Summary of Product Characteristics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

PACKAGE LEAFLET: INFORMATION for the USER Lercanidipine
PACKAGE LEAFLET: INFORMATION FOR THE USER Lercanidipine Hydrochloride 10 mg Film-coated Tablets Lercanidipine Hydrochloride 20 mg Film-coated Tablets lercanidipine hydrochloride Read all of this leaflet carefully before you start using this medicine because it contains important information for you. - Keep this leaflet. You may need to read it again. - If you have any further questions, ask your doctor or pharmacist. - This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours. - If you get any of the side effects talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4. What is in this leaflet: 1. What Lercanidipine Hydrochloride Film-coated Tablets is and what it is used for 2. What you need to know before you take Lercanidipine Hydrochloride Film-coated Tablets 3. How to take Lercanidipine Hydrochloride Film-coated Tablets 4. Possible side effects 5. How to store Lercanidipine Hydrochloride Film-coated Tablets 6. Contents of the pack and other information 1. WHAT LERCANIDIPINE HYDROCHLORIDE FILM-COATED TABLETS IS AND WHAT IT IS USED FOR Lercanidipine belongs to a group of medicines called calcium channel blockers (dihydropyridine derivatives) that lower blood pressure.. Lercanidipine is used to treat high blood pressure also known as hypertension in adults over the age of 18 years (it is not recommended for children under 18 years old). 2. WHAT YOU NEED TO KNOW BEFORE YOU TAKE LERCANIDIPINE -

Summary of Product Characteristics, Labelling and Package Leaflet
SUMMARY OF PRODUCT CHARACTERISTICS, LABELLING AND PACKAGE LEAFLET 1 SUMMARY OF PRODUCT CHARACTERISTICS 2 1. NAME OF THE MEDICINAL PRODUCT /.../ 10 mg film-coated tablet /.../ 20 mg film-coated tablet 2. QUALITATIVE AND QUANTITATIVE COMPOSITION One film-coated tablet contains 10 mg lercanidipine hydrochloride, equivalent to 9.4 mg lercanidipine. One film-coated tablet contains 20 mg lercanidipine hydrochloride, equivalent to 18.8 mg lercanidipine. Excipient with known effect: /.../ 10 mg film-coated tablet: Lactose monohydrate 30 mg Excipient with known effect: /.../ 20 mg film-coated tablet: Lactose monohydrate 60 mg For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Film--coated tablet /.../ 10 mg film-coated tablet: Yellow, round, biconvex 6.5 mm film-coated tablets, scored on one side, marked 'L' on the other side. /.../ 20 mg film-coated tablet: Pink, round, biconvex 8.5 mm film-coated tablets, scored on one side, marked 'L' on the other side. The score line is only to facilitate breaking for ease of swallowing and not to divide into equal doses. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications /.../ is indicated for the treatment of mild to moderate essential hypertension. 4.2 Posology and method of administration Posology Route of administration: For oral use. The recommended dosage is 10 mg orally once a day at least 15 minutes before meals; the dose may be increased to 20 mg depending on the individual patient's response. Dose titration should be gradual, because it may take about 2 weeks before the maximal antihypertensive effect is apparent. Some individuals, not adequately controlled on a single antihypertensive agent, may benefit from the addition of lercandipine to therapy with a beta-adrenoreceptor blocking drug, a diuretic (hydrochlorothiazide) or an angiotensin converting enzyme inhibitor. -

