Public Health Annual Report 2015-16
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

NEWSLETTER of the ORKNEY FAMILY HISTORY SOCIETY No 79 September 2016
SIB FOLK NEWS NEWSLETTER OF THE ORKNEY FAMILY HISTORY SOCIETY No 79 September 2016 GRAPHICS JOHN SINCLAIR 2 NEWSLETTER OF THE ORKNEY FAMILY HISTORY SOCIETY Issue No 79 September 2016 ORKNEY FAMILY HISTORY NEWSLETTER No 79 SEPTEMBER 2016 COVER SIB HIGHLIGHTS PAGE 2 From the Chair PAGES 3,4,5 more reminiscences from Jackie Brown Pages 6 & 7 Peter's very important ancestor From PAGES 8,9,10 Norman Windwick the Chair recalls his childhood at the Toc H Welcome to the September issue of the Sib Folk News at the end of a PAGE 11 summer of lovely weather and a very busy time in the office. In Orkney as a Tumbledown 'Gyrehouse' Stenness whole, we must have had record numbers of tourists this year with over 100 cruise ships including Orkney in their itinerary plus all the holidaymakers who PAGES 12 & 13 visited our islands. The Kirkwall Shops. A stroll down The Family History Society had a table in the exhibition hall at the Vintage memory lane Rally in August and it was good to see and have a chat with our members and welcome some new ones as well. Remember, we look forward to seeing PAGES 14 & 15 you in the office if you get stuck with your research or if you just want to say Captain James 'hello'. Renton Waters The website is being updated with more interesting and helpful resources PAGES 16 & 17 Mandy Thomson bitten so don't forget to check out www.orkneyfhs.co.uk and you will be amazed by the Orkney at the amount of information freely available to our members. -

FOI) the Balfour, Foreland Road, Kirkwall, Orkney KW15 1NZ
Freedom of Information (FOI) The Balfour, Foreland Road, Kirkwall, Orkney KW15 1NZ www.ohb.scot.nhs.uk RE: Freedom of Information Request 202021 / 055 – Falls Data Your Query Date of Request June 2020 1. I would like to request any data you hold on falls from the last 5 years. a) I am looking for the total number of falls sorted by hospital from the last 5 years? b) I am looking for the total number of falls sorted by ward from the last 2 years? 2. I would also like to request all email addresses for ward managers and falls leads/groups within the trust? 3. On average how much does falls cost the trust per year? Clarification Question 2 and 3 are an expansion of question 1. I hope this clarifies for you. In addition please could the data be sorted by the last 5 full calendar years and please include any data that the trust hold for this year too. Response Please be advised that NHS Orkney is a small remote and rural health board which operates one hospital – the Balfour. 1. a) Please note the methodology for measuring falls locally has changed over time. The methodology used for collecting this data is different from previous years. The data provided excludes any falls as a result of ‘assisted lowering’ which were counted in previous years. The total of excluded falls using the new methodology is 4 for 2019 and 3 for 2020. Year 2015 2016 2017 2018 2019 2020 Number of 63 82 113 88 103 *42 patient falls recorded *As at 25/06/2020. -
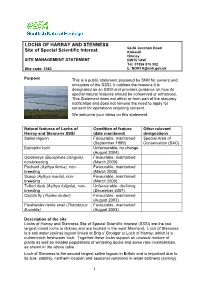
Lochs of Harray and Stenness Site of Special Scientific Interest (SSSI) Are the Two Largest Inland Lochs in Orkney and Are Located in the West Mainland
LOCHS OF HARRAY AND STENNESS 54-56 Junction Road Site of Special Scientific Interest Kirkwall Orkney SITE MANAGEMENT STATEMENT KW15 1AW Tel: 01856 875 302 Site code: 1083 E: [email protected] Purpose This is a public statement prepared by SNH for owners and occupiers of the SSSI. It outlines the reasons it is designated as an SSSI and provides guidance on how its special natural features should be conserved or enhanced. This Statement does not affect or form part of the statutory notification and does not remove the need to apply for consent for operations requiring consent. We welcome your views on this statement. Natural features of Lochs of Condition of feature Other relevant Harray and Stenness SSSI (date monitored) designations Saline lagoon Favourable, maintained Special Area of (September 1999) Conservation (SAC) Eutrophic loch Unfavourable, no change (August 2004) Goldeneye (Bucephala clangula), Favourable, maintained non-breeding (March 2000) Pochard (Aythya ferina), non- Favourable, maintained breeding (March 2000) Scaup (Aythya marila), non- Favourable, maintained breeding (March 2000) Tufted duck (Aythya fuligula), non- Unfavourable, declining breeding (December 2007) Caddis fly (Ylodes reuteri) Favourable, maintained (August 2003) Freshwater nerite snail (Theodoxus Favourable, maintained fluviatilis) (August 2003) Description of the site Lochs of Harray and Stenness Site of Special Scientific Interest (SSSI) are the two largest inland lochs in Orkney and are located in the west Mainland. Loch of Stenness is a salt water (saline) lagoon linked at Brig o’ Brodgar to Loch of Harray, which is a nutrient-rich freshwater loch. Together these lochs support an unusual mixture of plants as well as notable populations of wintering ducks and some rare invertebrates, as shown in the above table. -

