Phytochemical and Antimicrobial Activity Investigation of Nicandra Physaloides Gaertn (Solanaceae)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
PLANTS of the CURIMATAÚ PARAIBANO Valdeci F
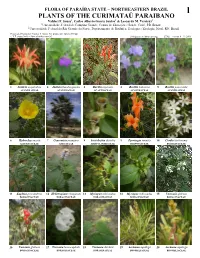
FLORA OF PARAÍBA STATE – NORTHEASTERN BRAZIL 1 PLANTS OF THE CURIMATAÚ PARAIBANO Valdeci F. Sousa1, Carlos Alberto Garcia Santos1 & Leonardo M. Versieux2 1 Universidade Federal de Campina Grande, Centro de Educação e Saúde, Cuité, PB, Brazil 2 Universidade Federal do Rio Grande do Norte, Departamento de Botânica, Ecologia e Zoologia, Natal, RN, Brazil Photos and Production: Valdeci F. Sousa. Pós-production: Juliana Philipp. © V.F. Sousa [[email protected]]. [fieldguides.fieldmuseum.org] [776] version 1 11/2019 1 Justicia aequilabris 2 Justicia thunbergioides 3 Ruellia asperula 4 Ruellia bahiensis 5 Ruellia paniculata ACANTHACEAE ACANTHACEAE ACANTHACEAE ACANTHACEAE ACANTHACEAE 6 Hydrocleys martii 7 Copernicia prunifera 8 Aristolochia disticha 9 Pyrostegia venusta 10 Cordia trichotoma ALISMATACEAE ARECACEAE ARISTOLOCHIACEAE BIGNONIACEAE BORAGINACEAE 11 Euploca procumbens 12 Heliotropium elongatum 13 Myriopus rubicundus 14 Myriopus rubicundus 15 Varronia globosa BORAGINACEAE BORAGINACEAE BORAGINACEAE BORAGINACEAE BORAGINACEAE 16 Varronia globosa 17 Varronia leucocephala 18 Varronia dardani 19 Aechmea aquilega 20 Aechmea aquilega BORAGINACEAE BORAGINACEAE BORAGINACEAE BROMELIACEAE BROMELIACEAE FLORA OF PARAÍBA STATE – NORTHEASTERN BRAZIL PLANTS OF THE CURIMATAÚ PARAIBANO 2 Valdeci F. Sousa1, Carlos Alberto Garcia Santos1 & Leonardo M. Versieux2 1 Universidade Federal de Campina Grande, Centro de Educação e Saúde, Cuité, PB, Brazil 2 Universidade Federal do Rio Grande do Norte, Departamento de Botânica, Ecologia e Zoologia, Natal, -

Physalis Peruviana Linnaeus, the Multiple Properties of a Highly Functional Fruit: a Review
Review Physalis peruviana Linnaeus, the multiple properties of a highly functional fruit: A review Luis A. Puente a,⁎, Claudia A. Pinto-Muñoz a, Eduardo S. Castro a, Misael Cortés b a Universidad de Chile, Departamento de Ciencia de los Alimentos y Tecnología Química. Av. Vicuña Mackenna 20, Casilla, Santiago, Chile b Universidad Nacional de Colombia, Facultad de Ciencias Agropecuarias, Departamento de Ingeniería Agrícola y de Alimento, A.A. 568 Medellin Colombia abstract The main objective of this work is to spread the physicochemical and nutritional characteristics of the Physalis peruviana L. fruit and the relation of their physiologically active components with beneficial effects on human health, through scientifically proven information. It also describes their optical and mechanical properties and presents micrographs of the complex microstructure of P. peruviana L. fruit and studies on the antioxidant Keywords: capacity of polyphenols present in this fruit. Physalis peruviana Bioactive compounds Functional food Physalins Withanolides Contents 1. Introduction .............................................................. 1733 2. Uses and medicinal properties of the fruit ................................................ 1734 3. Microstructural analysis ........................................................ 1734 4. Mechanical properties of the fruit .................................................... 1735 5. Optical properties of the fruit ...................................................... 1735 6. Antioxidant properties of fruit -