Dorset Medicines Advisory Group
DORSET CARDIOLOGY WORKING GROUP GUIDELINE FOR CALCIUM CHANNEL BLOCKERS IN HYPERTENSION SUMMARY The pan-Dorset cardiology working group continues to recommend the use of amlodipine (a third generation dihydropyridine calcium-channel blocker) as first choice calcium channel blocker on the pan-Dorset formulary for hypertension. Lercanidipine is second choice, lacidipine third choice and felodipine is fourth choice. This is due to preferable side effect profiles in terms of ankle oedema and relative costs of the preparations. Note: where angina is the primary indication or is a co-morbidity prescribers must check against the specific product characteristics (SPC) for an individual drug to confirm this is a licensed indication. N.B. Lacidipine and lercandipine are only licensed for use in hypertension. Chapter 02.06.02 CCBs section of the Formulary has undergone an evidence-based review. A comprehensive literature search was carried out on NHS Evidence, Medline, EMBASE, Cochrane Database, and UK Duets. This was for recent reviews or meta-analyses on calcium channel blockers from 2009 onwards (comparative efficacy and side effects) and randomised controlled trials (RCTs). REVIEW BACKGROUND Very little good quality evidence exists. No reviews, meta-analyses or RCTs were found covering all calcium channel blockers currently on the formulary. Another limitation was difficulty obtaining full text original papers for some of the references therefore having to use those from more obscure journals instead. Some discrepancies exist between classification of generations of dihydropyridine CCBs, depending upon the year of publication of the reference/authors’ interpretation. Dihydropyridine (DHP) CCBs tend to be more potent vasodilators than non-dihydropyridine (non-DHP) CCBs (diltiazem, verapamil), but the latter have greater inotropic effects. -

Lercanidipine Vs Lacidipine in Isolated Systolic Hypertension
Journal of Human Hypertension (2003) 17, 799–806 & 2003 Nature Publishing Group All rights reserved 0950-9240/03 $25.00 www.nature.com/jhh ORIGINAL ARTICLE Lercanidipine vs lacidipine in isolated systolic hypertension M Millar-Craig1, B Shaffu2, A Greenough3, L Mitchell3 and C McDonald3 1Department of Cardiology, Derbyshire Royal Infirmary, London Road, Derby, UK; 2Station Road Surgery, 152 Station Road, Wigston, Leicester, UK; 3Napp Pharmaceuticals Limited, Cambridge Science Park, Milton Road, Cambridge, UK This randomised, double-blind, double-dummy, parallel blood pressure was À0.81 (À4.45, 2.84) mmHg. These group, multicentre study compared the efficacy and confidence intervals were within the limits specified for tolerability of lercanidipine with lacidipine. Elderly equivalence, that is, (À5, 5) mmHg. Ambulatory blood patients with isolated systolic hypertension (supine pressure monitoring showed that the antihypertensive blood pressure X160/o95 mmHg) were enrolled and effects of both drugs lasted for the full 24-h dosing underwent a placebo run-in period of 14–27 days before period and followed a circadian pattern. Both treatments random allocation to lercanidipine tablets 10 mg once were well tolerated with a low incidence of adverse drug daily (n ¼ 111) or lacidipine tablets 2 mg once daily reactions and a low withdrawal rate. Significantly fewer (n ¼ 111) for the assessment period (112–160 days). patients withdrew from treatment with lercanidipine Titration to lercanidipine 20 mg once daily (two 10 mg (P ¼ 0.015). Neither treatment had any clinically signifi- tablets) or lacidipine 4 mg once daily (two 2 mg tablets) cant effect on pulse rate or cardiac conduction. -

