Cervical Radiculopathy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

UK Clinical Guideline for Best Practice in the Use of Vaginal Pessaries for Pelvic Organ Prolapse
UK Clinical Guideline for best practice in the use of vaginal pessaries for pelvic organ prolapse March 2021 Developed by members of the UK Clinical Guideline Group for the use of pessaries in vaginal prolapse representing: the United Kingdom Continence Society (UKCS); the Pelvic Obstetric and Gynaecological Physiotherapy (POGP); the British Society of Urogynaecology (BSUG); the Association for Continence Advice (ACA); the Scottish Pelvic Floor Network (SPFN); The Pelvic Floor Society (TPFS); the Royal College of Obstetricians and Gynaecologists (RCOG); the Royal College of Nursing (RCN); and pessary users. Funded by grants awarded by UKCS and the Chartered Society of Physiotherapy (CSP). This guideline was completed in December 2020, and following stakeholder review, has been given official endorsement and approval by: • British Association of Urological Nurses (BAUN) • International Urogynecological Association (IUGA) • Pelvic Obstetric and Gynaecological Physiotherapy (POGP) • Scottish Pelvic Floor Network (SPFN) • The Association of Continence Advice (ACA) • The British Society of Urogynaecology (BSUG) • The Pelvic Floor Society (TPFS) • The Royal College of Nursing (RCN) • The Royal College of Obstetricians and Gynaecologists (RCOG) • The United Kingdom Continence Society (UKCS) Review This guideline will be due for full review in 2024. All comments received on the POGP and UKCS websites or submitted here: [email protected] will be included in the review process. 2 Table of Contents Table of Contents ................................................................................................................................ -

Hand Gestures
L2/16-308 More hand gestures To: UTC From: Peter Edberg, Emoji Subcommittee Date: 2016-10-31 Proposed characters Tier 1: Two often-requested signs (ILY, Shaka, ILY), and three to complete the finger-counting sets for 1-3 (North American and European system). None of these are known to have offensive connotations. HAND SIGN SHAKA ● Shaka sign ● ASL sign for letter ‘Y’ ● Can signify “Aloha spirit”, surfing, “hang loose” ● On Emojipedia top requests list, but requests have dropped off ● 90°-rotated version of CALL ME HAND, but EmojiXpress has received requests for SHAKA specifically, noting that CALL ME HAND does not fulfill need HAND SIGN ILY ● ASL sign for “I love you” (combines signs for I, L, Y), has moved into mainstream use ● On Emojipedia top requests list HAND WITH THUMB AND INDEX FINGER EXTENDED ● Finger-counting 2, European style ● ASL sign for letter ‘L’ ● Sign for “loser” ● In Montenegro, sign for the Liberal party ● In Philippines, sign used by supporters of Corazon Aquino ● See Wikipedia entry HAND WITH THUMB AND FIRST TWO FINGERS EXTENDED ● Finger-counting 3, European style ● UAE: Win, victory, love = work ethic, success, love of nation (see separate proposal L2/16-071, which is the source of the information below about this gesture, and also the source of the images at left) ● Representation for Ctrl-Alt-Del on Windows systems ● Serbian “три прста” (tri prsta), symbol of Serbian identity ● Germanic “Schwurhand”, sign for swearing an oath ● Indication in sports of successful 3-point shot (basketball), 3 successive goals (soccer), etc. HAND WITH FIRST THREE FINGERS EXTENDED ● Finger-counting 3, North American style ● ASL sign for letter ‘W’ ● Scout sign (Boy/Girl Scouts) is similar, has fingers together Tier 2: Complete the finger-counting sets for 4-5, plus some less-requested hand signs. -

