HPTN 071 Statistical Analysis Plan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Kenya - Caucus Parliamentary Parliamentary National Assembly of Kenya National Assembly Hon
AFRICA 2019-2020 THE ICCF GROUP INTERNATIONALCONSERVATION.ORG COPYRIGHT INTERNATIONAL CONSERVATION CAUCUS FOUNDATION MISSION THE MOST ADVANCED TO ADVANCE SOLUTION IN CONSERVATION CONSERVATION GOVERNANCE BY WE BUILD POLITICAL WILL BUILDING The ICCF Group advances governments' leadership in conservation internationally by building political will POLITICAL WILL, within legislatures and supporting governments in the management of protected areas. PROVIDING ON-THE-GROUND CATALYZING CHANGE WITH KNOWLEDGE & EXPERTISE SOLUTIONS The ICCF Group supports political will by catalyzing strategic partnerships and knowledge sharing between policymakers and our extensive network. VISION TO PRESERVE THE WORLD'S MOST CRITICAL LANDSCAPES A WORLD The ICCF Group's international track record in legislative outcomes, public-private partnerships, & land WHERE management demonstrates that our unique model is emerging as a cost-effective, sustainable solution to PEOPLE AND conservation governance challenges. NATURE SUSTAIN AND NURTURE ONE ANOTHER 2019-2020 THE ICCF GROUP THE ICCF GROUP IN AFRICA EMPOWERING POLICYMAKERS &AND THE JUDICIARY The ICCF Group is working in East, Southern, and Central Africa to foster political will for conservation and support the sustainable management of natural resources. The ICCF Group has facilitated the establishment of parliamentary conservation caucuses in ten countries and is collaborating with each of these coalitions of policymakers to strengthen governance across several key natural resource sectors. The ICCF Group coordinates high-level political engagement with expertise on conservation strategies and solutions; facilitates interactions between U.S. and international policymakers, conservation organizations, and government agencies; and seeks to leverage and integrate resources in support of sustainable natural resource management policies. ICCF-supported caucuses enable, inform, and strengthen policymakers in their commitment to conservation. -

Analysis of the Market Structures and Systems for Indigenous Fruit Trees: the Case for Uapaca Kirkiana in Zambia
ANALYSIS OF THE MARKET STRUCTURES AND SYSTEMS FOR INDIGENOUS FRUIT TREES: THE CASE FOR UAPACA KIRKIANA IN ZAMBIA by Kaala Bweembelo Moombe Thesis submitted in partial fulfilment of the requirements for the degree of Master of Forest Science at the University of Stellenbosch Department of Forest and Wood Science Faculty of AgriSciences Supervisor: Mr Cori Ham Co-supervisors: Ms. Jeannette Clark, Dr Steve Franzel and Mr. Pierre Ackerman March 2009 Declaration By submitting this thesis electronically I, Kaala Bweembelo Moombe, declare that the entirety of the work contained in this thesis is my own, original work, that I am the owner of the copyright thereof (unless to the extent explicitly otherwise stated) and that I have not previously in its entirety or in part submitted it for obtaining any qualification. Date: 19th Feburuary 2009 Signature: _ ____ Copyright© 2009 Stellenbosch University All rights reserved ii ABSTRACT This study is about marketing of Uapaca kirkiana fruit in Zambia, a fruit that has great economic value especially among the rural and urban poor. It contributes to general food security. In southern Africa, farmers and other stakeholders have identified Uapaca as a priority species for domestication. Current agroforestry initiatives are promoting integration of indigenous trees into farming systems to provide marketable products for income generation. Domestication of trees however, depends on expanding the market demand for tree products. There is considerable evidence that expanding market opportunities is critical for the success of domestication innovations but farmers have been introduced to domestication with little consideration for marketing. The existing market potential can be achieved through sound knowledge on markets and marketing. -