Preparation and Evaluation of Self-Micro Emulsifying Drug Delivery Systems of Lercanidipine Hcl Using Medium and Short Chain Glycerides: a Comparative Study
Preparation and Evaluation of Self-micro Emulsifying Drug Delivery Systems of Lercanidipine HCl using Medium and Short Chain Glycerides: A Comparative Study Vrunda C. Suthar, Shital B. Butani Department of Pharmaceutics and Pharmaceutical Technology, Institute of Pharmacy, Nirma University, Ahmedabad, Gujarat, India Abstract Aims: The aim of this study was to formulate a self-microemulsifying drug delivery system (SMEDDS) ORIGINAL ARTICLE ORIGINAL of Lercanidipine HCl (LCH) using medium chain (MC) and short chain (SC) glycerides as oil phase and to compare the dissolution efficiency of both formulations. Materials and Methods: Different oils and surfactants containing MC and SC fatty acid as basic molecule were screened using quantitative solubility study and constructing pseudoternary phase diagrams. Cosolvents were used as cosurfactants. The preconcentrates were tested for a self-microemulsifying time, % transmittance, cloud point, globule size, zeta potential, and in-vitro drug release. Selected formulations were compared by calculating dissolution efficiencies in different pH media. Results: Capmul MCM, Cremophor® RH 40, and polyethylene glycol 400 were chosen as oil, surfactant, and cosurfactant, respectively, for MC glyceride and triacetin and Tween 80 were selected as oil and surfactant for SC triglyceride category, respectively. All the formulations spontaneously resulted into transparent microemulsion with globule sizes range from 50 to 90 nm for MC-SMEDDS and 200-317 nm for SC-SMEDDS. The formed microemulsions were stable as shown by zeta potential and cloud point determination. However, in-vitro drug release in 0.1 N HCl showed quite a similar dissolution of all the formulation batches, a study in the different pH media showed that LCH being weak base, possess pH dependent solubility. -

1. What Enalapril/Lercanidipine Krka Is and What It Is Used
PL. ENALAPRIL/LERCANIDIPINE KRKA 10 MG/10 MG IE first page IIIIIfflI Package leaflet: Information for the user 1. What Enalapril/Lercanidipine Krka is - obstruction to the flow of blood from the left ventricle • if you have renal problems (including kidney transplantation); - temsirolimus, sirolimus, everolimus and other medicines • potassium-sparing diuretics (e.g. triamterene, amiloride), • a medicine for ulcers and heartburn called cimetidine at of the heart, including a narrowing of the aorta (aortic • if you have abnormally increased levels of a hormone belonging to the class of mTOR inhibitors (used to avoid potassium supplements or medicines containing daily doses of more than 800 mg. and what it is used for stenosis); called aldosterone in your blood (primary aldosteronism); rejection of transplanted organs and for cancer), potassium (including dietary salt substitutes), other drugs • medicines which are most often used to treat diarrhoea Enalapril/Lercanidipine Krka Enalapril/Lercanidipine Krka is a fixed combination of an - chest discomfort occurring at rest or becoming worse • if you have liver problem; - racecadotril (used to treat diarrhoea), which can increase potassium in your body (such as (racecadotril) or avoid rejection of transplanted organs 10 mg/10 mg film-coated tablets ACE-inhibitor (enalapril) and a calcium channel blocker or happening more often (unstable angina pectoris); • if you have a blood problem, such as low or lack of white - vildagliptin (a medicine used to treat diabetes). heparin, a medicine used to thin blood to prevent clots; (sirolimus, everolimus, temsirolimus and other medicines (lercanidipine), two medicines that lower blood pressure. - within one month after suffering a heart attack blood cells (leucopenia, agranulocytosis), low platelet If you are about to have a procedure trimethoprim and co-trimoxazole also known as belonging to the class of mTOR inhibitors). -
Calcium Channel Blockers (Ccbs)
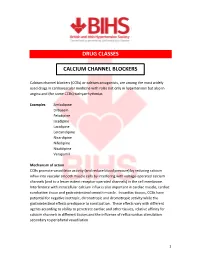
DRUG CLASSES CALCIUM CHANNEL BLOCKERS Calcium channel blockers (CCBs) or calcium antagonists, are among the most widely used drugs in cardiovascular medicine with roles not only in hypertension but also in angina and (for some CCBs) tachyarrhythmias. Examples Amlodipine Diltiazem Felodipine Isradipine Lacidipine Lercanidipine Nicardipine Nifedipine Nisoldipine Verapamil Mechanism of action CCBs promote vasodilator activity (and reduce blood pressure) by reducing calcium influx into vascular smooth muscle cells by interfering with voltage-operated calcium channels (and to a lesser extent receptor-operated channels) in the cell membrane. Interference with intracellular calcium influx is also important in cardiac muscle, cardiac conduction tissue and gastrointestinal smooth muscle. In cardiac tissues, CCBs have potential for negative inotropic, chronotropic and dromotropic activity while the gastrointestinal effects predispose to constipation. These effects vary with different agents according to ability to penetrate cardiac and other tissues, relative affinity for calcium channels in different tissues and the influence of reflux cardiac stimulation secondary to peripheral vasodilation. 1 Although often considered as a single class, CCBs can be subdivided according to structural and functional distinctions. Dihydropyridine derivates : amlodipine, felodipine, isradipine, lacidipine, lercanidipine, nicardipine, nifedipine, nisoldipine Phenylalkylamine : verapamil Benzothiazepine derivative : diltiazem Dihydropyridine derivatives have pronounced -