Palm Reading
Palm Reading Also known as palmistry or chiromancy, palm reading is practiced all over the world with roots in Indian astrology and gypsy fortune-telling. The objective is to evaluate a person’s character and aspects of their life by studying the palm of their hand. There is no substantiate evidence of correlation between palm features and psychological traits; palm reading is for entertainment purposes. Getting Started Which hand to read? There are two main practices: For males, the left hand is what you’re born with, and the right is what you’ve accumulated throughout your life. For females, it’s the opposite. Your dominant hand (the hand you use most often) determines your future and your other, non-dominant hand, is used to determine the past or hidden traits Take these into consideration when choosing which hand to read. Reading the Primary Lines of your Hand 1. Interpret the Heart Line This line is believed to indicate emotional stability, romantic perspectives, depression, and cardiac health. Begins below the index finger = content with love life Begins below the middle finger = selfish when it comes to love Begins in-between the middle and index fingers = caring and understanding Is straight and short = less interest in romance Touches life line = heart is broken easily Is long and curvy = freely expresses emotions and feelings Is straight and parallel to the head line = good handle on emotions Is wavy = many relationships, absence of serious relationships Circle on the line = sad or depressed Broken line = emotional trauma 2. Examine the Head Line This line represents learning style, communication style, intellectualism, and thirst for knowledge. -
Upper Extremity Impairment Rating Methodology and Case Presentation
Upper Extremity Impairment Rating Methodology and Case Presentation Dr. M. Alvi, PhD, PEng, MD, FRCSC To Rate or Not to Rate That is the Question! 2 Objectives Definition of terms The process of impairment evaluation using the AMA Guidelines Components of an impairment report Demonstrate ability to perform musculoskeletal impairment evaluations 3 Impairment ≠ Disability Disability Pain Impairment 4 JAMA Feb 15, 1958 12 other guides were published in the JAMA over the next twelve years. Of interest to us are the guide on the vascular system, published March 5, 1960, and the guide on the peripheral nervous system which was published July 13, 1964. Musculoskeletal System 5 Evolution of the Guides 1970 1980 1990 2000 2010 1st 2nd 3rd 3rd R 4th 5th 6th 1971 1984 1988 1990 1993 2000 2007 6 History of the AMA Guides 1956 - ad hoc committee 1958-1970 - 13 publications in JAMA 1971 - First Edition 1981 - established 12 expert panels 1984 - Second Edition 1988 - Third Edition 1990 - Third Edition-Revised 1993 - Fourth Edition (4 printings) 2000 – Fifth Edition (November 2000) 2007 (December) – Sixth Edition Radical paradigm shift 7 AMA Guides Growth in Size 700 600 500 400 Pages 300 200 100 0 Third Second Third Fourth Fifth Sixth Rev. Pages 245 254 262 339 613 634 8 Goals Explain the concept of impairment Discuss the proper use of the AMA Guides Explain source and limitations of the Guides Describe the steps involved in evaluating impairment Discuss critical issues encountered in the use of the Guides 11 Purpose of the Guides Provide a reference framework Achieve objective fair and reproducible evaluations Minimize adversarial situations Process for collecting, recording, and communicating information 12 The AMA Guides must adopt the terminology and conceptual framework of disablement as put forward by the International Classification of Functioning, Disability and Health (ICF). -

Classification of Finger Posture in Drop Finger Due to Cervical Foraminal Stenosis: a Mini-Review
hysical M f P ed l o ic a in n r e u & o R J l e a h International Journal of Physical n a b o i t i l i a ISSN: 2329-9096t a n r t i e o t n n I Medicine & Rehabilitation Mini Review Classification of Finger Posture in Drop Finger Due to Cervical Foraminal Stenosis: A Mini-Review Mitsuru Furukawa1*, Michihiro Kamata2 1Department of Orthopedic Surgery, Murayama Medical Center, Tokyo, Japan; 2Department of Orthopedic Surgery, Keiyu Hospital, Kanagawa, Japan ABSTRACT Few reports have been published examining cervical foraminal stenosis as the cause of drop finger. This mini-review, therefore, will provide a summary of the findings of articles published on this topic, written in both English and Japanese. Cervical foraminal stenosis is difficult to diagnose from imaging findings alone; thus, physical examination findings are often needed to make a firm diagnosis. Numbness of the fingers, the extent of interscapular pain, and finger posture can be used to differentiate drop finger due to cervical foraminal stenosis from other diseases. It is crucial to provide sufficient explanation to the patient before a decompression surgery is performed because the recovery of muscle strength is often incomplete and the improvement may be small. Keywords: Drop finger; Cervical foraminal stenosis; C7 nerve root; C8 nerve root ABBREVIATIONS: RESULTS CFS: cervical foraminal stenosis; PION; Posterior Interosseous The search obtained three case reports, one clinical feature, and Nerve; ECR; Extensor Carpi Radialis; EDM; Extensor Digiti one surgical outcome from PubMed, whereas two case reports Minimi; EIP; Extensor Indicis Proprius and two reviews came from the Japan Medical Abstracts Society. -

