Zabdeno, INN-Ebola Vaccine
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ebola Hemorrhagic Fever: Properties of the Pathogen and Development of Vaccines and Chemotherapeutic Agents O
ISSN 00268933, Molecular Biology, 2015, Vol. 49, No. 4, pp. 480–493. © Pleiades Publishing, Inc., 2015. Original Russian Text © O.I. Kiselev, A.V. Vasin, M.P. Shevyryova, E.G. Deeva, K.V. Sivak, V.V. Egorov, V.B. Tsvetkov, A.Yu. Egorov, E.A. RomanovskayaRomanko, L.A. Stepanova, A.B. Komissarov, L.M. Tsybalova, G.M. Ignatjev, 2015, published in Molekulyarnaya Biologiya, 2015, Vol. 49, No. 4, pp. 541–554. REVIEWS UDC 578.2,578.76 Ebola Hemorrhagic Fever: Properties of the Pathogen and Development of Vaccines and Chemotherapeutic Agents O. I. Kiseleva, A. V. Vasina, b, M. P. Shevyryovac, E. G. Deevaa, K. V. Sivaka, V. V. Egorova, V. B. Tsvetkova, d, A. Yu. Egorova, E. A. RomanovskayaRomankoa, L. A. Stepanovaa, A. B. Komissarova, L. M. Tsybalovaa, and G. M. Ignatjeva a Institute of Influenza, Ministry of Health of the Russian Federation, St. Petersburg, 197376 Russia; email: [email protected] b St. Petersburg State Polytechnic University, St. Petersburg, 195251 Russia c Ministry of Health of the Russian Federation, Moscow, 127994 Russia d Topchiev Institute of Petrochemical Synthesis, Moscow, 119991 Russia Received December 29, 2014; in final form, January 16, 2015 Abstract—Ebola hemorrhagic fever (EHF) epidemic currently ongoing in West Africa is not the first among numerous epidemics in the continent. Yet it seems to be the worst EHF epidemic outbreak caused by Ebola virus Zaire since 1976 as regards its extremely large scale and rapid spread in the population. Experiments to study the agent have continued for more than 20 years. The EHF virus has a relatively simple genome with seven genes and additional reading frame resulting from RNA editing. -

Evidence Assessment STRATEGIC ADVISORY GROUP of EXPERTS (SAGE) on IMMUNIZATION Meeting 15 March 2021
Evidence Assessment STRATEGIC ADVISORY GROUP OF EXPERTS (SAGE) ON IMMUNIZATION Meeting 15 March 2021 FOR RECOMMENDATION BY SAGE Prepared by the SAGE Working Group on COVID-19 vaccines EVIDENCE ASSESSMENT: Ad26.COV2.S COVID-19 vaccine Key evidence to inform policy recommendations on the use of Ad26.COV2.S COVID-19 vaccine Evidence retrieval • Based on WHO and Cochrane living mapping and living systematic review of Covid-19 trials (www.covid-nma.com/vaccines) Retrieved evidence Majority of data considered for policy recommendations on Ad26.COV2.S Covid-19 vaccine are published in scientific peer reviewed journals: • Interim Results of a Phase 1–2a Trial of Ad26.COV2.S Covid-19 Vaccine. NEJM. February 2021. DOI: 10.1056/NEJMoa2034201. Jerald Sadoff, Mathieu Le Gars, Georgi Shukarev, et al. • FDA briefing document Janssen Ad26.COV2.S (COVID-19) Vaccine • Ad26 platform literature: Custers et al. Vaccines based on the Ad26 platform; Vaccine 2021 Quality assessment Type of bias Randomization Deviations from Missing outcome Measurement of Selection of the Overall risk of intervention data the outcome reported results bias Working Group Low Low Low Low Low LOW judgment 1 EVIDENCE ASSESSMENT The SAGE Working Group specifically considered the following issues: 1. Trial endpoints used in comparison with other vaccines Saad Omer 2. Evidence on vaccine efficacy in the total population and in different subgroups Cristiana Toscano 3. Evidence of vaccine efficacy against asymptomatic infections, reducing severity, hospitalisations, deaths, and efficacy against virus variants of concern Annelies Wilder-Smith 4. Vaccination after SARS-CoV2 infection. 5. Evidence on vaccine safety in the total population and in different subgroups Sonali Kochhar 6. -

To Ebola Reston
WHO/HSE/EPR/2009.2 WHO experts consultation on Ebola Reston pathogenicity in humans Geneva, Switzerland 1 April 2009 EPIDEMIC AND PANDEMIC ALERT AND RESPONSE WHO experts consultation on Ebola Reston pathogenicity in humans Geneva, Switzerland 1 April 2009 © World Health Organization 2009 All rights reserved. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distin- guished by initial capital letters. All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either express or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use. This publication contains the collective views of an international group of experts and does not necessarily represent the decisions or the policies of the World Health Organization. -