Registered Voters by Gender and Constituency
REGISTERED VOTERS BY GENDER AND CONSTITUENCY % OF % OF SUB % OF PROVINCIAL CONSTITUENCY NAME MALES MALES FEMALES FEMALES TOTAL TOTAL KATUBA 25,040 46.6% 28,746 53.4% 53,786 8.1% KEEMBE 23,580 48.1% 25,453 51.9% 49,033 7.4% CHISAMBA 19,289 47.5% 21,343 52.5% 40,632 6.1% CHITAMBO 11,720 44.1% 14,879 55.9% 26,599 4.0% ITEZH-ITEZHI 18,713 47.2% 20,928 52.8% 39,641 5.9% BWACHA 24,749 48.1% 26,707 51.9% 51,456 7.7% KABWE CENTRAL 31,504 47.4% 34,993 52.6% 66,497 10.0% KAPIRI MPOSHI 41,947 46.7% 47,905 53.3% 89,852 13.5% MKUSHI SOUTH 10,797 47.3% 12,017 52.7% 22,814 3.4% MKUSHI NORTH 26,983 49.5% 27,504 50.5% 54,487 8.2% MUMBWA 23,494 47.9% 25,545 52.1% 49,039 7.4% NANGOMA 12,487 47.4% 13,864 52.6% 26,351 4.0% LUFUBU 5,491 48.1% 5,920 51.9% 11,411 1.7% MUCHINGA 10,072 49.7% 10,200 50.3% 20,272 3.0% SERENJE 14,415 48.5% 15,313 51.5% 29,728 4.5% MWEMBEZHI 16,756 47.9% 18,246 52.1% 35,002 5.3% 317,037 47.6% 349,563 52.4% 666,600 100.0% % OF % OF SUB % OF PROVINCIAL CONSTITUENCY NAME MALES MALES FEMALES FEMALES TOTAL TOTAL CHILILABOMBWE 28,058 51.1% 26,835 48.9% 54,893 5.4% CHINGOLA 34,695 49.7% 35,098 50.3% 69,793 6.8% NCHANGA 23,622 50.0% 23,654 50.0% 47,276 4.6% KALULUSHI 32,683 50.1% 32,614 49.9% 65,297 6.4% CHIMWEMWE 29,370 48.7% 30,953 51.3% 60,323 5.9% KAMFINSA 24,282 51.1% 23,214 48.9% 47,496 4.6% KWACHA 31,637 49.3% 32,508 50.7% 64,145 6.3% NKANA 27,595 51.9% 25,562 48.1% 53,157 5.2% WUSAKILE 23,206 50.5% 22,787 49.5% 45,993 4.5% LUANSHYA 26,658 49.5% 27,225 50.5% 53,883 5.3% ROAN 15,921 50.1% 15,880 49.9% 31,801 3.1% LUFWANYAMA 18,023 50.2% -

Members of the Northern Rhodesia Legislative Council and National Assembly of Zambia, 1924-2021
NATIONAL ASSEMBLY OF ZAMBIA Parliament Buildings P.O Box 31299 Lusaka www.parliament.gov.zm MEMBERS OF THE NORTHERN RHODESIA LEGISLATIVE COUNCIL AND NATIONAL ASSEMBLY OF ZAMBIA, 1924-2021 FIRST EDITION, 2021 TABLE OF CONTENTS FOREWORD ................................................................................................................................................ 3 PREFACE ..................................................................................................................................................... 4 ACKNOWLEDGEMENTS .......................................................................................................................... 5 ABBREVIATIONS ...................................................................................................................................... 7 INTRODUCTION ........................................................................................................................................ 9 PART A: MEMBERS OF THE LEGISLATIVE COUNCIL, 1924 - 1964 ............................................... 10 PRIME MINISTERS OF THE FEDERATION OF RHODESIA .......................................................... 12 GOVERNORS OF NORTHERN RHODESIA AND PRESIDING OFFICERS OF THE LEGISTRATIVE COUNCIL (LEGICO) ............................................................................................... 13 SPEAKERS OF THE LEGISTRATIVE COUNCIL (LEGICO) - 1948 TO 1964 ................................. 16 DEPUTY SPEAKERS OF THE LEGICO 1948 TO 1964 .................................................................... -

