2009 Organ Donation Congress 10Th ISODP & 16Th ETCO
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Appendix A—Digest of Other White House Announcements
Appendix A—Digest of Other White House Announcements The following list includes the President’s public President Vicente Fox of Mexico to discuss the schedule and other items of general interest an- situation in Argentina. nounced by the Office of the Press Secretary In the afternoon, the President traveled to and not included elsewhere in this book. Portland, OR, and later returned to the Bush Ranch in Crawford, TX. January 1 In the morning, at the Bush Ranch in January 7 Crawford, TX, the President had an intelligence In the morning, the President had an intel- briefing. ligence briefing. Later, he returned to Wash- The President issued an emergency declara- ington, DC. tion for areas struck by record and near-record The President announced the recess appoint- snowfall in New York. ment of John Magaw to be Under Secretary January 2 of Transportation for Security. In the morning, the President had an intel- The President announced his intention to ligence briefing. nominate Anthony Lowe to be Administrator of the Federal Insurance Administration at the January 3 Federal Emergency Management Agency. In the morning, the President had an intel- The President announced his intention to des- ligence briefing. ignate Under Secretary of Commerce for Inter- national Trade Grant D. Aldonas, Deputy Sec- January 4 retary of Labor Donald C. Findlay, and Under In the morning, the President had an intel- Secretary of the Treasury for International Af- ligence briefing. He then traveled to Austin, TX, and later returned to Crawford, TX. fairs John B. Taylor as members of the Board The President announced his intention to of the Overseas Private Investment Corporation. -

A Study to Determine the Color Preferences of School Children, 1950-1951
A study to determine the color preferences of school children, 1950-1951 Item Type text; Thesis-Reproduction (electronic) Authors Ryan, Leo Thomas, 1914- Publisher The University of Arizona. Rights Copyright © is held by the author. Digital access to this material is made possible by the University Libraries, University of Arizona. Further transmission, reproduction or presentation (such as public display or performance) of protected items is prohibited except with permission of the author. Download date 06/10/2021 16:01:14 Link to Item http://hdl.handle.net/10150/319109 A STUDY TO DETERMINE THE COLOR PREFERENCES OF SCHOOL CHILDREN 1950 - 1951 LeoL Ryanz /' v \ A Thesis submitted to the faculty of the Department of Education in partial fulfillment of the requirements for the degree of MASTER OF ARTS in the Graduate College, University of Arizona 1951 TABLE OP CONTENTS: Chapter Page ■I. INTRODUCTION«, t . 6 "II. BACKGROUND FOR THE STUDY. - . , . .18: III. METHOD OF PROCEDURE .............. 40 IVp PRESENTATION OF DATA. .............. 50 V. ANALYSIS AND INTERPRETATION .......... 64 VI. SUMMARY.-. ... V ' . .... ... ... 75 Oozig3.U1 s 2.ons o oo o a o o o o 0 a & 0 o o o 5 Recommendations® o 76 Xj im 11 a t x on s <> o ©& <» » « @ @ 6 « « © <> * © *7 7 Suggestions for Future Research • *, . <> • „ 77 BIBLIOGRAPHY o . < . , . o . , -* . , 78 AP P BIX 3D IDC ^ 0 8 o o o o o e o O © o o o © o o o o 8 ii LIST OF GH&RTS Ghart , . Page lo ■ SYMBOLISM OF COLORS Q . 0 21 II.:- SYMBOLISM OF DIRECTIONAL COLORS IN . ' DIFFERENT COUNTRIES . .. .. ... 23 III, SYMBOLISM OF COLORS OF THE ELEMENTS . -
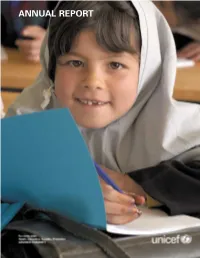
Annual Report 2002
ANNUAL REPORT KHUSHBOO GOES TO SCHOOL Khushboo, 7, whose name means ‘having a sweet scent’, is in second grade at the Ghulam Haider School in Kabul, Afghanistan. She likes being in school, and despite complaining “My teachers give me lots of homework to do…!” she says she wants to be a teacher some day. Khushboo lives in a poor neighbourhood with her family: her father, who is a messenger, her mother, a younger brother, and a 10-year-old sister who also goes to this school. UNICEF provided Khushboo’s school with learning materials and paid for teacher training. The school was one of thousands that benefited from UNICEF assistance after years of conflict and extreme poverty had nearly destroyed the country’s educa- tion system. The previous regime had banned all girls, including Khushboo’s sister, from attending school. From 2001 to 2002, UNICEF led efforts to support the Interim Administration’s ‘Back to School’ campaign. By the end of 2002, 3 million Afghan children – including 1 million girls – were back in the classroom. More children are on their way. UNICEF ANNUAL REPORT Covering 1 January to 31 December 2002 CONTENTS FOREWORD BY UNITED NATIONS SECRETARY-GENERAL KOFI A. ANNAN . 2 FOREWORD BY UNICEF EXECUTIVE DIRECTOR CAROL BELLAMY . 3 OUR PRIORITIES . 5 THE EARLY YEARS . 7 IMMUNIZATION ‘PLUS’ . 10 EDUCATING GIRLS . 15 FIGHTING HIV/AIDS . 18 PROTECTING CHILDREN . 23 CHILDREN LEAD . 27 NATIONAL COMMITTEES . 28 CORPORATE ALLIANCES . 30 RESOURCES AND MANAGEMENT . 32 ACHIEVING ORGANIZATIONAL EXCELLENCE . 42 GLOBAL PARTNERSHIPS . 52 UNICEF AT WORK (list of countries) . 54 GOODWILL AMBASSADORS . 56 OUR COMMITMENTS . -