By: Laura M. Kunz, M.A.,Ccc-Slp
BY: LAURA M. KUNZ, M.A.,CCC-SLP What is a Touch-Cue System? A Touch-Cue system is a series of hand signals that are associated with consonant sounds; these hand signals are Speech Skills placed in different locations around the mouth to prompt sound production. Learning to speak is a process that develops gradually from The Touch-Cue System, presented in this book, has been adapted and modified infancy to 7 or 8 years of age. There are differences in the age at from several different sources to fit the needs of our preschool program. which children master particular speech sounds. It is important to This book was originally developed to help stimulate accurate production of error remember that learning to produce a speech sound correctly in all sounds in children with severe articulation delays, such as apraxia (motor planning words and phrases is a gradual process. It is common for children problems) and phonological processes (delayed patterns of speech). After utilizing not to produce all speech sounds correctly until age 7 or 8. the program in the classroom it became evident that it worked for more than just BY AGE: CHILDREN HAVE MASTERED THESE SOUNDS the severe children. Every child with articulation delays began to benefit from this multi-sensory approach. The book is set up to help teach parents how to use tactile, 3 ½ p, m, h, n, w, b, and vowels visual and auditory cues to stimulate accurate production of sounds. Hand signals 4 ½ k, g, d, t, ng, y are used as visual cues. -

Wrist Problem Or Neck Problem? 8:00Am - 7:00Pm Wednesday - Carpal Tunnel Syndrome Is One of the and Arm Pain Or Tingling
ACTIVE P.T. SOLUTION S ...BECAUSE LIFE SHOULD BE ACTIVE APTS Monthly Office Hours: VOLUME VI, ISSUE IX SEPTEMBER 2016 Monday - 8:00am - 5:30pm Tuesday - Wrist Problem or Neck Problem? 8:00am - 7:00pm Wednesday - Carpal tunnel syndrome is one of the and arm pain or tingling. There are When the shoulders round and the most common nerve entrapments of some that get temporary relief but the head shifts forward, the muscles in 8:00am - 5:30pm the upper extremity. It occurs when problem recurs frequently with symp- the neck and shoulders compress Thursday - the median nerve is compressed in toms of higher intensity. Other pa- the nerves that course from the the wrist. However, it is not uncom- tients develop symptoms similar to neck to the hand. The hand re- 8:00am - 5:30pm mon for compression of the median carpal tunnel syndrome following neck quires a stable base at the neck and nerve to occur in several different injury. They may not have had a wrist shoulders in order to function Friday - sites in the forearm. Over the course injury but still experience pain in the properly. Weakness caused by 8:00am - 4:00pm of time, the general population has hand. inactivity and poor posture ulti- come to accept that hand and wrist mately causes the hand and fore- Location: pain, numbness, or tingling adds up to Since the body is a complex network arm muscles to be overworked. carpal tunnel syndrome. In fact, hun- of joints, nerves, ligaments, muscle, This results in “double crush syn- 91 Columbus Street dreds of people each year have wrist and fascia, it is possible that a symp- drome” or nerve compression in Auburn, NY 13021 decompression surgery in hopes of tom from one area of the body may be the neck and shoulders proximally relieving these symptoms. -

