That These Foreign Amines, Or Their ,3-Hydroxylated Derivatives, May Enter Norepi- Nephrine Storage Sites and Then Be Released7' 8 by Nerve Stimulation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 De Juan Et Al
US 200601 10428A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 de Juan et al. (43) Pub. Date: May 25, 2006 (54) METHODS AND DEVICES FOR THE Publication Classification TREATMENT OF OCULAR CONDITIONS (51) Int. Cl. (76) Inventors: Eugene de Juan, LaCanada, CA (US); A6F 2/00 (2006.01) Signe E. Varner, Los Angeles, CA (52) U.S. Cl. .............................................................. 424/427 (US); Laurie R. Lawin, New Brighton, MN (US) (57) ABSTRACT Correspondence Address: Featured is a method for instilling one or more bioactive SCOTT PRIBNOW agents into ocular tissue within an eye of a patient for the Kagan Binder, PLLC treatment of an ocular condition, the method comprising Suite 200 concurrently using at least two of the following bioactive 221 Main Street North agent delivery methods (A)-(C): Stillwater, MN 55082 (US) (A) implanting a Sustained release delivery device com (21) Appl. No.: 11/175,850 prising one or more bioactive agents in a posterior region of the eye so that it delivers the one or more (22) Filed: Jul. 5, 2005 bioactive agents into the vitreous humor of the eye; (B) instilling (e.g., injecting or implanting) one or more Related U.S. Application Data bioactive agents Subretinally; and (60) Provisional application No. 60/585,236, filed on Jul. (C) instilling (e.g., injecting or delivering by ocular ion 2, 2004. Provisional application No. 60/669,701, filed tophoresis) one or more bioactive agents into the Vit on Apr. 8, 2005. reous humor of the eye. Patent Application Publication May 25, 2006 Sheet 1 of 22 US 2006/0110428A1 R 2 2 C.6 Fig. -

Treatment for Calcium Channel Blocker Poisoning a Systematic Review
Clinical Toxicology ISSN: 1556-3650 (Print) 1556-9519 (Online) Journal homepage: http://www.tandfonline.com/loi/ictx20 Treatment for calcium channel blocker poisoning: A systematic review M. St-Onge, P.-A. Dubé, S. Gosselin, C. Guimont, J. Godwin, P. M. Archambault, J.-M. Chauny, A. J. Frenette, M. Darveau, N. Le sage, J. Poitras, J. Provencher, D. N. Juurlink & R. Blais To cite this article: M. St-Onge, P.-A. Dubé, S. Gosselin, C. Guimont, J. Godwin, P. M. Archambault, J.-M. Chauny, A. J. Frenette, M. Darveau, N. Le sage, J. Poitras, J. Provencher, D. N. Juurlink & R. Blais (2014) Treatment for calcium channel blocker poisoning: A systematic review, Clinical Toxicology, 52:9, 926-944, DOI: 10.3109/15563650.2014.965827 To link to this article: http://dx.doi.org/10.3109/15563650.2014.965827 © 2014 The Author(s). Published by Taylor & View supplementary material Francis. Published online: 06 Oct 2014. Submit your article to this journal Article views: 8320 View related articles View Crossmark data Citing articles: 47 View citing articles Full Terms & Conditions of access and use can be found at http://www.tandfonline.com/action/journalInformation?journalCode=ictx20 Download by: [Bird Lib Ouhsc] Date: 14 November 2017, At: 06:23 Clinical Toxicology (2014), 52, 926–944 Copyright © 2014 Informa Healthcare USA, Inc. ISSN: 1556-3650 print / 1556-9519 online DOI: 10.3109/15563650.2014.965827 REVIEW ARTICLE Treatment for calcium channel blocker poisoning: A systematic review M. ST-ONGE,1,2,3 P.-A. DUBÉ,4,5,6 S. GOSSELIN,7,8,9 C. GUIMONT,10 J. -

