Bacterial Metabolites of Human Gut Microbiota Correlating with Depression
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Electronic Supplementary Material (ESI) for Analyst. This Journal Is © the Royal Society of Chemistry 2017
Electronic Supplementary Material (ESI) for Analyst. This journal is © The Royal Society of Chemistry 2017 Supplemental Table 2. Proteins Increased in Either Blood or Horizon media Table 2A. Proteins Increased in Spores Produced on Horizon Soil Over Spores Produced on Blood Medium quasi.fdr Protein Protein Class/Name KEGG Pathway Names or Function (if ID Pathways found in KEGG) Amino Acid Metabolism bat00250, bat00280, Alanine, aspartate and glutamate metabolism, bat00410, Valine, leucine and isoleucine degradation, bat00640, beta-Alanine metabolism to acetyl CoA, 4.50E-07 BAS0310 4-aminobutyrate aminotransferase bat00650 Propanoate metabolism, Butanoate metabolism bat00270, bat00330, Cysteine and methionine metabolism, Arginine bat00410, and proline metabolism, beta-Alanine 3.84E-10 BAS5060 spermidine synthase bat00480 metabolism, Glutathione metabolism bat00270, bat00330, Cysteine and methionine metabolism, Arginine bat00410, and proline metabolism, beta-Alanine 2.30E-09 BAS5219 spermidine synthase bat00480 metabolism, Glutathione metabolism bat00250, Alanine, aspartate and glutamate metabolism, 6.94E-07 BAS0561 alanine dehydrogenase bat00430 Taurine and hypotaurine metabolism bat00250, Alanine, aspartate and glutamate metabolism, 5.23E-07 BAS4521 alanine dehydrogenase bat00430 Taurine and hypotaurine metabolism 0.005627 BAS5218 agmatinase, putative bat00330 Arginine and proline metabolism 2,3,4,5-tetrahydropyridine-2- carboxylate N-succinyltransferase, 1.40E-10 BAS3891 putative bat00300 Lysine biosynthesis bat00010, bat00020, Glycolysis -
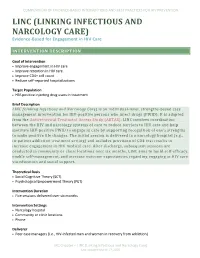
LINKING INFECTIOUS and NARCOLOGY CARE) Evidence-Based for Engagement in HIV Care
COMPENDIUM OF EVIDENCE-BASED INTERVENTIONS AND BEST PRACTICES FOR HIV PREVENTION LINC (LINKING INFECTIOUS AND NARCOLOGY CARE) Evidence-Based for Engagement in HIV Care INTERVENTION DESCRIPTION Goal of Intervention • Improve engagement in HIV care • Improve retention in HIV care • Improve CD4+ cell count • Reduce self-reported hospitalizations Target Population • HIV-positive injecting drug users in treatment Brief Description LINC (Linking Infectious and Narcology Care) is an individual-level, strengths-based case management intervention for HIV-positive persons who inject drugs (PWID). It is adapted from the Antiretroviral Treatment Access Study (ARTAS). LINC involves coordination between the HIV and narcology systems of care to reduce barriers to HIV care and help motivate HIV-positive PWID to engage in care by supporting recognition of one’s strengths to make positive life changes. The initial session is delivered in a narcology hospital (e.g., in-patient addiction treatment setting) and includes provision of CD4 test results to increase engagement in HIV medical care. After discharge, subsequent sessions are conducted in community or clinic locations over six months. LINC aims to build self-efficacy, enable self-management, and increase outcome expectancies regarding engaging in HIV care via education and social support. Theoretical Basis • Social Cognitive Theory (SCT) • Psychological Empowerment Theory (PET) Intervention Duration • Five sessions delivered over six months Intervention Settings • Narcology hospital • Community or clinic locations • Phone Deliverer • Peer case managers (i.e., HIV-infected men and women in recovery from addiction) LRC Chapter – LINC (Linking Infectious and Narcology Care) Last updated March 17, 2020 COMPENDIUM OF EVIDENCE-BASED INTERVENTIONS AND BEST PRACTICES FOR HIV PREVENTION Delivery Methods • Case management • Printed materials • Discussion • Video • Goal setting Structural Components There are no reported structural components reported for this study. -