Understanding Ebola
Understanding Ebola With the arrival of Ebola in the United States, it's very easy to develop fears that the outbreak that has occurred in Africa will suddenly take shape in your state and local community. It's important to remember that unless you come in direct contact with someone who is infected with the disease, you and your family will remain safe. State and government agencies have been making preparations to address isolated cases of infection and stop the spread of the disease as soon as it has been positively identified. Every day, the Centers of Disease Control and Prevention (CDC) is monitoring developments, testing for suspected cases and safeguarding our lives with updates on events and the distribution of educational resources. Learning more about Ebola and understanding how it's contracted and spread will help you put aside irrational concerns and control any fears you might have about Ebola severely impacting your life. Use the resources below to help keep yourself calm and focused during this unfortunate time. Ebola Hemorrhagic Fever Ebola hemorrhagic fever (Ebola HF) is one of numerous Viral Hemorrhagic Fevers. It is a severe, often fatal disease in humans and nonhuman primates (such as monkeys, gorillas, and chimpanzees). Ebola HF is caused by infection with a virus of the family Filoviridae, genus Ebolavirus. When infection occurs, symptoms usually begin abruptly. The first Ebolavirus species was discovered in 1976 in what is now the Democratic Republic of the Congo near the Ebola River. Since then, outbreaks have appeared sporadically. There are five identified subspecies of Ebolavirus. -

Overview of Candidate Ebola Vaccines As of August 19, 2019
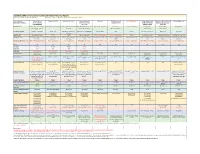
Ebola vaccines – Background paper for SAGE deliberations Overview of candidate Ebola vaccines as of August 19, 2019 Nine candidate Ebola vaccines have undergone or are currently undergoing clinical evaluation at different trial phases. Three vaccines were licensed, three vaccines have completed or are in trials up to Phase 1 phase, two vaccines up to or in Phase 2 stage, and one vaccine has completed Phase 3 stage. Type of Developer Strain(s) a. Current stage of clinical Proposed Proposed Proposed target Current storage Current formulation Number of clinical Forecasted production candidate aimed to evaluation vaccination indication population for the specifications* and presentation research grade does capacity vaccine protect schedule label indication available against b. Number of subjects with data (doses per vial) analysed to date c. Regulatory status PROPOSED INDICATION: REACTIVE USE DURING OUTBREAKS Licensed in country of origin Ad5-EBOV CanSino Biologics Zaire a. Phase 1 in China and Phase 2 in 1 dose Reactive 18 to 60 years +2°C to +8°C for 12 Final Formulation: 20,000 doses Can produce 150 000 (monovalent)1 Inc. & Beijing ebolavirus Sierra Leone months Lyophilized doses per year and Institute of (Makona) b. >681 people enrolled potentially scale-up to 500 Biotechnology, c. Licensed obtained from CFDA in 000 doses/year. China October 2017 to use under national Presentation: reserves by National Medical Single dose vial + Products Administration (NMPA), diluent China in the event of Ebola outbreak Submitted to WHO for Emergency Use Assessment and Listing (EUAL) in July 2018. Granted Breakthrough Therapy Designation by the US FDA and PRIME status by the European Medicines Agency (EMA) since 2016 rVSVΔG- Merck, USA Monovalent a. -