The Cape Gooseberry and the Mexican Husk Tomato
MORTON AND RUSSELL: CAPE GOOSEBERRY 261 LITERATURE CITED Seedling Plantings in Hawaii. Hawaii Agric. Expt. Sta. Bui. 79: 1-26. 1938. 1. Pope, W. T. The Macadamia Nut in Hawaii. 10. Howes, F. N. Nuts, Their Production and Hawaii Agric. Exp. Sta. Bui. 59: 1-23. 1929. Everyday Use. 264 pp. London, Faber & Faber. 2. Hamilton, R. A. and Storey, W. B. Macadamia 1953. Nut Varieties for Hawaii Orchards. Hawaii Farm Sci., 11. Cooil, Bruce J. Hawaii Agric. Exp. Sta. Bien 2: (4). 1954. nial Report—1950-52: p. 56. ft. Chell, Edwin and Morrison, F. R. The Cultiva 12. Beaumont, J. H. and Moltzau, R. H. Nursery tion and Exploitation of the Australian Nut. Sydney, Propagation and Topworking of the Macadamia. Ha Tech. Museum Bui. 20: 1935. waii Agric?. Exp. Sta. Cir. 13: 1-28. 1937. 4. Francis, W. D. Australian Rain Forest Trees. 13. Fukunaga. Edward T. Grafting and Topwork 469 pp. Sydney and London, Angus and Robertson: ing the Macadamia. Univ. of Hawaii Agric. Ext. Cir. 1951 58: 1-8. 1951. 5. Bailey, L. H. Manual of Cultivated Plants. N. Y.f 14. Storey, W. B., Hamilton, R. A. and Fukunaga, McMillan. 1949. E. T. The Relationship of Nodal Structures to Train 6. Chandler, Wm. H. Evergreen Orchards. 352 pp.: ing Macadamia Trees. Am. Soc. Hort. Sci. Proc. 61: Philadelphia, Lea & Febiger. 1950. pp. 317-323. 1953. 7. Schroeder, C. A. The Macadamia Nut. Calif. 15. Anonymous. Insect Pests and Diseases of Agric, p. 3: April 1954. Plants. Queensland Agriculture and Pastoral Hand 8. Miller, Carey D. -

Appendix Color Plates of Solanales Species
Appendix Color Plates of Solanales Species The first half of the color plates (Plates 1–8) shows a selection of phytochemically prominent solanaceous species, the second half (Plates 9–16) a selection of convol- vulaceous counterparts. The scientific name of the species in bold (for authorities see text and tables) may be followed (in brackets) by a frequently used though invalid synonym and/or a common name if existent. The next information refers to the habitus, origin/natural distribution, and – if applicable – cultivation. If more than one photograph is shown for a certain species there will be explanations for each of them. Finally, section numbers of the phytochemical Chapters 3–8 are given, where the respective species are discussed. The individually combined occurrence of sec- ondary metabolites from different structural classes characterizes every species. However, it has to be remembered that a small number of citations does not neces- sarily indicate a poorer secondary metabolism in a respective species compared with others; this may just be due to less studies being carried out. Solanaceae Plate 1a Anthocercis littorea (yellow tailflower): erect or rarely sprawling shrub (to 3 m); W- and SW-Australia; Sects. 3.1 / 3.4 Plate 1b, c Atropa belladonna (deadly nightshade): erect herbaceous perennial plant (to 1.5 m); Europe to central Asia (naturalized: N-USA; cultivated as a medicinal plant); b fruiting twig; c flowers, unripe (green) and ripe (black) berries; Sects. 3.1 / 3.3.2 / 3.4 / 3.5 / 6.5.2 / 7.5.1 / 7.7.2 / 7.7.4.3 Plate 1d Brugmansia versicolor (angel’s trumpet): shrub or small tree (to 5 m); tropical parts of Ecuador west of the Andes (cultivated as an ornamental in tropical and subtropical regions); Sect. -

Of Physalis Longifolia in the U.S
The Ethnobotany and Ethnopharmacology of Wild Tomatillos, Physalis longifolia Nutt., and Related Physalis Species: A Review1 ,2 3 2 2 KELLY KINDSCHER* ,QUINN LONG ,STEVE CORBETT ,KIRSTEN BOSNAK , 2 4 5 HILLARY LORING ,MARK COHEN , AND BARBARA N. TIMMERMANN 2Kansas Biological Survey, University of Kansas, Lawrence, KS, USA 3Missouri Botanical Garden, St. Louis, MO, USA 4Department of Surgery, University of Kansas Medical Center, Kansas City, KS, USA 5Department of Medicinal Chemistry, University of Kansas, Lawrence, KS, USA *Corresponding author; e-mail: [email protected] The Ethnobotany and Ethnopharmacology of Wild Tomatillos, Physalis longifolia Nutt., and Related Physalis Species: A Review. The wild tomatillo, Physalis longifolia Nutt., and related species have been important wild-harvested foods and medicinal plants. This paper reviews their traditional use as food and medicine; it also discusses taxonomic difficulties and provides information on recent medicinal chemistry discoveries within this and related species. Subtle morphological differences recognized by taxonomists to distinguish this species from closely related taxa can be confusing to botanists and ethnobotanists, and many of these differences are not considered to be important by indigenous people. Therefore, the food and medicinal uses reported here include information for P. longifolia, as well as uses for several related taxa found north of Mexico. The importance of wild Physalis species as food is reported by many tribes, and its long history of use is evidenced by frequent discovery in archaeological sites. These plants may have been cultivated, or “tended,” by Pueblo farmers and other tribes. The importance of this plant as medicine is made evident through its historical ethnobotanical use, information in recent literature on Physalis species pharmacology, and our Native Medicinal Plant Research Program’s recent discovery of 14 new natural products, some of which have potent anti-cancer activity. -

