Handbook in 2006 with a view to provide information about the National Archives of India on the basis of the guidelines issued by DOPT. The revised version of the handbook comprehensively explains the legal provisions and functioning of National Archives of India. I feel happy to present before you the revised and updated version of the handbook as done very meticulously by the RTI Cell. I am thankful to Dr.Meena Gautam, Deputy Director of Archives & Central Public Information Officer and S/Shri Ashok Kaushik, Archivist and Shri Uday Shankar, Assistant Archivist of RTI Cell for assisting in updating the present edition. I trust this updated publication will familiarize the public with the mandate, structure and functioning of the NAI. LOV VERMA JOINT SECRETARY & DGA Dated: 2008 Place: New Delhi Table of Contents S.No. Particulars Page No. ============================================================= 1 . Introduction 1-3 2. Particulars of Organization, Functions & Duties 4-11 3. Powers and Duties of Officers and Employees 12-21 4. Rules, Regulations, Instructions, 22-27 Manual and Records for discharging Functions 5. Particulars of any arrangement that exist for 28-29 consultation with or representation by the members of the Public in relation to the formulation of its policy or implementation thereof 6. -

Pilgrimage to Temples Dakshina Kannada
E-Book: for free circulation Pilgrimage to Temples In Dakshina Kannada By Tamarapu Sampath Kumaran About the Author: Mr T Sampath Kumaran is a freelance writer. He regularly contributes articles on Management, Business, Ancient Temples, and Temple Architecture to many leading Dailies and Magazines. His articles are popular in “The Young World section” of THE HINDU. His e- books on nature, environment and different cultures of people around the world are educative and of special interest to the young. His e-books – Guide to 108 Divya Desams, Guide to 275 Siva Sthalams, The Path of Ramanuja, Guide to Kancheepuram and Hinduism in a nutshell have been well received in the religious circle. He was associated in the renovation and production of two Documentary films on Nava Tirupathi Temples, and Tirukkurungudi Temple in Tamilnadu. Acknowledgement: I wish to express my gratitude to the authors from whose works I gathered the details for this book, and Courtesy, Google for some of the photographs. Special thanks to www.scribd.com for hosting my e-books. Introduction to Dakshina Kannada / SouthCanara. Dakshina Kannada, also called South Canara, is a coastal district of the Karnataka state. It is bordered by the districts of Udupi to the north, Chikkamagaluru to the northeast, Hassan District to the east, Kodagu to the southeast, and Kasaragod in Kerala to the south. The Arabian Sea bounds it on the west. Mangalore is the capital and chief city of the district. There is also the good presence of mountainous region in the state, with tea and coffee plantations. Dakshina Kannada and Udupi districts are often called Tulu Nadu, as Tulu is the majority language in the region. -

Consolidated List Private Universities
UNIVERSITY GRANTS COMMISSION State-wise List of Private Universities as on 06.08.2021 S.No Name of Private University Date of Notification ARUNACHAL PRADESH 1. Apex Professional University, Pasighat, District East Siang, 10.05.2013 Arunachal Pradesh - 791102. 2. Arunachal University of Studies, NH-52, Namsai, Distt – Namsai 26.05.2012 - 792103, Arunachal Pradesh. 3. Arunodaya University, E-Sector, Nirjuli, Itanagar, Distt. Papum 21.10.2014 Pare, Arunachal Pradesh-791109 4. Himalayan University, 401, Takar Complex, Naharlagun, 03.05.2013 Itanagar, Distt – Papumpare – 791110, Arunachal Pradesh. 5. North East Frontier Technical University, Sibu-Puyi, Aalo 03.09.2014 (PO), West Siang (Distt.), Arunachal Pradesh –791001. 6. The Global University, Hollongi, Itanagar, Arunachal Pradesh. 18.09.2017 7. The Indira Gandhi Technological & Medical Sciences University, 26.05.2012 Ziro, Arunachal Pradesh. 8. Venkateshwara Open University, Itanagar, Arunachal Pradesh. 20.06.2012 Andhra Pradesh 9. Bharatiya Engineering Science and Technology Innovation 17.02.2019 University, Gownivaripalli, Gorantla Mandal, Anantapur, Andhra Pradesh 10. Centurian University of Technology and Management, Gidijala 23.05.2017 Junction, Anandpuram Mandal, Visakhapatnam- 531173, Andhra Pradesh. 11. KREA University, 5655, Central, Expressway, Sri City-517646, 30.04.2018 Andhra Pradesh 12. Saveetha Amaravati University, 3rd Floor, Vaishnavi Complex, 30.04.2018 Opposite Executive Club, Vijayawada- 520008, Andhra Pradesh 13. SRM University, Neerukonda-Kuragallu Village, mangalagiri 23.05.2017 Mandal, Guntur, Dist- 522502, Andhra Pradesh (Private University) 14. VIT-AP University, Amaravati- 522237, Andhra Pradesh (Private 23.05.2017 University) ASSAM 15. Assam Don Bosco University, Azara, Guwahati 12.02.2009 16. Assam Down Town University, Sankar Madhab Path, Gandhi 29.04.2010 Nagar, Panikhaiti, Guwahati – 781 036. -