5Th ETCO Annual Meeting Riga, 3-5 October 2008 Title
5th ETCO Annual Meeting Riga, 3-5 October 2008 Title: European Living Donation And Public Health (EULID) Authors: Pal-Dag Line2, Andy Maxwell4, Assumpta Ricart1, Leonídio J Silva Coelho Dias 3, Chloë Ballesté1, Irene Martínez1, David Paredes1, Jordi Vilardell1, Martí Manyalic1 and participants of the EULID Project. Institutions: 1Hospital Clínic de Barcelona, 2UHR Rikshospitalet, 3HGSA Hospital Geral de Santo Antonio, 4UK Transplant. Presenting author:Assumpta Ricart. C/Aragó, 65 4rt 4ª. 08015. Barcelona. Spain. e-mail: [email protected]. Tel: +34658518202; +34932269060 Introduction: There is no specific pronouncement of the European Union in relation to standards of quality and safety for the living donation process, and there is a great heterogeneity among European countries on the topic. European legislation, registers and systematized experiences on organ living donors (LD) are still rare. This is surprising if we compare the situation with that of the donations proceeding from deceased people or directives on quality and safety regarding human tissues and cells. We present the EULID project which aim is to establish a European common standard to guarantee LD health and safety thorough common practices and regulations. Material Twelve partner from eleven European countries (Cyprus, France, Italy, Norway, Poland, Portugal. Romania, Slovenia, Spain, Sweden and UK) work cooperatively. Partners work in four different Working Groups to establish European Communication platform: Web: http://eulivingdonor.eu/ The Project is grant-aided by the European Commission through the The Public Health Executive Agency (April2007 – October2009). Methods WG1. Legal and ethical recommendations in relation to organ LD health and safety. WG2. Recommendations in relation to LD health and safety protection practices. -