JABG01P351 Horton.Pdf
JOURNAL of the ADELAIDE BOTANIC GARDENS AN OPEN ACCESS JOURNAL FOR AUSTRALIAN SYSTEMATIC BOTANY flora.sa.gov.au/jabg Published by the STATE HERBARIUM OF SOUTH AUSTRALIA on behalf of the BOARD OF THE BOTANIC GARDENS AND STATE HERBARIUM © Board of the Botanic Gardens and State Herbarium, Adelaide, South Australia © Department of Environment, Water and Natural Resources, Government of South Australia All rights reserved State Herbarium of South Australia PO Box 2732 Kent Town SA 5071 Australia J. Adelaide Bot Gard. 1(6): 351-356 (1979) TAXONOMIC ACCOUNT OF NICANDRA (SOLANACEAE) IN AUSTRALIA Philippa Horton Waite Agricultural Research Institute, University of Adelaide, P. Bag 1, Glen Osmond, South Australia 5064 Abstract Nicandra, of which there is only one species, N. physalodes (L.) Gaertn., is a native of Peru and has become naturalized in many tropical and temperate regions of the world. In Australia it is a weedy species occurring mainly in cleared or disturbed sites and on cultivated ground, mostly in the eastern coastal region. A description of the species based on Australian material is presented and its distribution in Australia is mapped. Introduction Nicandra physalodes, the only species in the genus (family Solanaceae) and nativeto Peru, has become a well-established member of the Australian flora. It has been cultivatedas an ornamental garden plant in Australia and elsewhere, and is now widely dispersed in tropical and temperate areas. N. physalodes has been suspected of poisoning stock, but feeding experiments in New South Wales in which thegreen berries and the plant were tested on sheep and a goat gave negative results (Hurst, 1942). -