Intracavernous Methoxamine in the Treatment of Priapism
International Journal of Impotence Research (1998) 10, 257±259 ß 1998 Stockton Press All rights reserved 0955-9930/98 $12.00 http://www.stockton-press.co.uk/ijir Case Report Intracavernous methoxamine in the treatment of priapism J Jara, I Moncada, G Bueno and C Hernandez Urology Department, Hospital General Universitario, Madrid, Spain Methoxamine is an alpha-adrenergic drug, its unique pharmacokinetics and mechanism of action on alpha-1 receptors lead to consider it, similarly to phenylephrine, as a ®rst-choice drug for treating drug-induced or veno-occlusive priapism. The experience obtained with its use in the management of three cases of priapism lasting over 7 h and one case of sustained rigid erection caused during anesthetic induction are reported. Keywords: methoxamine; priapism; intracavernous drug therapy Introduction adrenergic agents. In a later phase, cell ischemia and ®brosis takes place, making the smooth muscle irresponsive to pharmacologic agents. Since the introduction of intracavernous injections In this present study we report on the ef®cacy and of vasoactive drugs in clinical practice, the inci- safety of methoxamine, a selective alpha-1 adrener- dence of priapism have enormously increased, from gic agent, in the treatment of drug-induced pri- 1 being an occasional ®nding to be the most common apism. cause of priapism, according to Lue.2 The incidence of this untoward effect of intra- cavernous injections depends on the drug used, the dose administered and the underlying etiology of Case reports impotence. In a review of the literature,3 papaverine induced priapism in 9.5% of 2314 patients, the Case 1 combination of papaverine plus phentolamine in 5.3% of 2914 patients and PGE1 only in 2.4% of the A 44 y old male presented to the urology department 1284 patients revised. -

Title 16. Crimes and Offenses Chapter 13. Controlled Substances Article 1
TITLE 16. CRIMES AND OFFENSES CHAPTER 13. CONTROLLED SUBSTANCES ARTICLE 1. GENERAL PROVISIONS § 16-13-1. Drug related objects (a) As used in this Code section, the term: (1) "Controlled substance" shall have the same meaning as defined in Article 2 of this chapter, relating to controlled substances. For the purposes of this Code section, the term "controlled substance" shall include marijuana as defined by paragraph (16) of Code Section 16-13-21. (2) "Dangerous drug" shall have the same meaning as defined in Article 3 of this chapter, relating to dangerous drugs. (3) "Drug related object" means any machine, instrument, tool, equipment, contrivance, or device which an average person would reasonably conclude is intended to be used for one or more of the following purposes: (A) To introduce into the human body any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (B) To enhance the effect on the human body of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (C) To conceal any quantity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; or (D) To test the strength, effectiveness, or purity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state. (4) "Knowingly" means having general knowledge that a machine, instrument, tool, item of equipment, contrivance, or device is a drug related object or having reasonable grounds to believe that any such object is or may, to an average person, appear to be a drug related object. -

(12) United States Patent (10) Patent No.: US 6,264,917 B1 Klaveness Et Al
USOO6264,917B1 (12) United States Patent (10) Patent No.: US 6,264,917 B1 Klaveness et al. (45) Date of Patent: Jul. 24, 2001 (54) TARGETED ULTRASOUND CONTRAST 5,733,572 3/1998 Unger et al.. AGENTS 5,780,010 7/1998 Lanza et al. 5,846,517 12/1998 Unger .................................. 424/9.52 (75) Inventors: Jo Klaveness; Pál Rongved; Dagfinn 5,849,727 12/1998 Porter et al. ......................... 514/156 Lovhaug, all of Oslo (NO) 5,910,300 6/1999 Tournier et al. .................... 424/9.34 FOREIGN PATENT DOCUMENTS (73) Assignee: Nycomed Imaging AS, Oslo (NO) 2 145 SOS 4/1994 (CA). (*) Notice: Subject to any disclaimer, the term of this 19 626 530 1/1998 (DE). patent is extended or adjusted under 35 O 727 225 8/1996 (EP). U.S.C. 154(b) by 0 days. WO91/15244 10/1991 (WO). WO 93/20802 10/1993 (WO). WO 94/07539 4/1994 (WO). (21) Appl. No.: 08/958,993 WO 94/28873 12/1994 (WO). WO 94/28874 12/1994 (WO). (22) Filed: Oct. 28, 1997 WO95/03356 2/1995 (WO). WO95/03357 2/1995 (WO). Related U.S. Application Data WO95/07072 3/1995 (WO). (60) Provisional application No. 60/049.264, filed on Jun. 7, WO95/15118 6/1995 (WO). 1997, provisional application No. 60/049,265, filed on Jun. WO 96/39149 12/1996 (WO). 7, 1997, and provisional application No. 60/049.268, filed WO 96/40277 12/1996 (WO). on Jun. 7, 1997. WO 96/40285 12/1996 (WO). (30) Foreign Application Priority Data WO 96/41647 12/1996 (WO). -