Improving the Regulatory Response to Vaccine Development During a Public Health Emergency
Every Minute Matters: Improving the Regulatory Response to Vaccine Development During a Public Health Emergency RASHMI BORAH* ABSTRACT In recent months, our lives have been turned upside down by the novel coronavirus (COVID-19) emergency. With no cure or vaccine in sight, millions of people have contracted the virus, and the death toll has surpassed that of World War I in a fraction of the time. In fact, the past decade has been marked by a series of highly publicized public health emergencies, including the devastating Ebola and Zika virus global outbreaks. Some of this panic arose from a failure to manufacture and distribute vaccines in a timely fashion. This failure occurred despite having several viable vaccine candidates, adequate funding, and strong public support for the vaccines. This Article explains how these failures are the consequence of a complex network of existing regulatory pathways and insufficient incentives to produce affordable vaccinations during a public health emergency. Fortunately, there are several ways that both the U.S. Patent and Trademark Office and the U.S. Food and Drug Administration can improve and streamline the process of patenting, approving, manufacturing, and distributing a vaccination. The last decade has demonstrated that public health emergencies occur quickly, and affected communities cannot afford the delays and mishaps that characterized the vaccine response to COVID-19, Ebola, and Zika. This Article explores three ways to facilitate the development and distribution of vaccinations during a public health emergency. First, the U.S. Patent and Trademark Office can establish a dedicated public health emergency patent pathway for vaccine technology developed specifically in response to a public health emergency. -
Candidate SARS-Cov-2 Vaccines in Advanced Clinical Trials: Key Aspects Compiled by John D
Candidate SARS-CoV-2 Vaccines in Advanced Clinical Trials: Key Aspects Compiled by John D. Grabenstein, RPh, PhD All dates are estimates. All Days are based on first vaccination at Day 0. Vaccine Sponsor Univ. of Oxford ModernaTX USA BioNTech with Pfizer Johnson & Johnson Novavax Sanofi Pasteur with CureVac with Bayer CanSino Biologics with Sinopharm (China National Sinovac Biotech Co. [with Major Partners] (Jenner Institute) (Janssen Vaccines & GlaxoSmithKline Academy of Military Biotec Group) (Beijing IBP, with AstraZeneca Prevention) Medical Sciences Wuhan IBP) Headquarters Oxford, England; Cambridge, Cambridge, Massachusetts Mainz, Germany; New York, New Brunswick, New Jersey Gaithersburg, Maryland Lyon, France; Tübingen, Germany Tianjin, China; Beijing, China; Beijing, China England, Gothenburg, New York (Leiden, Netherlands) Brentford, England Beijing, China Wuhan, China Sweden Product Designator ChAdOx1 or AZD1222 mRNA-1273 BNT162b2, tozinameran, Ad26.COV2.S, JNJ-78436735 NVX-CoV2373 TBA CVnCoV Ad5-nCoV, Convidecia BBIBP-CorV CoronaVac Comirnaty Vaccine Type Adenovirus 63 vector mRNA mRNA Adenovirus 26 vector Subunit (spike) protein Subunit (spike) protein mRNA Adenovirus 5 vector Inactivated whole virus Inactivated whole virus Product Features Chimpanzee adenovirus type Within lipid nanoparticle Within lipid nanoparticle Human adenovirus type 26 Adjuvanted with Matrix-M Adjuvanted with AS03 or Adjuvanted with AS03 Human adenovirus type 5 Adjuvanted with aluminum Adjuvanted with aluminum 63 vector dispersion dispersion vector AF03 -

What Clinicians Need to Know About Johnson & Johnson's Janssen COVID-19 Vaccine
Centers for Disease Control and Prevention Center for Preparedness and Response What Clinicians Need to Know About Johnson & Johnson’s Janssen COVID-19 Vaccine Clinician Outreach and Communication Activity (COCA) Webinar Tuesday, March 2, 2021 To Ask a Question ▪ All participants joining us today are in listen-only mode. ▪ Using the Webinar System – Click the “Q&A” button. – Type your question in the “Q&A” box. – Submit your question. ▪ The video recording of this COCA Call will be posted at https://emergency.cdc.gov/coca/calls/2021/callinfo_030221.asp and available to view on-demand a few hours after the call ends. ▪ If you are a patient, please refer your questions to your healthcare provider. ▪ For media questions, please contact CDC Media Relations at 404-639-3286, or send an email to [email protected]. Today’s Presenters ▪ Sarah Mbaeyi, MD, MPH CDR, U.S. Public Health Service Medical Officer National Center for Immunization and Respiratory Diseases Centers for Disease Control and Prevention ▪ Sara Oliver, MD LCDR, U.S. Public Health Service Co-lead, Advisory Committee for Immunization Practices COVID-19 Vaccines Work Group COVID-19 Response Centers for Disease Control and Prevention ▪ Kathleen Dooling, MD, MPH Medical Officer Co-lead, Advisory Committee for Immunization Practices COVID-19 Vaccines Work Group COVID-19 Response Centers for Disease Control and Prevention ACIP COVID-19 Vaccines What Clinicians Need to Know about Johnson and Johnson’s Janssen COVID-19 vaccine Sara Oliver MD, MSPH Sarah Mbaeyi MD, MPH Kathleen Dooling MD, MPH March 2, 2021 For more information: www.cdc.gov/COVID19 Outline: 1) Safety and efficacy of Janssen COVID-19 vaccines Dr. -