Withaferin-A—A Natural Anticancer Agent with Pleitropic Mechanisms of Action
International Journal of Molecular Sciences Review Withaferin-A—A Natural Anticancer Agent with Pleitropic Mechanisms of Action In-Chul Lee 1 and Bu Young Choi 2,* 1 Department of Cosmetic science, Seowon University, Cheongju, Chungbuk 361-742, Korea; [email protected] 2 Department of Pharmaceutical Science & Engineering, Seowon University, Cheongju, Chungbuk 361-742, Korea * Correspondence: [email protected]; Tel.: +82-43-299-8411 Academic Editor: Ge Zhang Received: 18 January 2016; Accepted: 17 February 2016; Published: 4 March 2016 Abstract: Cancer, being the second leading cause of mortality, exists as a formidable health challenge. In spite of our enormous efforts, the emerging complexities in the molecular nature of disease progression limit the real success in finding an effective cancer cure. It is now conceivable that cancer is, in fact, a progressive illness, and the morbidity and mortality from cancer can be reduced by interfering with various oncogenic signaling pathways. A wide variety of structurally diverse classes of bioactive phytochemicals have been shown to exert anticancer effects in a large number of preclinical studies. Multiple lines of evidence suggest that withaferin-A can prevent the development of cancers of various histotypes. Accumulating data from different rodent models and cell culture experiments have revealed that withaferin-A suppresses experimentally induced carcinogenesis, largely by virtue of its potent anti-oxidative, anti-inflammatory, anti-proliferative and apoptosis-inducing properties. Moreover, withaferin-A sensitizes resistant cancer cells to existing chemotherapeutic agents. The purpose of this review is to highlight the mechanistic aspects underlying anticancer effects of withaferin-A. Keywords: withaferin-A; phytochemical; cancer; chemoprevention; chemotherapy 1. -
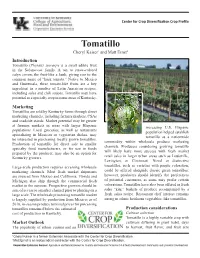
Tomatillo Cheryl Kaiser1 and Matt Ernst2 Introduction Tomatillo (Physalis Ixocarp) Is a Small Edible Fruit in the Solanaceae Family
Center for Crop Diversification Crop Profile Tomatillo Cheryl Kaiser1 and Matt Ernst2 Introduction Tomatillo (Physalis ixocarp) is a small edible fruit in the Solanaceae family. A tan to straw-colored calyx covers the fruit-like a husk, giving rise to the common name of “husk tomato.” Native to Mexico and Guatemala, these tomato-like fruits are a key ingredient in a number of Latin American recipes, including salsa and chili sauces. Tomatillo may have potential as a specialty crop in some areas of Kentucky. Marketing Tomatillos are sold by Kentucky farms through direct marketing channels, including farmers markets, CSAs and roadside stands. Market potential may be greater at farmers markets in areas with larger Hispanic increasing U.S. Hispanic populations. Local groceries, as well as restaurants population helped establish specializing in Mexican or vegetarian dishes, may tomatillo as a nationwide be interested in purchasing locally grown tomatillos. commodity within wholesale produce marketing Production of tomatillo for direct sale to smaller channels. Producers considering growing tomatillo specialty food manufacturers, or for use in foods will likely have more success with fresh market prepared by the producer, may also be an option for Kentucky growers. retail sales in larger urban areas such as Louisville, Lexington, or Cincinnati. Novel or distinctive Large-scale production requires accessing wholesale tomatillos, such as varieties with purple coloration, marketing channels. Most fresh market shipments could be offered alongside classic green tomatillos; are sourced from Mexico and California; Florida and however, producers should identify the preferences Michigan also ship through the commercial fresh of potential customers, as some may prefer certain market in the summer. -

Withania Somnifera
1 2 Letter from the Publisher Amanda Klenner Ashwagandha is one of the best-known Ayurvedic herbs used in Western herbalism, and has thousands of years of traditional use in India as a rasāyana (rejuvenative) and an adaptogen. Its name means “smell of the stallion” or “strength of a stallion,” depending on the translator. Some say it is because Ashwagandha tea smells like horse sweat. I disagree. I choose to believe it is because ashwagandha is brilliant at helping us gain strength, stamina, and vigor. As an adaptogen, ashwagandha can moderate stress and immune responses by supporting healthy function of the Hypothalamus- Pituitary-Adrenal (HPA) axis. In other words, it helps reduce our stress hormones, balance our hormones, and nourish the body in a generally safe and effective way. Because of its popularity, it has been studied extensively and is being incorporated into medical treatments for people recovering both from basic illness and from damage done to the body by chemotherapy and radiation. I myself have just come out of having a nasty flu, and am still suffering side effects from it. I am taking ashwagandha and some other adaptogens to help me recover my vitality and nourish my body after a long and debilitating illness. Traditionally, ashwagandha is used in Ayurveda to help balance those with Kapha and Vata leanings, who both tend toward a cold constitution. Kapha people, when imbalanced, are stagnant, damp, and slow. Vata people are scattered, thin, cold, dry, and always busy, but not often in a functional way, when they’re out of balance. -

Morphological Studies of Medicinal Plant of Withania Somnifera (L.) Dunal Grown in Heavy Metal Treated (Contaminated) Soil
Journal of Pharmacognosy and Phytochemistry 2014; 3 (1): 37-42 ISSN 2278-4136 ISSN 2349-8234 Morphological studies of medicinal plant of Withania JPP 2014; 3 (1): 37-42 Received: 24-03-2014 somnifera (L.) Dunal grown in heavy metal treated Accepted: 12-04-2014 (contaminated) soil. Ch. Saidulu Department of Botany, University College of Science, Osmania Ch. Saidulu, C. Venkateshwar, S. Gangadhar Rao University, Hyderabad-500007, Andhra Pradesh, India. Email:[email protected] ABSTRACT Tel: +91-09010730301 Plants were grown in pot culture experiments with three treatments in black soil, Treatment No I, a control without any addition to the soil, Treatment No II, Cadmium 10ppm, Chromium 20ppm, Nickel 16ppm C. Venkateshwar were introduced into the soil, Treatment No III, one % of Calcium hydroxide was also added along with Department of Botany, University College of Science, Osmania heavy metals to soil and was grown up to the productivity levels. To know the effect of the heavy metals University, Hyderabad-500007, on the growth and development of Withania somnifera plants, the study of macro morphology of external Andhra Pradesh, India. character was undertaken. Productivity was reduced in the plants grown in heavy metal treated plants Email: [email protected] compared to control plants. The experimental data revealed that the external morphology plants i.e., Plant Tel: +91-09440487742 height (cms), No of branches reduced in (Treatment No II) heavy metals treated plants and also was increased in No. of leaves compared to control plants and heavy metals + Calcium hydroxide treated S. Gangadhar Rao Department of Botany, University plants. The No. -