General Agreement on Tariffs Andtrade
RESTRICTED GENERAL AGREEMENT TAR/W/87/Rev.1 16 June 1994 ON TARIFFS AND TRADE Limited Distribution (94-1266) Committee on Tariff Concessions HARMONIZED COMMODITY DESCRIPTION AND CODING SYSTEM (Harmonized System) Classification of INN Substances Revision The following communication has been received from the Nomenclature and Classification Directorate of the Customs Co-operation Council in Brussels. On 25 May 1993, we sent you a list of the INN substances whose classification had been discussed and decided by the Harmonized System Committee. At the time, we informed you that the classification of two substances, clobenoside and meclofenoxate, would be decided later. Furthermore, for some of the chemicals given in that list, one of the contracting parties had entered a reservation and the Harmonized System Committee therefore reconsidered its earlier decision in those cases. I am therefore sending you herewith a revised complete list of the classification decisions of the INN substances. In this revised list, two substances have been added and the classifications of two have been revised as explained below: (a) Addition Classification of clobenoside, (subheading 2940.00) and meclofenoxate (subheading 2922.19). (b) Amendment Etafedrine and moxidentin have now been reclassified in subheadings 2939.40 and 2932.29 respectively. The list of INN substances reproduced hereafter is available only in English. TAR/W/87/Rev. 1 Page 2 Classification of INN Substances Agreed by the Harmonized System Committee in April 1993 Revision Description HS Code -

View PDF Version
Green Chemistry View Article Online PAPER View Journal | View Issue Synthesis of pharmaceutical drugs from cardanol derived from cashew nut shell liquid†‡ Cite this: Green Chem., 2019, 21, 1043 Yiping Shi, Paul C. J. Kamer § and David J. Cole-Hamilton * Cardanol from cashew nut shell liquid extracted from cashew nut shells was successfully converted into various useful pharmaceutical drugs, such as norfenefrine, rac-phenylephrine, etilefrine and fenoprofene. 3-Vinylphenol, the key intermediate for the synthesis of these drugs, was synthesised from cardanol by ethenolysis to 3-non-8-enylphenol followed by isomerising ethenolysis. The metathesis reaction worked very well using DCM, but the greener solvent, 2-methyl tetrahydrofuran, also gave very similar results. Hydroxyamination of 3-vinylphenol with an iron porphyrin catalyst afforded norfenefrine in over 70% yield. Methylation and ethylation of norfenefrine afforded rac-phenylephrine and etilefrine respectively. A sequence of C–O coupling, isomerising metathesis and selective methoxycarbonylation afforded feno- profene in good yield. A comparison of the routes described in this paper with some standard literature Creative Commons Attribution 3.0 Unported Licence. syntheses of 3-vinylphenol and of the drug molecules shows significant environmental advantages in terms of precursors, yields, number of steps, conditions and the use of catalysts. The Atom Economy of our processes is generally similar or significantly superior to those of the literature processes mainly Received 7th December 2018, because the side products produced during synthesis of 3-vinylphenol (1-octeme, 1,4-cyclohexadiene Accepted 15th January 2019 and propene) are easily separable and of commercial value, especially as they are bio-derived. -