New Medicine Service – List of Medicines
New Medicine Service – list of medicines May 2013 The medicines selected for inclusion in the NMS are those that are listed in the chapters/sub- sections, detailed below, of the current edition of the British National Formulary (www.bnf.org). Asthma and COPD BNF Ref BNF sub-section descriptor 3.1.1 Adrenoceptor agonists 3.1.2 Antimuscarinic bronchodilators 3.1.3 Theophylline 3.1.4 Compound bronchodilator preparations 3.2 Corticosteroids 3.3 Cromoglicate and related therapy, leukotriene receptor antagonists and phosphodiesterase type-4 inhibitors Type 2 Diabetes 6.1.1.1 Short acting insulins* 6.1.1.2 Intermediate and long acting insulins* 6.1.2 Antidiabetic drugs Antiplatelet/Anticoagulant therapy 2.8.2 Oral anticoagulants 2.9 Antiplatelet drugs Hypertension 2.2.1 Thiazides and related diuretics 2.4 Beta-adrenoceptor blocking drugs* 2.5.1 Vasodilator antihypertensive drugs 2.5.2 Centrally acting antihypertensive drugs 2.5.4 Alpha-adrenoceptor blocking drugs* 2.5.5 Drugs affecting the renin-angiotensin system* 2.6.2 Calcium-channel blockers* * where the community pharmacist can determine that the medicine has been newly prescribed for a patient with the specified condition. It is assumed that in most cases, the pharmacist will be able to determine the condition for which the new medicine is being prescribed from the PMR or by asking the patient. The following page contains a list of generic drug names which are listed in the above BNF sub- sections. This list is provided as an aid for pharmacists; for an up to date and definitive list of medicines that are included in the BNF sub-sections listed above the BNF should always be consulted. -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

A Guide to the Administration of Medicines in the Perioperative
......„„.....NHS Grampian Guideline For The Administration Of Medicines In The Pen-Operative Period Co-ordinators: Consultation Group: Approver: Pre-Operative Assessment See Consultation list Medicine Guidelines and Pharmacist Policies Group Signature: Signature: ...i 0 0 a Identifier: Review Date: Date Approved: NHSG/Guid/Peri0p/ May 2022 May 2019 MGPG1026 Uncontrolled when printed Version 3 Executive Sign-Off This document has been endorsed by the Director of Pharmacy and Medicines Management Signature: Title: Guideline for the Administration of Medicines in the Peri- Operative Period Unique Identifier: NHSG/Guid/PeriOp/MGPG1026 Replaces: NHSG/Guid/PeriOp/MGPG697, Version 2 Across NHS Organisation Directorate Clinical Service Sub Boards Wide Department Area This controlled document shall not be copied in part or whole without the express permission of the author or the author’s representative. Lead Author/Co-ordinator: Pre-Operative Assessment Pharmacist Subject (as per document Clinical Guidance registration categories): Key word(s): Peri-operative medication guidance, gastro intestinal system, cardiovascular system, respiratory, central nervous, infections, endocrine, obstetrics, gynaecology, urinary tract, malignant, nutrition, blood, musculoskeletal, joint, corticosteroid treatment, alternative routes, antiepileptic Process Document: Policy, Guideline Protocol, Procedure or Guideline Document application: NHS Grampian Purpose/description: This policy is designed to be used by pharmacy, nursing and medical staff at pre-assessment -