A Warm Welcome to Dounby Community School
Parents & Carers Information Booklet 2020-21 CONTENTS Vision, Values and Aims ................................................................... 1 Quick Contact List ........................................................................... 2 About Our School ............................................................................. 3 School Staff ...................................................................................... 5 Managing Covid-19 in School .......................................................... 6 Keeping You Informed ..................................................................... 7 School Organisation ......................................................................... 8 School Calendar ................................................................................. 9 Being Absent ...................................................................................... 10 Daily Checklist ................................................................................... 10 Play and School Clubs ....................................................................... 14 Curriculum........................................................................................... 15 Religious Observance & Learning .................................................. 18 Working with Parents and Carers ................................................. 19 Pupil Council ........................................................................................ 21 Additional Learning Needs ............................................................ -

Festive Period Domestic and Commercial Refuse Collections
Festive Period Domestic and Commercial Refuse Collections Mainland and Linked South Isles Domestic and commercial refuse collection days over the Christmas and New Year period are listed below. Regular waste collections will resume on Monday 6 January 2020. Domestic and Fortnightly Trade Refuse Collections Area. Normally Collected. Refuse Collection Dates. Area 1 – Kirkwall (Central and North West). Monday. Monday 23 December. Area 3 – Kirkwall (Central). Wednesday. Monday 23 December. Area 6 – East Holm, Deerness, Tankerness and Toab. Monday. Monday 23 December. Area 2 – Kirkwall (West). Tuesday. Tuesday 24 December. Area 7 – Kirkwall (South), Holm, Burray (North). Tuesday. Tuesday 24 December. Area 8 – South Ronaldsay and Burray (South). Wednesday. Tuesday 24 December. Area 4 – Kirkwall (South East). Thursday. Friday 27 December. Area 5 – Kirkwall (North East). Friday. Friday 27 December. Area 9 – Stromness (Central). Monday. Monday 30 December. Area 11 –Stromness (Outer), Sandwick and Birsay. Wednesday. Monday 30 December. Area 10 – Stromness (Outer Areas) and Stenness (West). Tuesday. Tuesday 31 December. Area 12 – Dounby, Birsay and Evie. Thursday. Friday 3 January 2020. Area 13 – Firth, Rendall, Evie and Harray. Friday. Friday 3 January 2020. Area 14 – Finstown, Stenness (East) and Harray. Thursday. Friday 3 January 2020. Area. Normally Collected. Refuse Collection Dates. Area 15 – Orphir and Stenness (West). Friday. Friday 3 January 2020. Domestic Recycling Information Please note alterations for domestic recycling collection over the festive period. Recycling centres will remain open – see separate advert for opening times. Area: Last recycling collection: Next recycling collection: Area 1 – Kirkwall (Central and North West). Monday 16 December. Monday 13 January 2020. Area 6 – East Holm, Deerness, Tankerness and Toab. -