Penetrating Topical Pharmaceutical Compositions Containing N-\2-Hydroxyethyl\Pyrrolidone
Europaisches Patentamt ® J European Patent Office © Publication number: 0 129 285 Office europeen des brevets A2 (12) EUROPEAN PATENT APPLICATION © Application number: 84200823.7 ©Int CI.3: A 61 K 47/00 A 61 K 31/57, A 61 K 45/06 © Date of filing: 12.06.84 © Priority: 21.06.83 US 506273 © Applicant: THE PROCTER & GAMBLE COMPANY 301 East Sixth Street Cincinnati Ohio 45201 (US) © Date of publication of application: 27.12.84 Bulletin 84/52 © Inventor: Cooper, Eugene Rex 2425 Ambassador Drive © Designated Contracting States: Cincinnati Ohio 4523KUS) BE CH DE FR GB IT LI NL SE © Representative: Suslic, Lydia et al, Procter & Gamble European Technical Center Temseiaan 100 B-1820 Strombeek-Bever(BE) © Penetrating topical pharmaceutical compositions containing N-(2-hydroxyethyl)pyrrolidone. Topical pharmaceutical compositions comprising a pharmaceutically-active agent and a novel, penetration- enhancing vehicle or carrier are disclosed. The vehicle or carrier comprises a binary combination of N-(2-Hydroxyethyl) pyrrolidone and a "cell-envelope disordering compound". The compositions provide marked transepidermal and per- cutaneous delivery of the active selected. A method of treat- ing certain pathologies and conditions responsive to the selected active, systemically or locally, is also disclosed. TECHNICAL FIELD i The present invention relates to compositions which enhance the utility of certain pharmaceutically-active agents by effectively delivering these agents through the integument. Because of the ease of access, dynamics of application, large surface area, vast exposure to the circulatory and lymphatic networks, and non-invasive nature of the treatment, the delivery of pharmaceutically-active agents through the skin has long been a promising concept. -

NDA 13-400/S-086 Page 3 TABLETS
NDA 13-400/S-086 Page 3 TABLETS ALDOMET® (METHYLDOPA) DESCRIPTION ALDOMET™ (Methyldopa) is an antihypertensive drug. Methyldopa, the L-isomer of alpha-methyldopa, is levo-3-(3,4-dihydroxyphenyl)-2-methylalanine. Its empirical formula is C10H13NO4, with a molecular weight of 211.22, and its structural formula is: Methyldopa is a white to yellowish white, odorless fine powder, and is soluble in water. ALDOMET is supplied as tablets, for oral use, in three strengths: 125 mg, 250 mg, or 500 mg of methyldopa per tablet. Inactive ingredients in the tablets are: calcium disodium edetate, cellulose, citric acid, colloidal silicon dioxide, D&C Yellow 10, ethylcellulose, guar gum, hydroxypropyl methylcellulose, iron oxide, magnesium stearate, propylene glycol, talc, and titanium dioxide. CLINICAL PHARMACOLOGY ALDOMET is an aromatic-amino-acid decarboxylase inhibitor in animals and in man. Although the mechanism of action has yet to be conclusively demonstrated, the antihypertensive effect of methyldopa probably is due to its metabolism to alpha-methylnorepinephrine, which then lowers arterial pressure by stimulation of central inhibitory alpha-adrenergic receptors, false neurotransmission, and/or reduction of plasma renin activity. Methyldopa has been shown to cause a net reduction in the tissue concentration of serotonin, dopamine, norepinephrine, and epinephrine. Only methyldopa, the L-isomer of alpha-methyldopa, has the ability to inhibit dopa decarboxylase and to deplete animal tissues of norepinephrine. In man the antihypertensive activity appears to be due solely to the L-isomer. About twice the dose of the racemate (DL-alpha-methyldopa) is required for equal antihypertensive effect. Methyldopa has no direct effect on cardiac function and usually does not reduce glomerular filtration rate, renal blood flow, or filtration fraction. -
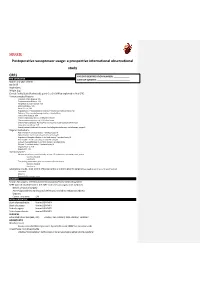
Postoperative Vasopressor Usage: a Prospective International Observational Study
SQUEEZE Postoperative vasopressor usage: a prospective international observational study CRF1 PATIENT IDENTIFICATION NUMBER: _____________ PRE-OPERATIVE DATE OF SURGERY: ___________________________ Month and year of birth Sex [m/f] Height [cm] Weight [kg] Clinical Frailty Scale (Rockwood): point 0 to 9. (Will be explained in final CRF) Previous medical history: Coronary Artery Disease: Y/N Cerebrovascular Disease: Y/N Peripheral vascular disease: Y/N Atrial fibrillation: Y/N Heart failure: Y/N Hypertension: Y treated and controlled, Y treated but not controlled, No Diabetes: Takes insulin/managed without insulin/None Chronic liver disease: Y/N Chronic respiratory disease: COPD/other/None Chronic immunosuppression: HIV/other/none Chronic Kidney Disease: No/Yes/Yes and receives renal replacement therapy Long-term steroid use: Y/N Recent/current treatment for cancer (including chemotherapy, radiotherapy, surgery) Regular medications ACE inhibitor: Y and took today/ Y omitted today/N Alpha blocker: Y and took today/ Y omitted today/N Angiotensin Receptor Blocker: Y and took today/ Y omitted today/N Beta blocker: Y and took today/ Y omitted today/N Calcium channel blocker: Y and took today/ Y omitted today Diuretic: Y and took today/ Y omitted today/N Regular NSAIDs: Y/N Regular PPI: Y/N Haemodynamics Measurement in the past 6 months, at least 12h prior to the operating room, at rest: Systolic, Diastolic Heart rate The reading immediately prior to induction of anaesthesia: Systolic, Diastolic Heart rate Laboratory results, most recent (if known -