Japan: Revising Arms Export Regulation
Japan Japan Japan: Revising arms export regulation Recent changes to Japan’s ‘Three Principles on Arms while article 48 covers goods. Exports’ relax controls held tightly for decades. Legislation supporting the act includes (1) cabinet orders, (2) ministerial Crystal Pryor reviews the revisions while pointing out orders, and (3) notifications and an important gap in Japan’s munitions regulations guidance. The most important statutes under the act are two cabinet orders: the Export Trade Control Order apan is one of the frontrunners for principles to allow exports in cases that (‘ETCO’, or Yushutsu-rei) and the the sale of submarines to will contribute to global peace and Foreign Exchange Order (‘FEO’ or J Australia, vying with France and serve Japan’s security interests. The Gaitame-rei). The ETCO refers to Germany. Japan arguably produces the rules themselves were renamed the controlled goods (article 48 of the world’s best non-nuclear submarine, ‘Three Principles on Defense Trade Law) while FEO specifies its Soryu class. The Australian Equipment Transfers’. controlled technologies (article 25 of government initially approached Japan In July 2014, the Japanese the Trade Law). Ministerial orders about the $35 billion deal in 2014. It is government approved delivery of provide details like the specification of noteworthy because, if realised, it seeker gyros to the United States for listed items. Finally, notifications and would be Japan’s first major defence use in Patriot Advanced Capability-2 guidance/ notices (interpretations) sit export to a third party (i.e., not the (PAC-2) missile interceptors. (The below ministerial orders in Japan’s United States) in four decades.1 Prime PAC-2 will ultimately be sold to Qatar.) legal structure. -

Dakota Access-ETCO Exhibit 9.1
Dakota Access-ETCO Exhibit 9.1 David Harrison, Ph.D. Managing Director National Economic Research Associates, Inc. 99 High Street, 16th Floor Boston, Massachusetts 02129 +1 617 927 4500 Fax +1 617 927 4501 Direct dial: +1 617 927 4512 [email protected] David Harrison Managing Director Dr. David Harrison is a Managing Director at NERA Economic Consulting. He has extensive experience evaluating the economic effects of a wide range of policies and programs as a consultant, academic and government official. Dr. Harrison has been active in the development and economic assessment of climate change policies around the world. He and his colleagues assisted the European Commission and the UK government with the design and implementation of the European Union Emissions Trading Scheme and national European programs related to climate change, renewable policies, and energy efficiency policies. Dr. Harrison has participated in the development or evaluation of major greenhouse gas programs and proposals in the United States, including those in California, the Northeast, the Midwest and various federal initiatives, as well as programs in Europe and Australia. He has lectured frequently on climate change and related topics at numerous conferences in the United States and abroad, including those sponsored by the European Commission, the International Energy Agency, the Organization for Economic Cooperation and Development and numerous groups in North America and the Pacific Rim. Dr. Harrison has directed numerous studies of the economic impacts of policies and programs related to major energy infrastructure investments, including pipelines, power plants, petroleum and petrochemical facilities, and others. He has prepared similar economic impact studies of major technologies and policies (Airbnb, video piracy, tariffs), transportation infrastructure (airports, highways, airlines), housing and tourism activities, environmental remediation (Superfund), manufacturing and mining activities (including mining, chemical) and others. -

Development of Fisheries in the Exclusive Economic Zone of Sri Lanka
Indian Ocean Programme IOP/TEcri./?P .' 17 DEVELOPMENT OP FISHKRDJJS IN rl'HE JliXCLUSIVEl 11;coNOMIC ZONE OF SRI LANKA FDOD AND AGHICULTUffill r)RGf\fflZA'I'ION Oii' 'I'!iE UNITED NATIONS UNITED NATIONS DEVELOPME1NT PROGRAMME Horne, 19'/D ;ij, def~igne;iions omp1o;ted and the presemtation of in thirJ publioation do not imply the GfJion of nny whatsoever on the part tho J.i'ood ox1d Ag1'icnltu:n.) 0J.'gc>niza:tion of the Nations eoncEn·ning the statmJ of any v to:i'Pitm·y, cj:ty or area or of i"ts 'l;ic'1G; n<" conowrning '&he delimitation of frorrtiGl'D (H' boumlar:ieso Campleman? Go (1978) Teche Repe IndigE. _Ocean P:r·o~l:!2::'f';;11¥!!~ 7 ( 10) g 13 Po Development of fislrnrfas in the exclusive economic zone of Sri Lanka Comm®rcial fishing. Economic analysiso Feasibility. Financing. Fish<n'y developmento Fishery l'EHmurcer3o Potimtii'tl yielde ISW i Sri Lanke,. The; copyright in i;h:iD lJook hi veE.ri;ed in the Food and Ai;-riculture Organization of the United Nationso ~('he 1)ook may not l)e reproduced, in whole or in part, by a:ny mothod or procesr:;~ without written permission from the copyright holder" Applicv;ti.ons for f'ltWh permission, with &, ste,tement of the purpose and extent of the reproduction desh0 ed, chould 1Je addressed to the Director, Publications D:ivirJion~ Food ax1d Agriculture 01•ganiza.tion of the United Nations, Via delle 'rel'.'mt~ di Caracalla1 00'100 Home v Italy. -