Catte List 11 March 19.Xlsx
Monday 11 March 2019 - Special Sale of Store Cattle TIMES APPROX. ISLES 10:45 Johnston, Hewan, Shapinsay 1-14 Miller, Haquoy, Shapinsay 15-22 Meason, Frustigarth, Shapinsay 23-33 Trenabie Farms, Trenabie, Westray 34-35 Mainland, Nearhouse, Rousay 36-65 Leslie, Lopness, Sanday 66-76 Rendall, Braefoot, Shapinsay 77-88 Scott, Skaill, Westray 89-100 MAINLAND 11:25 Thomson, Cockmurra, Holm 404-407 Scott, Redland, Firth 408-414 Sandison, Hindatoon, Harray 415-440 Sinclair, Midhouse, Harray 441-452 Stevenson, Bridgend, Orphir 453-462 Smith, Lower Cornquoy, Holm 463-471 Appietown Farms, Rendall 195-258 ISLES 12:10 Stout, Kirkbrae, Westray 101-140 Leslie, Chapelbrae, Westray 141-150 Bain, Twiness, Westray 151-167 Harcus, Branstane, Westray 168-177 How Farms, How, Sanday 178-189 Seatter, Hammer, Westray 190-194 MAINLAND 12:45 Miller, Roadside, St Ola 472-475 Seator, Grimbister, Firth 476-485 Groat, Cloke, Dounby 486 Hourston, Bigging Cottage, Dounby 487-489 Flett, Nistaben, Harray 490-493 Paterson, Veltigar, Tankerness 494-513 Ross, Lenahowe, Sandwick 514-521 Brown, Glebe, Firth 522-531 Stephen, Sandwick House, South Ronaldsay 532-539 Biggings Farm, Biggings, Stenness 305-338 13:25 Brown, Newhall, Stromness 259-273 Fraser, Westshore, Rendall 274-285 Scott, Netherhill, Tankerness 286-297 Scott, Weethick, Tankerness 298-302 Low, Craighaven, Toab 303-304 Moar, Rosebank, Deerness 540 Sinclair, Braeland, South Ronaldsay 541-544 Maesquoy Farms, Harray 545-574 Sinclair, Karinya, Dounby 575-584 Baillie, Biggings, Toab 585-621 & 1622 14:10 Flett, Hurtiso, -

Orkney Winter Plan 2020/21
Gillian Morrison (Interim Chief Officer). Orkney Health and Care. 01856873535 extension: 2611. [email protected] Agenda Item: 11. Integration Joint Board Date of Meeting: 10 February 2021. Subject: Orkney Winter Plan 2020/21. 1. Summary 1.1. This is a whole system plan which aims to address the predicted additional pressures of winter across 2020/21 alongside the ongoing COVID-19 pandemic. Delivery of this plan will require strong leadership and collaborative working across the health and social care system at the most senior level to provide a focus on the additional impacts, challenges and resources required to sustain safe, effective and person centred care. 2. Purpose 2.1. The purpose of this paper is to present the Integration Joint Board with the draft Orkney Winter Plan 2020/21 for consideration and approval. 3. Recommendations The Integration Joint Board is invited to: 3.1. Approve the Orkney Winter Plan 2020/21, attached as Appendix 1 to this report. 4. Background 4.1. NHS Orkney, in common with other health boards, is expected to prepare a Winter Plan, in partnership based on national guidance and from lessons learned the previous year. 4.2. The Winter Plan, attached as Appendix 1 to this report, aims to create a set of conditions which improve resilience by building capability to absorb, respond and recover from disruptive challenges. Winter disruptions can include increased demand and activity due to seasonal flu, respiratory and circulatory illness; increased numbers of falls and trips; and wards closed to admission due to higher levels of norovirus. 4.3. Given the ongoing emergency footing and the COVID-19 pandemic, planning for this winter where there is a high likelihood of concurrent events is critical in ensuring services are best placed to meet the demands which are likely to be placed on them. -