Omega Laboratories, Inc. Robert Bard Managing Director 400 N
DEPARTMENT OF HEALTH & HUMAN SERVICES Public Health Service __________________________________________________________________________________________________________________________ Food and Drug Administration 10903 New Hampshire Avenue Document Control Center – WO66-G609 Silver Spring, MD 20993-0002 July 28, 2015 OMEGA LABORATORIES, INC. ROBERT BARD MANAGING DIRECTOR 400 N. CLEVELAND AVE. MOGADORE OH 44260 Re: K142855 Trade/Device Name: Omega Laboratories Hair Drug Screening Assay Methamphetamine (Meth) and 3, 4—Methylenedioxymethamphetamine (MDMA) Regulation Number: 21 CFR 862.3610 Regulation Name: Methamphetamine test system Regulatory Class: II Product Code: DKZ Dated: July 01, 2015 Received: July 13, 2015 Dear Robert Bard: We have reviewed your Section 510(k) premarket notification of intent to market the device referenced above and have determined the device is substantially equivalent (for the indications for use stated in the enclosure) to legally marketed predicate devices marketed in interstate commerce prior to May 28, 1976, the enactment date of the Medical Device Amendments, or to devices that have been reclassified in accordance with the provisions of the Federal Food, Drug, and Cosmetic Act (Act) that do not require approval of a premarket approval application (PMA). You may, therefore, market the device, subject to the general controls provisions of the Act. The general controls provisions of the Act include requirements for annual registration, listing of devices, good manufacturing practice, labeling, and prohibitions against misbranding and adulteration. Please note: CDRH does not evaluate information related to contract liability warranties. We remind you, however, that device labeling must be truthful and not misleading. If your device is classified (see above) into either class II (Special Controls) or class III (PMA), it may be subject to additional controls. -

Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DIX to the HTSUS—Continued
20558 Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DEPARMENT OF THE TREASURY Services, U.S. Customs Service, 1301 TABLE 1.ÐPHARMACEUTICAL APPEN- Constitution Avenue NW, Washington, DIX TO THE HTSUSÐContinued Customs Service D.C. 20229 at (202) 927±1060. CAS No. Pharmaceutical [T.D. 95±33] Dated: April 14, 1995. 52±78±8 ..................... NORETHANDROLONE. A. W. Tennant, 52±86±8 ..................... HALOPERIDOL. Pharmaceutical Tables 1 and 3 of the Director, Office of Laboratories and Scientific 52±88±0 ..................... ATROPINE METHONITRATE. HTSUS 52±90±4 ..................... CYSTEINE. Services. 53±03±2 ..................... PREDNISONE. 53±06±5 ..................... CORTISONE. AGENCY: Customs Service, Department TABLE 1.ÐPHARMACEUTICAL 53±10±1 ..................... HYDROXYDIONE SODIUM SUCCI- of the Treasury. NATE. APPENDIX TO THE HTSUS 53±16±7 ..................... ESTRONE. ACTION: Listing of the products found in 53±18±9 ..................... BIETASERPINE. Table 1 and Table 3 of the CAS No. Pharmaceutical 53±19±0 ..................... MITOTANE. 53±31±6 ..................... MEDIBAZINE. Pharmaceutical Appendix to the N/A ............................. ACTAGARDIN. 53±33±8 ..................... PARAMETHASONE. Harmonized Tariff Schedule of the N/A ............................. ARDACIN. 53±34±9 ..................... FLUPREDNISOLONE. N/A ............................. BICIROMAB. 53±39±4 ..................... OXANDROLONE. United States of America in Chemical N/A ............................. CELUCLORAL. 53±43±0