Ischaemic Sensory Loss in Patients with Peripheral Nerve Lesions by R
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.17.2.104 on 1 May 1954. Downloaded from J. Neurol. Neurosurg. Psychiat., 1954, 17, 104. ISCHAEMIC SENSORY LOSS IN PATIENTS WITH PERIPHERAL NERVE LESIONS BY R. W. GILLIATT and T. GRAHAME WILSON From the National Hospital, Queen Square, London, and the Middlesex Hospital, London During an investigation of patients with painful appears in the form of a change in the quality of paraesthesiae due to median nerve compression at sensation in the finger-tips. When the skin is rubbed the wrist it was found that arresting the circulation it may feel numb and yet rough or prickly, and this to the affected arm by a pneumatic cuff sometimes change precedes tactile anaesthesia when fine hairs resulted in intense median paraesthesiae, with pain are used for testing (Lewis, Pickering, and Roth- resembling that of the patients' spontaneous attacks. schild, 1931; Sinclair, 1948). The time of onset of It was also found in these patients that the inflation these changes and the order in which the finger-tips of a pneumatic tourniquet round the arm might become involved is obviously of great importance result in the rapid onset of numbness where none in relation to the findings in peripheral nerve lesions, had been present before, and that it would make a and for this reason a fresh series of observations on Protected by copyright. mild sensory deficit more clear cut. This abnormally control subjects has been included in the present rapid failure of sensation in an area of initial sensory work. -

Upper Limb Electrical Stimulation Exercises. P Taylor, G Mann, C Johnson, L Malone
Salisbury FES Newsletter Jan 2002 Upper limb electrical stimulation exercises. P Taylor, G Mann, C Johnson, L Malone In this article we wish to document some of the electrical stimulation techniques we use for the upper limb, primarily with hemiplegics, in the Salisbury FES clinic. There is a growing body evidence for the effectiveness of the use of electrical stimulation in the upper limb but it is not the intention that it is reviewed here. Instead, we refer you to the excellent recent review articles by John Chae et. al1, 2 and the comprehensive review in the Rancho Book.3 The Rancho Book also includes a very useful description of electrical stimulation techniques and treatment regimes. Electrical stimulation can be used for the following purposes: For strengthening weak muscle As with any repetitive exercise, muscle bulk and strength will be increased. This will also lead to greater capillary density and therefore improved local blood supply and tissue condition. For increasing ROM Electrical stimulation can provide regular stretching, similar to passive stretching but performed over a more extended period. Be careful that some joints are not over stretched while trying to increase the range of others. For example it is sometimes useful to use MCP joint extension blocking splint to protect the MCP joints and improve the effectiveness of the action on the PIP and DIP joints. Another example might be the use of wrist flexion blocking splints when exercising finger flexors. Care must be taken that repetitive movement does not lead to skin marking. For enhancing the effect of botulinum toxin. -
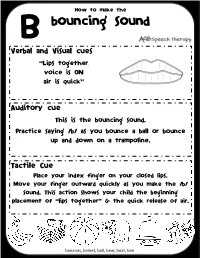
Bouncing Sound
How to make the B bouncing sound Verbal and Visual cues “Lips together, voice is ON air is quick” Auditory cue This is the bouncing sound. Practice saying /b/ as you bounce a ball or bounce up and down on a trampoline. Tactile Cue Place your index finger on your closed lips. Move your finger outward quickly as you make the /b/ sound. This action shows your child the beginning placement of “lips together” & the quick release of air. bananas, basket, ball, bear, boat, bee How to make the CH choo-choo sound Verbal and Visual cues “Lips are apart but close, and may be rounded tongue is behind front teeth, voice is OFF, air is quick” Auditory cue This is the choo-choo sound. Practice saying CH as you push a train on the tracks. Tactile Cue Place your hands on either side of your mouth and expand your fingers as you make the CH sound. This action shows your child the beginning placement of lips close and the & the quick release of air. chair, chart, cheese, chilly, peach, beach How to make the d drumming sound Verbal and Visual cues “Lips apart, tongue is up, front Voice is ON sound is quick” Auditory cue This is the drumming sound. Practice saying /d/ as you pound out a rhythm on a drum. Tactile Cue Place your index finger in the center of your lips, just under your nose. Move your finger outward quickly as you make the /d/ sound. This action shows your child the tongue placement & the quick release of sound. -