Heart of Neolithic Orkney World Heritage Site the Consultation Was Carried out in January and February 2020
THE COMMUNITY VIEW Heart of Neolithic Orkney World Heritage Site The consultation was carried out in January and February 2020. Contents Introduction 3 Community engagement 4 What the Heart of Neolithic Orkney 8 World Heritage Site means to the Orkney community How tourism impacts Orkney 12 Managing the Heart of Neolithic 18 Orkney World Heritage Site now and in the future Community priorities 24 for the next 5 years Next steps 32 1 2 Introduction Orkney’s most famous archaeological treasures — Skara Brae, the Ring of Brodgar, the Stones of Stenness, and the Maeshowe chambered tomb — form the keystones of the UNESCO Heart of Neolithic Orkney World Heritage Site (WHS). The site is managed by Historic Environment Scotland on behalf of Scottish Ministers, along with partners Orkney Islands Council, Scottish Natural Heritage and the Royal Society for the Protection of Birds. These organisations form the World Heritage Site Steering Group, supported by Highlands and Islands Enterprise and the University of the Highlands and Islands Archaeology Institute. The key aims and actions that are in place to manage the site are reviewed and updated every fve years and incorporated into the Management Plan for the site. To inform the next Management Plan for 2020-25, due out later this year, the Steering Group wanted to fnd out more about how Orcadians felt about the WHS and how the management of the site affected them. To do this, the Steering Group commissioned an independent consultant to run a community engagement exercise. The feedback that local people have provided will help the Steering Group to create a management plan that balances different aspects of the WHS like tourism and conservation of the monuments with the daily lives of the islanders. -

BADMINTON on Sunday 23 April the Final Competition in the Orkney
BADMINTON On Sunday 23 April the final competition in the Orkney Badminton Association fixture was played in the Pickaquoy Centre - the Primary Schools Badminton Team Competition. It was good to see 12 teams competing, two more than last year. There were first time appearances from Stenness and St Margarets Hope and both teams performed well on the day. The event ran smoothly and resulted in some very close and exciting matches throughout the placings. Teams: Papdale Primary Team 1 - Owen Reid, Joe Sutherland, Lianne Bruce & Nicola Kemp. Papdale Primary Team 2 – Cameron Barbour, Craig Sutherland, Nicola Sutherland & Laura Martin. Adult helper – Calvin Reid & Mrs Sutherland St Margarets Hope Primary – Leona Norquoy, Leanne Omand, Aiden drever & Andrew Stevenson. Adult helper – Mrs Norquoy St Andrews Primary Team 1 – Liam Delday, Simon Loudon, Aimee Drever & Helen Moar. St Andrews Primary Team 2 – Joseph Mills, Callum Lewis, Fiona Moar & Judith Bonner. St Andrews Primary Team 3 – Craig Rendall, Samuel Murray, Stephanie Moar & Catriona Ward. Adult helpers – Fiona MacNab & Linda Bonner. Dounby Primary – Ryan Major, Scott Davidson, Isla Kirkness & Alanna Swanney. Adult helper – Anne Davidson. Stromness Primary – Theo Prendergast, Graeme Bain, Morna Brown & Trisbee Sinclair. Adult helper – Matilda Prendergast & Josh Prendergast. Stenness Primary – Lewis Moar, Garry Mathers, Sisie Manson & Jody Spence. Adult helpers – Mrs Kennedy, Jill Manson & parents. Glaitness Primary Team 1 – Mathew Reid, Thorfinn Manson, Sarah Cowie & Catrin Sutherland. Glaitness Primary Team 2 – Jamie Firth, Max Harris Jones, Rhiann Mackay & Aimee Garrioch. Glaitness Primary Team 3 – Duncan MacLean, Andrew Reid, Claire Johnston & Thora Cant. Adult helpers – Lesley Mackay & Lorna Reid. The competition was played in the initial stages with four groups competing for places into the final stages. -

Capital Sights in Kirkwall Montage by John Sinclair 2 NEWSLETTER of the ORKNEY FAMILY HISTORY SOCIETY Issue No 54 June 2010
NEWSLETTER OFSIB THE ORKNEY FAMILY FOLK HISTORY SOCIETY NEWSISSUE No 54 June 2010 Tankerness House 16th Cent. St Olaf’s Church Doorway 11th cent Moosie Too’er 16th Cent. St Magnus Cathedral 12th-15th cent. Victoria Street Orkney Library & Archive where OFHS is located Gow’s Folly Sports, arts, leisure and cinema complex Albert Street and the ‘big tree’ Capital sights in Kirkwall Montage by John Sinclair 2 NEWSLETTER OF THE ORKNEY FAMILY HISTORY SOCIETY Issue No 54 June 2010 ORKNEY FAMILY HISTORY NEWSLETTER Issue No 54 June2010 CONTENTS FRONT COVER From the chair Capital sights in Kirkwall I am sure you are looking forward to your summer holidays whether PAGE 2 you seek the sun, beach and sand or a nice cruise, it is an opportunity From the Chair to relax with family and friends. Orkney will again see many visitors and, as in past years, the Society will welcome many who return to PAGE 3 find that elusive Orcadian ancestor or to experience returning to one’s Tumbledown– 'Newhouse' homeland. The Society’s Annual General Meeting was held in May and I was PAGES 4, & 5 honoured to be re-elected as your chairperson for another year. I was pleased to report on a very North Walls & positive year past and on how the committee have created more opportunities for members and better Brims 1861 access to resources via our website. This has been particularly beneficial to our overseas members population 10 years on who have seen greater benefits for their family history research. We have seen further growth in membership. -