Report of the Auditor General on Deployment of Teachers in Basic
Republic of Zambia Report of the Auditor General on Deployment of Teachers in Basic Schools July 2014 Deployment of Teachers in Basic Schools 1 2 Deployment of Teachers in Basic Schools Foreword This report is on the deployment of teachers in basic schools and the audit was conducted pursuant to the Public Finance Act No. 15 of 2004, which empowers me to carry out performance and other specialised audits in government ministries and departments and report my findings to Parliament. In the course of audit, and in conformity with the Office reporting procedure, the draft report was communicated to the Permanent Secretary who was requested to respond to the issues raised therein within thirty (30) days of the issuance of the draft report. However, and in spite of the reminder sent to the Ministry in October 2012, as at the reporting date, the Ministry had not provided comments on the contents of the draft report. I nevertheless, wish to thank the Permanent Secretary and staff at the Ministry of Education Headquarters as well as provinces and districts, for their cooperation during the audit and preparation of this report. I also wish to extend my appreciation to other staff, including teachers, in all the schools visited for according me time and information I required for the audit. Dr. Anna O. Chifungula Auditor General Deployment of Teachers in Basic Schools iii Acronyms CPD Continuous Professional Development DEBS District Education Board Secretary DEBs District Education Boards DESO District Education Standards Officer FNDP Fifth National -

Republic of Zambia Living Conditions Monitoring
REPUBLIC OF ZAMBIA LIVING CONDITIONS MONITORING SURVEY III 2002 ENUMERATORS INSTRUCTION MANUAL CENTRAL STATISTICAL OFFICE P.O. BOX 31908 LUSAKA, ZAMBIA. PHONE: 251377/251385/252575/251381/250195/253609/253578/253908 TEL/FAX: 252575/253578/253908/253468 1 Enumerator’s Instructions Manual – LCMS III THE LIVING CONDITIONS MONITORING SURVEY III (2002) ENUMERATOR'S INSTRUCTION MANUAL TABLE OF CONTENTS CHAPTER PAGE CHAPTER I - INTRODUCTION ...................................................................................... 4 CHAPTER II - LISTING PROCEDURE ........................................................................... 9 2.1 Introduction ........................................................................................................... 9 2.2 Identification.......................................................................................................... 9 2.3 Summary of the SEA........................................................................................... 10 2.4 Sampling particulars............................................................................................. 10 2.5 Listing ................................................................................................................... 10 CHAPTER III - ENUMERATION................................................................................... 19 SECTION 1:HOUSEHOLD ROSTER............................................................................. 24 SECTION 2: MARITAL STATUS AND ORPHANHOOD........................................... -

NATIONAL ASSEMBLY ZAMBIA PARLIAMENTARY CONSERVATION CAUCUS (Updated January 11, 2019)
NATIONAL ASSEMBLY ZAMBIA PARLIAMENTARY CONSERVATION CAUCUS (Updated January 11, 2019) Co-Chairs Hon. Ephraim Belemu (UPND – Mbabala) Hon. Anthony Kasandwe (PF – Bangweulu) Members 1. Hon. Stephen Kampyongo (PF- Shiwang’andu MP) 2. Hon. Nickson Chilangwa (PF – Kawambwa) 3. Hon. Mutinta Mazoka (UPND – Pemba) 4. Hon. Steve Chungu (PF – Luanshya) 5. Hon. Malozo Sichone (PF – Isoka) 6. Hon. Jean Kapata (PF – Mandevu) 7. Hon. Dora Siliya (PF – Petauke) 8. Hon. Princess Kasune (UPND – Keembe) 9. Hon. Pilila Jere (Indp – Lumezi) 10. Hon. Margaret Miti (PF – Vubwi) 11. Hon. Emerine Kabashi (PF – Luapula) 12. Hon. Maria Langa( PF Chilanga) 13. Hon. Mumbi J. C. Phiri (PF – Nominated) 14. Hon. Credo Nanjuwa (UPND – Mumbwa) 15. Hon. Njamba Machila (Indp – Mwembeshi) 16. Hon. Peter Daka (MMD – Musanzala) 17. Hon. Maxas Ng’onga (PF – Kaputa) 18. Hon. Martin Malama (PF – Kanchibiya) 19. Hon. Kapembwa Simbao (PF – Senga Hill) 20. Hon. Mwalimu Simfukwe (PF – Mbala PF) 21. Hon. Garry Nkombo (UPND – Mazabuka) 22. Hon. Cornelius Mweetwa (UPND – Choma) 23. Hon. Mbolowa Subulwa (Indp – Siaoma) 24. Hon. Chinga Miyutu (UPND – Kalabo Central) 25. Hon. Mwansa Mbulakulima (PF – Milengi) 26. Hon. Richard Musukwa (PF – Chililabombwe) 27. Hon. Gift Chiyalika (PF – Lufubu) 28. Hon. Mubika Mubika (UPND – Shangombo) 29. Hon. Brian Mundubile (PF – Mporokoso) 30. Hon. Makebi Zulu (PF – Malambo) 31. Hon. Mwimba H Malama (PF Mfuwe) 32. Hon. Davison Mung’andu(PF – Chama South) 33. Hon. Teddy J Kasongo (PF – Nominated) 34. Hon. Gift Sialubalo (PF – Nominated) 35. Hon. Emmanuel Mulenga (PF – Ndola Central) 36. Hon. Whiteson Banda (PF – Nakonde) 37. Hon. Chishi C. Kasanda (UPND – Chisamba) 38. -