Chapter 5 High-Pressure Stopped-Flow Kinetic Studies of Nnos
Probing the dynamics and conformational landscape of neuronal nitric oxide synthase A thesis submitted to the University of Manchester for the degree of Doctor of Philosophy in the Faculty of Life Sciences 2013 Anna Sobolewska-Stawiarz Contents Contents ...................................................................................................................... 2 List of Figures ............................................................................................................. 6 List of Tables ............................................................................................................ 10 Abstract ..................................................................................................................... 12 Declaration ................................................................................................................ 13 Copyright Statement ................................................................................................ 13 Acknowledgements ................................................................................................... 14 List of Abbreviations ............................................................................................... 15 List of Amino Acids Abbreviations ........................................................................ 17 CHAPTER 1. INTRODUCTION ........................................................................... 18 1.1 Nitric oxide synthase ......................................................................................... -

Protein S-Nitrosylation: Methods of Detection and Cellular Regulation
Protein S-Nitrosylation: Methods of Detection and Cellular Regulation by Michael Tcheupdjian Forrester Department of Biochemistry Duke University Date:_______________________ Approved: ___________________________ Jonathan S. Stamler, MD (Supervisor) ___________________________ Irwin Fridovich, PhD ___________________________ K. V. Rajagopalan, PhD ___________________________ Dennis J. Thiele, PhD ___________________________ Eric J. Toone, PhD Dissertation submitted in partial fulfillment of the requirements for the degree of doctor of philosophy in the Department of Biochemistry in the Graduate School of Duke University 2009 i v ABSTRACT Protein S-Nitrosylation: Methods of Detection and Cellular Regulation by Michael Tcheupdjian Forrester Department of Biochemistry Duke University Date:_______________________ Approved: ___________________________ Jonathan S. Stamler, MD (Supervisor) ___________________________ Irwin Fridovich, PhD ___________________________ K. V. Rajagopalan, PhD ___________________________ Dennis J. Thiele, PhD ___________________________ Eric J. Toone, PhD An abstract of a dissertation submitted in partial fulfillment of the requirements for the degree of doctor of philosophy in the Department of Biochemistry in the Graduate School of Duke University 2009 i v Copyright by Michael T. Forrester 2009 Abstract Protein S-nitrosylation—the post-translational modification of cysteine thiols into S-nitrosothiols—is a principle mechanism of nitric oxide-based signaling. Studies have demonstrated myriad roles for S-nitrosylation in organisms from bacteria to humans, and recent efforts have begun to elucidate how this redox-based modification is regulated during physiological and pathophysiological conditions. This doctoral thesis is focused on the 1) analysis of existing methodologies for the detection of protein S-nitrosylation; 2) development of new methodologies for the detection of protein S-nitrosylation and 3) discovery of novel enzymatic mechanisms by which S-nitrosylation is regulated in vivo. -

Control Engineering Perspective on Genome-Scale Metabolic Modeling
Control Engineering Perspective on Genome-Scale Metabolic Modeling by Andrew Louis Damiani A dissertation submitted to the Graduate Faculty of Auburn University in partial fulfillment of the requirements for the Degree of Doctor of Philosophy Auburn, Alabama December 12, 2015 Key words: Scheffersomyces stipitis, Flux Balance Analysis, Genome-scale metabolic models, System Identification Framework, Model Validation, Phenotype Phase Plane Analysis Copyright 2015 by Andrew Damiani Approved by Jin Wang, Chair, Associate Professor of Chemical Engineering Q. Peter He, Associate Professor of Chemical Engineering, Tuskegee University Thomas W. Jeffries, Professor of Bacteriology, Emeritus; University of Wisconsin-Madison Allan E. David, Assistant Professor of Chemical Engineering Yoon Y. Lee, Professor of Chemical Engineering Abstract Fossil fuels impart major problems on the global economy and have detrimental effects to the environment, which has caused a world-wide initiative of producing renewable fuels. Lignocellulosic bioethanol for renewable energy has recently gained attention, because it can overcome the limitations that first generation biofuels impose. Nonetheless, in order to have this process commercialized, the biological conversion of pentose sugars, mainly xylose, needs to be improved. Scheffersomyces stipitis has a physiology that makes it a valuable candidate for lignocellulosic bioethanol production, and lately has provided genes for designing recombinant Saccharomyces cerevisiae. In this study, a system biology approach was taken to understand the relationship of the genotype to phenotype, whereby genome-scale metabolic models (GSMMs) are used in conjunction with constraint-based modeling. The major restriction of GSMMs is having an accurate methodology for validation and evaluation. This is due to the size and complexity of the models. -