NEWSLETTER of the ORKNEY FAMILY HISTORY SOCIETY Issue No 57 March 2011
NEWSLETTER OFSIB THE ORKNEY FAMILY FOLK HISTORY SOCIETY NEWSISSUE No 57 MARCH 2011 graphics John Sinclair 2 NEWSLETTER OF THE ORKNEY FAMILY HISTORY SOCIETY Issue No 57 March 2011 ORKNEY FAMILY HISTORY NEWSLETTER Issue No 57 March 2011 CONTENTS FRONT COVER Spring From has Sprung the chair PAGE 2 From the Chair As the economic recession starts to impact on people’s lives, PAGE 3 there are likely to be many changes over this next year. In Tumbledown Orkney, the Council has been consulting with the Orkney 'UPPERTOWN' community under the banner of “Tough Times – Tough Choices”. When researching one’s family history you do not PAGES 4,5 & 6 have to go back that many years when the same could have Capt. John Robert Arthurson equally described the lives of our forbearers. In reality their predicament was probably 20 times worse than what we have to face. Our committee is now back to full strength and we welcome Morag Sinclair on to our PAGE 7 Orkney Picnic. committee. Membership continues to grow with the Society now with over 2,500 members Tumbledown since its inception. Correction The 2011 programme began in February with a talk by David Eaton on “Momento Mori” – (How we commemorate the Dead). His slide show highlighted various styles of gravestones and tombs; their inscriptions, symbolism and other aspects of how past PAGE 8 The 1911 Census generations have commemorated their ancestor’s lives and deaths. Our March programme again explores the web with an emphasis of “Emigration Records” PAGE 9 and other new sites. There continues to be expansion in the range of Website resources 'Life un the targeted at the family history market. -

Muce, Dounby, Orkney, KW17 2HS
Muce, Dounby, Orkney, KW17 2HS 3 bedroom detached house situated on the outskirts of There is parking to the side and a large garage and coal shed. Dounby. Dounby Village is very close by with a Convenience Store, Post The property enjoys beautiful views over neighbouring Office, Butcher, Primary School, Doctors Surgery, Church and a farmland and out towards Hoy Hills. Hotel. Muce has solid fuel central heating run off a Charnwood multi Accommodation comprises of entrance hall, kitchen, stairs to fuel stove in the kitchen. There are double glazed windows bedroom 2, ensuite, sitting room, shower room, hall, bedrooms and doors throughout. 1 and stairs to bedroom 3. The property has a large garden to the front which is mainly This property offers great potential in a popular part of the West laid to lawn with mature bushes and shrubs. The rear is also Mainland. laid to lawn with a drying line. Offers over £135,000 Entrance Hall (7’ 06” x 4’ 01”): Exterior door, tiled flooring, cupboard under stairs with coat hooks, metre cupboard, opening to kitchen and door to sitting room. Kitchen (14’ 03” x 11’ 05”): Tiled flooring, 2 x windows, multifuel stove, double storage cupboard housing hot tank with shelving, kitchen units with worktop above, stainless steel sink with drainer, Beko gas cooker, space for tumble dryer, fridge freezer, plumbing for washing machine and dishwasher. Door to stairs leading to bedroom 2. Bedroom 2 (17’ 01” x 10’ 10”): Stairs, 3 x eaves storage cupboards, carpet, velux, door to ensuite. Ensuite (11’ 09” x 8’ 11”): Carpet, eaves storage, roll top standalone bath, wall heater, WC and WHB.