Journal of Pharmaceutical and Scientific Innovation
S Srinidhi et al: J. Pharm. Sci. Innov. 2018; 7(4) Journal of Pharmaceutical and Scientific Innovation www.jpsionline.com (ISSN : 2277 –4572) Review Article MADANAPHALA KALPAS: A REVIEW S Srinidhi *1, M Kumar Ashvini2, Gazala Hussain3, T Vidyavati4 , S Vasan Satish 1 1PG Scholar, Department of Panchakarma, Sri Dharmasthala Manjunatheshwara College of Ayurveda & Hospital, Hassan, Karnataka, India 2Professor and Head of Department of Panchakarma, Sri Dharmasthala Manjunatheshwara College of Ayurveda & Hospital, Hassan, Karnataka, India 3Associate Professor, Department of Rasashastra & Bhaishajya Kalpana, Sri Dharmasthala Manjunatheshwara College of Ayurveda & Hospital, Hassan, Karnataka, India 4PG Scholar, Department of Agada Tantra evum Vidhi Vaidyaka, Sri Dharmasthala Manjunatheswara College of Ayurveda & Hospital, Hassan, Karnataka, India *Corresponding Author Email: [email protected] DOI: 10.7897/2277-4572.07493 Received on: 01/08/18 Revised on: 19/08/18 Accepted on: 21/08/18 ABSTRACT Vamana (emetic therapy) is one among the panchakarma chikitsa (five eliminative therapies), where the morbid doshas are expelled through the oral cavity. Many vamaka yogas(emetics) have been mentioned in bruhatrayees (treatises of Ayurveda) in various forms of preparations. Madanaphala (emetic nut) is considered as best vamaka dravya (emetic drug). Many Madanaphala vamaka preparations like vati (pills), ghreya (inhalation), etc. have been mentioned in texts of Ayurveda. This review is an attempt to explore various yogas for vamana karma where madanaphala is used as the main ingredient. KEYWORDS: Madanaphala, vamana, yogas INTRODUCTION Paryaya (Synonyms) 5 Vamana karma (emetic therapy) is a procedure which is It has various synonyms and a few are as follows: Madana- it indicated in kapha pravrudha avastha (increased state of kapha) 1 causes mada (intoxication), Chardana- helps to induce vomiting, and urdhva jatrugata rogas (diseases of head, neck, throat, eyes, Pindeetaka- the fruit is spherical in shape, Shalyaka- has a lot of shoulder). -

'Indian Architecture' and the Production of a Postcolonial
‘Indian Architecture’ and the Production of a Postcolonial Discourse: A Study of Architecture + Design (1984-1992) Shaji K. Panicker B. Arch (Baroda, India), M. Arch (Newcastle, Australia) A Thesis Submitted to the University of Adelaide in fulfilment of the Requirements for the Degree of Doctor of Philosophy School of Architecture, Landscape Architecture and Urban Design Centre for Asian and Middle Eastern Architecture 2008 Table of Contents Abstract ............................................................................................................................................................................................iv Declaration ............................................................................................................................................................................................vi Acknowledgements..........................................................................................................................................................................vii List of Figures ........................................................................................................................................................................................ ix 1 Introduction ........................................................................................... 1 1.1: Overview..................................................................................................................................................................1 1.2: Background...........................................................................................................................................................2 -

Suryamitra Training Centres FY 2019-20
S.N State Suryamitra Training Centers for FY 2019-20 City Contact Email ID o. Number Training Training Center Partner 1 Andhra Centurion Gidijala Junction, Visakha 94370559 cree.vishakh Pradesh University of Anandpuram Mandal, patnam 55 apatnam@g Technology & Vishakhapatnam-531173 mail.com Management 2 Andhra Datapro datapro computers pvt ltd 47- Vishakh 80195537 cm.dwk@da Pradesh Computers Pvt. 9-10,2nd floor,subhadra apatna 77 tapro.in Ltd. complex,Nr.Diamond park,3rd m lane,DWARAKANAGAR, VISAKHAPATNAM-530016 3 Andhra Green Urja Green Urja Technologies & Guntur 99085566 sankartl@ya Pradesh Technology & systems (GUTS) C/o: 40 hoo.com Systems HMKS&MGS College of Engineering Kanagala, Guntur District Andhra Pradesh - 522259 4 Andhra IL&FS Skills IL&FS Institute of Skills @ Duttalu 99633344 R.purushoth Pradesh Development Duttalur, Rachavaripalli Road, r 36 am@ilfsindi Corporation Duttalur Vill & Mandal, SPSR a.com Ltd. Nellore, Andhrapradesh - 524222 5 Andhra PLNS Education 15/362, Mary Naidu Street, Nellore 79891997 isptvtnlr.pln Pradesh Pvt. Ltd. Subedarpet, Nellore - 87 [email protected] 524001 m 6 Andhra Surabhi Shabari Sai Pvt. ITI, Veldurthy Veldurt 97016882 sabarisaiiti@ Pradesh Educational hy 16 gmail.com Society 7 ANDHRA Syncroserve D.No.-44-1/2-1, Neon Plaza, Vijayaw 73961270 pmkk.vijaya PRADES Global Solutions Padalaveru, Machavaram ada 29 wada@sync H P Ltd Down, Eluru Road, hroserve.in Vijayawada, Andhra Pradesh- 520004 8 ANDHRA Syncroserve Ambati Mansion, 2nd Floor Guntur 91000645 pmkk.guntur PRADES Global Solutions above SBI, 4/15th