The Complete Genome Sequence, Occurrence and Host Range Of
Li et al. Virology Journal (2017) 14:15 DOI 10.1186/s12985-016-0676-2 RESEARCH Open Access The complete genome sequence, occurrence and host range of Tomato mottle mosaic virus Chinese isolate Yueyue Li1†, Yang Wang1†, John Hu2, Long Xiao1, Guanlin Tan1,3, Pingxiu Lan1, Yong Liu4* and Fan Li1* Abstract Background: Tomato mottle mosaic virus (ToMMV) is a recently identified species in the genus Tobamovirus and was first reported from a greenhouse tomato sample collected in Mexico in 2013. In August 2013, ToMMV was detected on peppers (Capsicum spp.) in China. However, little is known about the molecular and biological characteristics of ToMMV. Methods: Reverse transcription-polymerase chain reaction (RT-PCR) and rapid identification of cDNA ends (RACE) were carried out to obtain the complete genomic sequences of ToMMV. Sap transmission was used to test the host range and pathogenicity of ToMMV. Results: The full-length genomes of two ToMMV isolates infecting peppers in Yunnan Province and Tibet Autonomous Region of China were determined and analyzed. The complete genomic sequences of both ToMMV isolates consisted of 6399 nucleotides and contained four open reading frames (ORFs) encoding 126, 183, 30 and 18 kDa proteins from the 5’ to 3’ end, respectively. Overall similarities of the ToMMV genome sequence to those of the other tobamoviruses available in GenBank ranged from 49.6% to 84.3%. Phylogenetic analyses of the sequences of full-genome nucleotide and the amino acids of its four proteins confirmed that ToMMV was most closely related to Tomato mosaic virus (ToMV). According to the genetic structure, host of origin and phylogenetic relationships, the available 32 tobamoviruses could be divided into at least eight subgroups based on the host plant family they infect: Solanaceae-, Brassicaceae-, Cactaceae-, Apocynaceae-, Cucurbitaceae-, Malvaceae-, Leguminosae-, and Passifloraceae-infecting subgroups. -

Herbal Remedies and Their Possible Effect on the Gabaergic System and Sleep
nutrients Review Herbal Remedies and Their Possible Effect on the GABAergic System and Sleep Oliviero Bruni 1,* , Luigi Ferini-Strambi 2,3, Elena Giacomoni 4 and Paolo Pellegrino 4 1 Department of Developmental and Social Psychology, Sapienza University, 00185 Rome, Italy 2 Department of Neurology, Ospedale San Raffaele Turro, 20127 Milan, Italy; [email protected] 3 Sleep Disorders Center, Vita-Salute San Raffaele University, 20132 Milan, Italy 4 Department of Medical Affairs, Sanofi Consumer HealthCare, 20158 Milan, Italy; Elena.Giacomoni@sanofi.com (E.G.); Paolo.Pellegrino@sanofi.com (P.P.) * Correspondence: [email protected]; Tel.: +39-33-5607-8964; Fax: +39-06-3377-5941 Abstract: Sleep is an essential component of physical and emotional well-being, and lack, or dis- ruption, of sleep due to insomnia is a highly prevalent problem. The interest in complementary and alternative medicines for treating or preventing insomnia has increased recently. Centuries-old herbal treatments, popular for their safety and effectiveness, include valerian, passionflower, lemon balm, lavender, and Californian poppy. These herbal medicines have been shown to reduce sleep latency and increase subjective and objective measures of sleep quality. Research into their molecular components revealed that their sedative and sleep-promoting properties rely on interactions with various neurotransmitter systems in the brain. Gamma-aminobutyric acid (GABA) is an inhibitory neurotransmitter that plays a major role in controlling different vigilance states. GABA receptors are the targets of many pharmacological treatments for insomnia, such as benzodiazepines. Here, we perform a systematic analysis of studies assessing the mechanisms of action of various herbal medicines on different subtypes of GABA receptors in the context of sleep control.