Boletin De Documentación Nº 37, Marzo De 2009
Su elaboración en formato electrónico, iniciada en julio de 2002, ha supuesto importantes ventajas de cara a ampliar y agilizar su difusión entre los profesionales del sector, permitiendo asimismo la localización de documentación relevante por parte de cualquier ciudadano interesado en el campo de las drogodependencias. Como en los números anteriores, en el boletín de marzo se recogen las principales novedades bibliográficas que, sobre los distintos aspectos relacionados con las adicciones, han tenido entrada en el Centro de Documentación e Información de la Delegación del Gobierno para el Plan Nacional sobre Drogas en los tres últimos meses. El contenido del Boletín está estructurado en tres grandes epígrafes: Novedades bibliográficas (clasificadas por su temática y con indicación de su ruta en el caso de que estén disponibles a texto completo en Internet), Legislación y Sumarios de revistas. Esperamos que el Boletín, cuya difusión se realiza a través de listas de distribución de correo electrónico y de su presencia permanente en la página web de la Delegación del Gobierno para el Plan Nacional sobre Drogas, sea de interés y quedamos a la espera de cualquier sugerencia y/o consulta que sobre el mismo queráis formular. Ministerio de Sanidad y Consumo. Delegación del Gobierno para el Plan Nacional sobre Drogas José del Val – E-correo: [email protected] Jefe de Servicio del Centro de Documentación e Información 1 Aspectos Generales ........................................................................ 4 Aspectos Sociales ............................................................................ -
KEGG Orthology-Based Annotation of the Predicted
Dunlap et al. BMC Genomics 2013, 14:509 http://www.biomedcentral.com/1471-2164/14/509 DATABASE Open Access KEGG orthology-based annotation of the predicted proteome of Acropora digitifera: ZoophyteBase - an open access and searchable database of a coral genome Walter C Dunlap1,2, Antonio Starcevic4, Damir Baranasic4, Janko Diminic4, Jurica Zucko4, Ranko Gacesa4, Madeleine JH van Oppen1, Daslav Hranueli4, John Cullum5 and Paul F Long2,3* Abstract Background: Contemporary coral reef research has firmly established that a genomic approach is urgently needed to better understand the effects of anthropogenic environmental stress and global climate change on coral holobiont interactions. Here we present KEGG orthology-based annotation of the complete genome sequence of the scleractinian coral Acropora digitifera and provide the first comprehensive view of the genome of a reef-building coral by applying advanced bioinformatics. Description: Sequences from the KEGG database of protein function were used to construct hidden Markov models. These models were used to search the predicted proteome of A. digitifera to establish complete genomic annotation. The annotated dataset is published in ZoophyteBase, an open access format with different options for searching the data. A particularly useful feature is the ability to use a Google-like search engine that links query words to protein attributes. We present features of the annotation that underpin the molecular structure of key processes of coral physiology that include (1) regulatory proteins of -

Biochemical and Cellular Studies of Vertebrate Globins
Biochemical and Cellular Studies of Vertebrate Globins By Shun Wilford Tse Thesis submitted for the degree of Doctor of Philosophy School of Biological Sciences University of East Anglia September 2015 © This copy of the thesis has been supplied on condition that anyone who consults it is understood to recognise that its copyright rests with the author and that no quotations from the thesis, nor any information derived there-from may be published without the author's prior, written consent. Abstract Human cytoglobin is a small heme-containing protein in the globin superfamily with a wide range of tissue and organ distribution. Although several cellular functions have been proposed for cytoglobin, the exact physiological function is still not fully defined. Recently, cytoglobin has been implicated to have a regulatory role in cancer cells to control cell proliferation and migration depending on cellular oxygen level. In order to gain a better understanding of a structure-to-function relationship of cytoglobin as a heme-protein and to evaluate its possible physiological function(s) in cancer cells, a combination of techniques, including protein engineering and advanced spectroscopies, was deployed. In this study, recombinant human cytoglobin purified from E.coli was purified as a monomeric protein, but displayed a dimeric property in solution. An intra-molecular disulphide bond is formed within the protein which has a redox potential at ca -280 mV. Advanced spectroscopic studies confirmed a low-spin bis-histidyl heme in cytoglobin in both ferric and ferrous state regardless of the state of the disulphide bond. Furthermore, nitrite reductase activitiy in globins was investigated in detail using myoglobin as a model to explore the biochemical basis of the distal histidine residue in determining activity. -