Ebola Virus Disease Outbreak in Equateur Province, Democratic Republic of Congo, First Update
RAPID RISK ASSESSMENT Ebola virus disease outbreak in Equateur Province, Democratic Republic of the Congo First update, 25 May 2018 Main conclusions and options for response This is the ninth Ebola virus disease (EVD) outbreak in the Democratic Republic of the Congo (DRC) since the discovery of the virus in 1976. From 4 April until 20 May 2018, 49 cases and 26 deaths have been recorded: of which 22 are confirmed, 21 are probable and six are suspected cases. Cases have been reported from the Bikoro health zone (n=29; 10 confirmed and 19 probable), the Iboko health zone (n=16; eight confirmed, two probable and six suspected) and the Wangata health zone (n=4; all confirmed) [1]. The current outbreak is taking place in health zones neighbouring the Congo River, which is an important pathway of trade and travel. In addition, four confirmed EVD cases have been reported in the health zone of Wangata within the port city of Mbandaka which has a population of 1.2 million people. These factors have raised concerns about an increased probability of the spread of the disease at the national level. The identification of EVD cases in the urban area of Mbandaka city and around Tumba Lake both connected to the Congo River increases the risk of regional spread to other provinces of DRC and neighbouring countries (namely Republic of the Congo and the Central African Republic). ECDC is closely monitoring this outbreak in liaison with the Ministry of Health in DRC, WHO and other partners, and will re- evaluate the risk for EU/EEA citizens if necessary according to epidemiological findings. -
COVID-19 Vaccine Communication Guide Presented By
COVID-19 Vaccine Communication Guide Presented by In collaboration with Table of Contents Purpose ......................................................................................................................................................... 3 What vaccines are available for COVID-19? ................................................................................................... 3 How do the vaccines work? ............................................................................................................................ 3 How many shots will I need? .......................................................................................................................... 4 How effective are the different vaccines? ....................................................................................................... 4 How do we know if the COVID-19 vaccines are safe? ..................................................................................... 4 What are side-effects of the vaccine? ............................................................................................................. 5 Vaccine Hesitancy .......................................................................................................................................... 5 COVID Vaccine Communication Strategies ..................................................................................................... 5 Reflection ................................................................................................................................................................ -

Risk Assessment and Risk Mitigation Review(S)
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 761169Orig1s000 RISK ASSESSMENT and RISK MITIGATION REVIEW(S) Division of Risk Management (DRM) Office of Medication Error Prevention and Risk Management (OMEPRM) Office of Surveillance and Epidemiology (OSE) Center for Drug Evaluation and Research (CDER) Application Type BLA Application Number 761169 PDUFA Goal Date October 25, 2020 OSE RCM # 2020-264 Reviewer Name(s) Elizabeth Everhart, MSN, RN, ACNP Team Leader Naomi Boston, PharmD Acting Deputy Division Doris Auth, PharmD Director Review Completion Date August 10, 2020; date entered into DARRTS, August 20, 2020 Subject Evaluation of Need for a REMS Established Name atoltivimab – odesivimab – maftivimab (REGN-EB3) Trade Name Inmazeb Name of Applicant Regeneron Pharmaceuticals, Inc. Therapeutic Class Human IgG monoclonal antibody Formulation Solution for infusion Dosing Regimen 50 mg of each mAb/kg (3mL/kg) IV (b) (4) × 1 1 Reference ID: 4659652 Table of Contents EXECUTIVE SUMMARY ............................................................................................................................................................3 1 Introduction........................................................................................................................................................................3 2 Background .........................................................................................................................................................................3 2.1 Product Information..............................................................................................................................................3 -

Ebola Virus Disease Outbreak in North Kivu and Ituri Provinces, Democratic Republic of the Congo – Second Update
RAPID RISK ASSESSMENT Ebola virus disease outbreak in North Kivu and Ituri Provinces, Democratic Republic of the Congo – second update 21 December 2018 Main conclusions As of 16 December 2018, the Ministry of Health of the Democratic Republic of Congo (DRC) has reported 539 Ebola virus disease (EVD) cases, including 48 probable and 491 confirmed cases. This epidemic in the provinces of North Kivu and Ituri is the largest outbreak of EVD recorded in DRC and the second largest worldwide. A total of 315 deaths occurred during the reporting period. As of 16 December 2018, 52 healthcare workers (50 confirmed and two probable) have been reported among the confirmed cases, and of these 17 have died. As of 10 December 2018, the overall case fatality rate was 58%. Since mid-October, an average of around 30 new cases has been reported every week, with 14 health zones reporting confirmed cases in the past 21 days. This trend shows that the outbreak is continuing across geographically dispersed areas. Although the transmission intensity has decreased in Beni, the outbreak is continuing in Butembo city, and new clusters are emerging in the surrounding health zones. A geographical extension of the outbreak (within the country and to neighbouring countries) cannot be excluded as it is unlikely that it will be controlled in the near future. Despite significant achievements, the implementation of response measures remains problematic because of the prolonged humanitarian crisis in North Kivu province, the unstable security situation arising from a complex armed conflict and the mistrust of affected communities in response activities.