Lercanidipine, a New Third Generation Ca-Antagonist in the Treatment of Hypertension
Journal of Clinical and Basic Cardiology An Independent International Scientific Journal Journal of Clinical and Basic Cardiology 1999; 2 (2), 169-174 Lercanidipine, a new third generation Ca-antagonist in the treatment of hypertension Gasser R, Klein W, Köppel H Homepage: www.kup.at/jcbc Online Data Base Search for Authors and Keywords Indexed in Chemical Abstracts EMBASE/Excerpta Medica Krause & Pachernegg GmbH · VERLAG für MEDIZIN und WIRTSCHAFT · A-3003 Gablitz/Austria FOCUS ON CA-ANTAGONISTS Lercanidipine J Clin Basic Cardiol 1999; 2: 169 Lercanidipine, a new third generation Ca-antagonist in the treatment of hypertension R. Gasser, H. Köppel, W. Klein Recently several large endpoint studies have clearly established the importance of antihypertensive treatment in the preven- tion of cardiovascular death. Calcium antagonists clearly have their place within the therapeutic efforts aimed at cardiovascular risk control. Despite former debates on side effects and safety problems calcium channel blockers thus still hold an important position in the treatment of systemic hypertension. While earlier developments have focused on increasing potency and selec- tivity of calcium channel blockers, the most recent developments have brought about drugs with a particularly slow onset and long duration of action. The latest designer-drug in this context is lercanidipine. This particular calcium channel blocker combines practically all desired effects. Pharmacologically the drug has a high lipophilicity which enables a long duration and a single-dose use. It has a unique binding profile which guarantees constant calcium antagonistic action independent of serum concentration changes. The proportion of responding patients lies between 70 and 90 %. The ideal dosage is 10 to 20 mg per day. -

Pharmacological Drugs Inducing Ototoxicity, Vestibular Symptoms and Tinnitus: a Reasoned and Updated Guide
European Review for Medical and Pharmacological Sciences 2011; 15: 601-636 Pharmacological drugs inducing ototoxicity, vestibular symptoms and tinnitus: a reasoned and updated guide G. CIANFRONE1, D. PENTANGELO1, F. CIANFRONE2, F. MAZZEI1, R. TURCHETTA1, M.P. ORLANDO1, G. ALTISSIMI1 1Department of Otolaryngology, Audiology and Phoniatrics, “Umberto I” University Hospital, Sapienza University, Rome (Italy); 2Institute of Otorhinolaryngology, School of Medicine, Catholic University of the Sacred Heart, Rome (Italy) Abstract. – The present work on drug-in- Introduction duced ototoxicity, tinnitus and vertigo repre- sents the update and revision of a previous The panorama of the pharmacological origin guide to adverse drug reactions for italian physi- iatrogenic noxae able to induce either harmful cians (2005). The panorama of drug-induced side effects causing ototoxicity or symptoms ototoxic effects or just a symptomatology like tin- such as tinnitus or dizziness and vertigo has en- nitus or balance disturbances, without any harm- larged in recent years, thanks to a better knowl- ful consequence, has widened in the last few edge and a more specific attention of pharma- years. The reason for this is the progress of scien- ceutical firms and drug-control institutions. In tific knowledge, the increased awareness of the daily clinical practice, there is a need for the pharmaceutical companies and of the institutions, family physician and the ENT specialist or audi- ologist (also in consideration of the possible which supervise pharmaceutical production. medico-legal implications) to focus the attention Only through continuous updating and experi- on the possible risk of otological side effects. ence sharing it’s possible to offer patients the This would allow a clinical risk-benefit evalua- certainty of receiving the treatment that is appro- tion, weighing the possible clinical advantage in priate, safe and effective and based upon the their field of competence against possible oto- most credited clinical studies.