40 Years IFSH
40 Years Institute for Peace Research and Security Policy at the University of Hamburg 19712000 1974 2007 2003 2002 2009 19991979 2006 1994 1981 2001 1983 1977 1985 1997 IFSH 2008 1998 1984 1989 1995 1973 1986 2005 19751978 1982 1992 1990 2010 1980 1988 2004IFSH 1971-2011 +++ 40 Years +++ Research - Consultancy - Teaching 1976 1993 1972 19961987 1991 2011 Institute for Peace Research and Security Policy at the University of Hamburg Beim Schlump 83, 20144 Hamburg Phone: 0049-40-866 077 0, Fax: 0049-40-866 36 15 e-mail: [email protected] www.ifsh.de Editor: Susanne Bund Translation: MDS Editing and Translation Services, 53343 Wachtberg Production: Druckerei Schierhorn, Gilbertstraße 22, 22767 Hamburg Hamburg 2011 Reproduction, including excerpts, only with the permission of IFSH. IFSH Contents The Directors of IFSH since 1971 2 The IFSH 1971 – 2011 3 Disarmament and Arms Control 5 European Security Policy – 40 Years a Topic at the IFSH 11 Leadership Development and Civic Education in the German Armed Forces A Traditional Subject of Research at IFSH 16 Consultancy at the IFSH 21 The Research Programme of the IFSH 25 Internship, Study, Doctorates The Promotion of Junior Researchers at the IFSH 29 IFSH – 40 Years of Public Relations Work 34 IFSH Chronology 38 The Authors 40 1 IFSH The Directors of IFSH since 1971 Egon Bahr, 1984 - 1994 (Photo: Holger Noß) Count Wolf von Baudissin, 1971 - 1984 (Photo: Baudissin Dokumentationszentrum) Dieter S. Lutz 1994 - 2003 Reinhard Mutz, 2003 - 2006 Michael Brzoska since 2006 2 IFSH The IFSH 1971 - 2011 It is infinitely easy to argue about whether the world has become a more peaceful place over the last four decades and life in Europe safer. -

European Trauma Course
European Trauma Course HOSPITAL CENTRAL DR. NÉLIO MENDONÇA SERVIÇO DE SAÚDE DA REGIÃO AUTÓNOMA DA MADEIRA Avenida Luiz de Camões, 57 - 9004-514 Funchal – MADEIRA ISLAND, PORTUGAL 2016, November, 19 – 21 1 COURSE DIRECTOR: SEBASTIAN KUHN COURSE CO-DIRECTOR: JAN GRIESINGER COURSE COORDINATORS: ELÁDIO CARDOSO COURSE ORGANIZERS: CARLOS MESQUITA DANIEL BARRADAS PEDRO RAMOS VÍTOR CORREIA Course organized within the framework of the Lusitanian Association for Trauma and Emergency Surgery (ALTEC-LATES), institutional member of the European Society for Trauma and Emergency Surgery (ESTES) 9th International Meeting of Trauma and Emergency Surgery THIS COURSE WILL BE SPOKEN IN ENGLISH COURSE FACULTY e-mail LUÍS FERREIRA Dublin, Ireland [email protected] JAN GRIESINGER Mainz, Germany [email protected] PIOTR KOLEDA Wroclaw, Poland [email protected] SEBASTIAN KUHN Mainz, Germany [email protected] CARLOS MESQUITA Coimbra, Portugal [email protected] MIGUEL PEREIRA Porto, Portugal [email protected] PEDRO RAMOS Funchal, Portugal [email protected] CARLOS RODRIGUES Faro, Portugal [email protected] NENAD TEUFEL Koprivnica, Croacia [email protected] JONATHAN TILSED Hull, England (UK) [email protected] DAFYDD WILLIAMS Bangor, Wales (UK) [email protected] ETC and ETCO The European Trauma Course (ETC) is a two-and-a-half-day simulation-based, hands-on course. The course is mainly practical and the candidates will be led in small groups through scenarios of increasing difficulty. The ETC is a project -