Dissemination Meetings for the Rural Finance
Republic of Zambia Ministry of Finance Investments and Debt Management Department Rural Finance Unit Report on the Rural Finance Policy and Strategy Dissemination Workshop 9th-11th December, 2019 Radisson Blu Hotel, Lusaka TABLE OF CONTENTS 1.0 INTRODUCTION .......................................................................................................... 1 2.0 OBJECTIVE ................................................................................................................... 2 3.0 DISCUSSIONS ............................................................................................................... 2 3.1 Financial Sector Policy Landscape in Zambia ............................................................ 2 3.2 Brief Overview of the Rural Finance Policy and Strategy .......................................... 3 3.2.1 The Role of the Legislature in Rural Finance ...................................................... 4 3.2.2 The Role of Government Line Ministries in Rural Finance ................................ 4 3.2.3 The Role of the Private Sector and Strategic Partners in Rural Finance ............. 4 3.3 The Rural Finance Expansion Programme.................................................................. 5 4.0 SUMMARY AND RECOMMENDATIONS................................................................. 5 APPENDICES ........................................................................................................................... 6 i. Table of Questions Asked .............................................................................................. -

District Investment Profile
DISTRICT INVESTMENT PROFILE LOCATION Ndola lies between latitudes 120° and 160° south and between 250° and 30° east of the Equator. It has borders with three (3) districts namely; Masaiti, Luanshya and Kitwe and shares an international boundary with the Democratic Republic of Congo (DRC) to the north. The City of Ndola has total land coverage of 1,108 km². Ndola falls within the gently sloping Copperbelt peneplain at an altitude ranging from 1250 to 1455 above sea level. The District is characterized by undulating terrain of less than 10 slopes and is dissected by the Mwambashi, Muliashi, Kafubu and Luansobe Rivers, the principle drainage lines to the Kafue River. Though there are isolated highly outcrops at Dola, Nakaputa and Kaloko hills, the average elevation is 1200 m above sea level NDOLA DISTRICT RESOURCE MAP CLIMATE AND RAINFALL PATTERN Ndola enjoys a typical savannah climate with three distinct seasons, namely the warm rainy season (November to April), the cool dry season (May to August) and the hot season (September to October). The district as a whole receives an average annual rainfall of 400mm. The rainfall distribution is mainly determined by the topography and prevailing 1 | P a g e winds from the Congo. The mean annual temperature is between 20°c and 25ºc with the absolute minimum temperatures of 32 degrees in January and the absolute minimum temperature of 12 degrees in June and July. The mean humidity rate is at 81% with the highest in January averaging 96% in the early morning and 66% in the early afternoons. The predominant direction of the prevailing winds is from 00 to 29 east of north at an average speed of 4.5 km per hour. -
Resource Allocation Model for The
RESOURCE ALLOCATION MODEL FOR THE CONSTITUENCY DEVELOPMENT FUND Frank Kakungu Working Paper No. 13 December 2013 © Zambia Institute for Policy Analysis & Research 2013 i Abstract Detailed information on the location of those with the greatest need for publicly provided social services may be the most valuable information policy makers could use to allocate resources, plan and budget. More often than not, the emphasis has been on evaluating the distribution of poverty, as defined by income insufficiency, to inform resource allocation. Theoretically, measures of household wealth can be reflected by income, consumption or expenditure information. However, the collection of accurate income and consumption data requires extensive resources for household surveys. As regards, it may be more appropriate to focus on relative material and social deprivation than narrowly defined