An Approach to the Painful Upper Limb
An approach to the painful upper limb Pain in the upper limb is a common presenting complaint in the primary health care setting and the origins of such pain are wide and varied. E Mogere, MB ChB, MMed (Gen Surgery) Division of Neurosurgery, University of Cape Town and Groote Schuur Hospital, Cape Town T Morgado, MB ChB, MRCS (Eng) Division of Neurosurgery, University of Cape Town and Groote Schuur Hospital, Cape Town D Welsh, FRCS (Eng), FCS (SA) Neurosurgery Division of Neurosurgery, University of Cape Town and Groote Schuur Hospital, Cape Town Correspondence to: E Mogere ([email protected]) The pain generator in the upper limb should to the shoulder, arm or hand, suggesting upper limb may require examination of the broadly be considered as: a local musculo-tendinous/skeletal cause.[1] eyes (to exclude Horner’s syndrome), an • spinal (radiculopathy or myeloradiculopa- Alternatively, the pain may radiate from assessment of neck movement, a vascular thy) the neck down into the limb, or from the assessment, breast and axilla palpation • peripheral nerve hand up towards the upper arm, suggesting and a neurological assessment of the lower • musculo-tendinous neurological origin. limbs. This is in addition to a thorough • skeletal (appendicular). neurological and orthopaedic assessment of The pattern of radiation may follow a the limb itself. The clinical approach dermatomal (radiculopathy) or non- The clinical findings are key to pinpointing dermatomal pattern (peripheral nerve or Neurological examination includes the pain source. non-neurological source). Pain radiation assessment of muscle power and bulk, does not preclude a non-neurological tendon reflexes and sensation. -

Occupational Therapy
OCCUPATIONAL THERAPY FOR CHILDREN WITH DOWN SYNDROME Janice Flegle MA OTR/L BCP Assistant Professor Munroe-Meyer Institute Occupational Therapy Department OBJECTIVES: Discuss the functional impact of low muscle tone, finger joint hyper-mobility, and (potential) visual involvement on the prehensile refinement and general dexterity of individual’s with Down Syndrome. Describe the relationship between communicative intent, literacy level, and handwriting readiness. Explore the rationale for oral motor compensations commonly seen when individual’s w/ Down Syndrome are eating and drinking. Explore the developmental requirements of self- care tasks that are difficult to master. “WHAT?! MY HANDS ARE FINE!” Hyper-mobile joints: move beyond typical ROM with little effort Inherent instability Thumb MCP and CMC joints most vulnerable Short fingers Low muscle tone Visual involvement FINE MOTOR SKILL ACQUISITION Early learning depends a lot on object manipulation Developmental ‘readiness’ apparent via the child’s interest, curiosity, self-initiated attempts ‘Ready’ for tool use when combining two objects in play FINE MOTOR SKILL ACQUISITION Needs more guidance, verbal cuing, encouragement, and modeling to learn new skills. Retention of learned skills will depend on whether or not that skill is important in the child’s routine. FINE (?) PINCER GRASP Often use middle finger Pad to Pad vs. and thumb to pick up Tip to Tip pincer small objects (vs. index Finger splay; palmer & thumb). surface lacks contour HANDWRITING . Scribbling: early tool-use . Representational Drawing . begin to understand that their drawings can represent something or someone… . Shapes / Symbols . these can be labeled and combined to add meaning . Communicative intent . handwriting is a form of communication ORAL MOTOR CHALLENGES .