White House Special Files Box 20 Folder 4
Richard Nixon Presidential Library White House Special Files Collection Folder List Box Number Folder Number Document Date Document Type Document Description 20 4 N.D. Other Document Section 3 tab divider for "1968-1969 Presidential Transaction" by Franklin B. Lincoln, Jr. 1 pg. 20 4 09/05/1967 Report "The Presidency, Executive Staffing, and the Federal Bureaucracy" study by Laurin L. Henry. Section 3 of "1968-1969 Presidential Transaction" by Franklin B. Lincoln, Jr. 28 pgs. 20 4 N.D. Other Document Section 4 tab divider for "1968-1969 Presidential Transaction" by Franklin B. Lincoln, Jr. 1 pg. 20 4 11/11/1968 Memo Memo from Franklin B. Lincoln, Jr. to RN RE: Executive Office of the President. 11 pgs. 20 4 N.D. Other Document Section 5 tab divider for "1968-1969 Presidential Transaction" by Franklin B. Lincoln, Jr. 1 pg. 20 4 11/25/1968 Report 1968-1969 Presidential Transition report. 25 pages plus cover page and 4 page index. 30 pgs. Tuesday, September 22, 2009 Page 1 of 3 Box Number Folder Number Document Date Document Type Document Description 20 4 N.D. Other Document Tab divider "EXHIBITS" for Section 5 of "1968-1969 Presidential Transaction" by Franklin B. Lincoln, Jr. 1 pg. 20 4 11/25/1968 Report Exhibit A of Section 5 of "1968-1969 Presidential Transaction" by Franklin B. Lincoln, Jr. 10 pgs. 20 4 10/25/1968 Report Exhibit B of Section 5 of "1968-1969 Presidential Transaction" by Franklin B. Lincoln, Jr. 1 pg. 20 4 10/25/1968 Report Exhibit C of Section 5 of "1968-1969 Presidential Transaction" by Franklin B. -
Guidance for the Control of Sensitive Technologies for Security Export for Academic and Research Institutions 3Rd Edition
(Tentative translation) Guidance for the Control of Sensitive Technologies for Security Export for Academic and Research Institutions 3rd Edition October 2017 Ministry of Economy, Trade and Industry Trade Control Department Note: The tentative translation is unofficial and to be used solely as reference materials to aid in the understanding of Japanese original text. Trade Control Department of Ministry of Economy, Trade and Industry is not responsible for the accuracy, reliability or currency of translation in this translation. < Table of Contents > I. Purposes and Usages of this Guidance .....................................................................................................................4 1. Purposes of this Guidance .....................................................................................................................................4 2. Usages of this Guidance ........................................................................................................................................5 II. Security Export Control System ....................................................................................................................................6 1. System Intent and Background ..............................................................................................................................6 1) Necessity of the Security Trade Control .................................................................................................................6 2) Transition of the Security -

The German Catholic Settlers of Waterloo County
THE GERMAN-FRENCH CATHOLIC SETTLERS OF WATERLOO COUNTY, ONTARIO Robert Wideen : 2020 Soufflenheim Genealogy Research and History www.soufflenheimgenealogy.com The German-French Catholic Settlers of Waterloo County, Ontario, Canada and Surrounding Counties - The Beginnings: 1824-1850’s. Compiled by Chris Bowman, 1991-2018 Most of the individuals in this work are from Alsace, mentioned 281 times, Baden, 245, and Bavaria, 62 times. Bas-Rhin is mentioned 165 times, Haut-Rhin 32. Soufflenheim, 92 times, and the nearby villages of Schirrhein 6 and Rountzenheim 20. New Germany in Ontario, the destination of a large number of emigrants from Soufflenheim, is found 388 times. 1883 Map of Waterloo County, Ontario. New Germany center right. CONTENTS The German-French Catholic Settlers Of Waterloo County, Ontario ........................................................... 1 Introduction ................................................................................................................................................ 2 Index of Names ......................................................................................................................................... 3 Biographies ................................................................................................................................................ 5 A - D ........................................................................................................................................................... 5 E - H ........................................................................................................................................................