poverty. More importantly when one wants to evaluate the distribution of relative disadvantaged status between quite small geographic areas (e.g. Constituency), it is best to use data derived from the census, given that it is the most inclusive and representative of all household surveys. More overall, income from surveys are measures more reflective of short-run household’s wealth or living standard, inadequate for estimating long-run poverty accurately whereas other socio-economic and demographic census variables are regarded as much more reliable to estimate long-run deprivation. The research reported on in this paper has calculated a composite index of deprivation using -
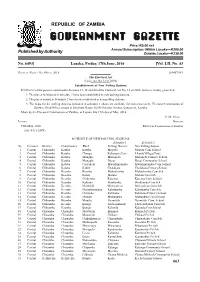
C:\Users\Public\Documents\GP JOBS\Gazette\Special Gazette No
REPUBLIC OF ZAMBIA Price: K5.00 net Annual Subscription: Within Lusaka—K200.00 Published by Authority Outside Lusaka—K230.00 No. 6493] Lusaka, Friday, 17th June, 2016 [Vol. LII, No. 43 GAZETTE NOTICE NO.416OF 2016 [6940718/1 The Electoral Act (Laws, Act No.12 of 2006) Establishment of New Polling Stations INEXERCISEof the powers contained in Sections 37, 38 and 40 of the Electoral Act No. 12 of 2006, notice is hereby given that: 1. The places mentioned in schedule 1 have been established as new polling districts. 2. The places named in Schedule 2 have been established as new polling stations. 3. The maps for the polling districts indicated in schedule 1 above are available for inspection at the Electoral Commission of Zambia, Head Office, situate at Elections House, Haille Selassie Avenue, Longacres, Lusaka. Made by the Electoral Commission of Zambia, at Lusaka this 19th day of May, 2016. P. M. ISAAC, LUSAKA Director 19th May, 2016 Electoral Commission of Zambia (101/5/5/ CONF) SCHEDULE OF NEW POLLING STATIONS Schedule 1 Schedule 2 No. Province District Constituency Ward Polling District New Polling Station 1 Central Chibombo Katuba Katuba Mayota Mayota Com School 2 Central Chibombo Katuba Chungu Kabangwe East Lilanda Village(Tent) 3 Central Chibombo Katuba Mungule Musopelo Musopelo Primary School 4 Central Chibombo Katuba Mungule Duzai Duzai Community School 5 Central Chibombo Katuba Cholokelo Mwashinyambo Mwashinyambo Com School 6 Central Chibombo Katuba Kabile Chalabana Chalabana Primary School 7 Central Chibombo Keembe Keembe Mukachembe -

Social Networks and the Political Salience of Ethnicity
Quarterly Journal of Political Science, 2019, 14:1–39 Social Networks and the Political Salience of Ethnicity Nicholas Eubank1∗ 1Center for the Study of Democratic Institutions, Vanderbilt University, Nashville, TN, USA; [email protected] ABSTRACT Ethnic politics scholars are increasingly convinced that (a) the political salience of ethnicity and (b) the correlation between ethno- linguistic fractionalization (ELF) and poor development are driven by the dense social networks shared by co-ethnics. By this ar- gument, social networks allow ethnic parties to leverage inbuilt networks to share information and support collective action, while ethnically fragmented communities struggle to hold politicians ac- countable. This paper provides the first comprehensive empirical test of the assumption underlying this argument. Using seven months of telecommunications data from 9 million mobile sub- scribers in Zambia — which includes records of almost 2 billion calls and SMS messages — to measure social networks across an entire country, this paper finds that electoral constituencies with high ELF also have more fragmented social networks, especially in rural areas. It also finds other potential cleavages that have not achieved political salience (namely, religious identity and em- ployment sector) are not correlated with network fragmentation, consistent with the idea that ethnicity achieves salience because it offers an organizational advantage not offered by other cleavages. Finally, it also finds that both voter knowledge and public goods are negatively correlated with network fragmentation, consistent with the network-proxy hypothesis. ∗This project would not have been possible without the generosity of numerous parties, including Real Impact Analytics, Real Impact’s Chief Data Scientists Gautier Krings, and its CEO Sébastien Deletaille.