Nitric Oxide Dioxygenase: an Enzymic Function for Flavohemoglobin
Proc. Natl. Acad. Sci. USA Vol. 95, pp. 10378–10383, September 1998 Biochemistry Nitric oxide dioxygenase: An enzymic function for flavohemoglobin PAUL R. GARDNER*, ANNE M. GARDNER,LORI A. MARTIN, AND ANDREW L. SALZMAN Division of Critical Care Medicine, Children’s Hospital Medical Center, and Department of Pediatrics, University of Cincinnati, 3333 Burnet Avenue, Cincinnati, OH 45229 Communicated by Irwin Fridovich, Duke University Medical Center, Durham, NC, July 7, 1998 (received for review June 9, 1998) ABSTRACT Nitric oxide (NO•) is a toxin, and various life Moreover, this aerobic cyanide-sensitive NO• consumption forms appear to have evolved strategies for its detoxification. activity appeared to constitute part of an adaptive defense NO•-resistant mutants of Escherichia coli were isolated that against NO• toxicity. Thus, we supposed that E. coli mutants rapidly consumed NO•.AnNO•-converting activity was re- containing elevated activity might be selected for resistance to • constituted in extracts that required NADPH, FAD, and O2, 2 NO -mediated killing, and furthermore, that they could be was cyanide-sensitive, and produced NO3 . This nitric oxide used to facilitate the biochemical and genetic characterization dioxygenase (NOD) contained 19 of 20 N-terminal amino of the NO• scavenging activity. acids identical to those of the E. coli flavohemoglobin. Fur- Here, we describe the isolation and characterization of an thermore, NOD activity was produced by the flavohemoglobin O2-dependent and cyanide-sensitive nitric oxide dioxygenase gene and was inducible by NO•. FlavohemoglobinyNOD- (NOD) from NO•-resistant E. coli, which is a flavohemoglo- deficient mutants were also sensitive to growth inhibition by bin. The identification of NOD with flavohemoglobin is sig- gaseous NO•. -

Use of the Communication Checklist
Psychiatria Danubina, 2020; Vol. 32, Suppl. 1, pp 88-92 Conference paper © Medicinska naklada - Zagreb, Croatia USE OF THE COMMUNICATION CHECKLIST - SELF REPORT (CC-SR) IN SCHIZOPHRENIA: LANGUAGE IMPAIRMENTS CORRELATE WITH POOR PREMORBID SOCIAL ADJUSTMENT Daria Smirnova1,2, Svetlana Zhukova3, Olga Izmailova4, Ilya Fedotov5, Yurii Osadshiy6, Alexander Shustov7, Anna Spikina8, Dmitriy Ubeikon9, Anna Yashikhina2, Natalia Petrova10, Johanna Badcock1, Vera Morgan1 & Assen Jablensky1 1Centre for Clinical Research in Neuropsychiatry, University of Western Australia, Perth, Australia 2Department of Psychiatry, Narcology, Psychotherapy and Clinical Psychology, Samara State Medical University, Samara, Russia 3Department of Psychiatry, Narcology and Psychology, Ivanovo State Medical Academy, Ivanovo, Russia 4Samara District Clinical Psychiatric Hospital, Samara, Russia 5Department of Psychiatry, Ryazan State Medical University n.a. academician I.P. Pavlov, Ryazan, Russia 6Department of Psychiatry, Narcology and Medical Psychology, Rostov State Medical University, Rostov-on-Don, Russia 7National Medical Research Centre of Psychiatry and Narcology n.a. V.P. Serbsky, Moscow, Russia 8Psychoneurological dispensary ʋ2, Saint Petersburg, Russia 9Department of Psychiatry, Narcology and Psychotherapy with the course of General and Medical psychology, S.I. Georgievsky Medical Academy, V.I. Vernadsky Crimean Federal University, Simferopol, Republic of Crimea, Russia 10Department of Psychiatry and Narcology, Saint Petersburg State University, Saint Petersburg, -

Workbook Psychiatry and Narcology
Kharkiv National Medical University Department of Psychiatry, Narcology and Medical Psychology WORKBOOK MANUAL FOR INDIVIDUAL WORK FOR MEDICAL STUDENTS PSYCHIATRY AND NARCOLOGY (Part 2) Student ___________________________________________________________ Faculty _________________________________________________________ Course _________________ Group _____________________________________ Kharkiv 2019 Затверджено вченою радою ХНМУ Протокол №5 від 23.05.2019 р. Psychiatry (Part 2) : workbook manual for individual work of students / I. Strelnikova, G. Samardacova, К. Zelenska – Kharkiv, 2019. – 103 p. Копіювання для розповсюдження в будь-якому вигляді частин або повністю можливо тільки з дозволу авторів навчального посібника. CLASS 7. NEUROTIC DISORDERS. CLINICAL FORMS. TREATMENT AND REHABILITATION. POSTTRAUMATIC STRESS DISORDER. TREATMENT AND REHABILITATION. Psychogenic diseases are a large and clinically varied group of diseases resulting from an effect of acute or long-term psychic traumas, which manifest themselves by both mental and somatoneurological disorders and, as a rule, are reversible. Psychogenic diseases are caused by a psychic trauma, i.e. some events which affect significant aspects of existence of the human being and result in deep psychological feelings. These may be subjectively significant events, i.e. those which are pathogenic for the majority of people. Besides, the psyche may be traumatized by conventionally pathogenic events, which cause feelings in an individual because of his peculiar hierarchy of values. Unfavorable psychogenic effects on the human being cause stress in him, i.e. a nonspecific reaction at the physiological, psychological and behavioural levels. Stress may exert some positive, mobilizing influence, but may result in disorganization of the organism activity. The stress, which exerts a negative influence and causes various disturbances and even diseases, is termed distress. Classification of neurotic disorders I. -

Current Advances of Nitric Oxide in Cancer and Anticancer Therapeutics
Review Current Advances of Nitric Oxide in Cancer and Anticancer Therapeutics Joel Mintz 1,†, Anastasia Vedenko 2,†, Omar Rosete 3 , Khushi Shah 4, Gabriella Goldstein 5 , Joshua M. Hare 2,6,7 , Ranjith Ramasamy 3,6,* and Himanshu Arora 2,3,6,* 1 Dr. Kiran C. Patel College of Allopathic Medicine, Nova Southeastern University, Davie, FL 33328, USA; [email protected] 2 John P Hussman Institute for Human Genomics, Miller School of Medicine, University of Miami, Miami, FL 33136, USA; [email protected] (A.V.); [email protected] (J.M.H.) 3 Department of Urology, Miller School of Medicine, University of Miami, Miami, FL 33136, USA; [email protected] 4 College of Arts and Sciences, University of Miami, Miami, FL 33146, USA; [email protected] 5 College of Health Professions and Sciences, University of Central Florida, Orlando, FL 32816, USA; [email protected] 6 The Interdisciplinary Stem Cell Institute, Miller School of Medicine, University of Miami, Miami, FL 33136, USA 7 Department of Medicine, Cardiology Division, Miller School of Medicine, University of Miami, Miami, FL 33136, USA * Correspondence: [email protected] (R.R.); [email protected] (H.A.) † These authors contributed equally to this work. Abstract: Nitric oxide (NO) is a short-lived, ubiquitous signaling molecule that affects numerous critical functions in the body. There are markedly conflicting findings in the literature regarding the bimodal effects of NO in carcinogenesis and tumor progression, which has important consequences for treatment. Several preclinical and clinical studies have suggested that both pro- and antitumori- Citation: Mintz, J.; Vedenko, A.; genic effects of NO depend on multiple aspects, including, but not limited to, tissue of generation, the Rosete, O.; Shah, K.; Goldstein, G.; level of production, the oxidative/reductive (redox) environment in which this radical is generated, Hare, J.M; Ramasamy, R.; Arora, H.