Factors Affecting Bronchodilator Delivery in Mechanically Ventilated Adults Arzu Ari and James B Fink
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Correlation Between Tidal Volume Measured by Spirometry and Impedance Pneumography
New Jersey Institute of Technology Digital Commons @ NJIT Theses Electronic Theses and Dissertations Fall 10-31-1994 Correlation between tidal volume measured by spirometry and impedance pneumography Krithika Seshadri New Jersey Institute of Technology Follow this and additional works at: https://digitalcommons.njit.edu/theses Part of the Biomedical Engineering and Bioengineering Commons Recommended Citation Seshadri, Krithika, "Correlation between tidal volume measured by spirometry and impedance pneumography" (1994). Theses. 1696. https://digitalcommons.njit.edu/theses/1696 This Thesis is brought to you for free and open access by the Electronic Theses and Dissertations at Digital Commons @ NJIT. It has been accepted for inclusion in Theses by an authorized administrator of Digital Commons @ NJIT. For more information, please contact [email protected]. Copyright Warning & Restrictions The copyright law of the United States (Title 17, United States Code) governs the making of photocopies or other reproductions of copyrighted material. Under certain conditions specified in the law, libraries and archives are authorized to furnish a photocopy or other reproduction. One of these specified conditions is that the photocopy or reproduction is not to be “used for any purpose other than private study, scholarship, or research.” If a, user makes a request for, or later uses, a photocopy or reproduction for purposes in excess of “fair use” that user may be liable for copyright infringement, This institution reserves the right to refuse to -

Pressure-Controlled Ventilation in Children with Severe Status Asthmaticus*
Feature Articles Pressure-controlled ventilation in children with severe status asthmaticus* Ashok P. Sarnaik, MD, FAAP, FCCM; Kshama M. Daphtary, MD; Kathleen L. Meert, MD, FAAP; Mary W. Lieh-Lai, MD, FAAP; Sabrina M. Heidemann, MD, FAAP Objective: The optimum strategy for mechanical ventilation in trolled ventilation, median pH increased to 7.31 (6.98–7.45, p < a child with status asthmaticus is not established. Volume-con- .005), and PCO2 decreased to 41 torr (21–118 torr, p < .005). For trolled ventilation continues to be the traditional approach in such patients with respiratory acidosis (PCO2 >45 torr) within 1 hr of children. Pressure-controlled ventilation may be theoretically starting pressure-controlled ventilation, the median length of time more advantageous in allowing for more uniform ventilation. We until PCO2 decreased to <45 torr was 5 hrs (1–51 hrs). Oxygen describe our experience with pressure-controlled ventilation in saturation was maintained >95% in all patients. Two patients had children with severe respiratory failure from status asthmaticus. pneumomediastinum before pressure-controlled ventilation. One Design: Retrospective review. patient each developed pneumothorax and subcutaneous emphy- Setting: Pediatric intensive care unit in a university-affiliated sema after initiation of pressure-controlled ventilation. All pa- children’s hospital. tients survived without any neurologic morbidity. Median duration Patients: All patients who received mechanical ventilation for of mechanical ventilation was 29 hrs (4–107 hrs), intensive care status asthmaticus. stay was 56 hrs (17–183 hrs), and hospitalization was 5 days Interventions: Pressure-controlled ventilation was used as the (2–20 days). initial ventilatory strategy. The optimum pressure control, rate, Conclusions: Based on this retrospective study, we suggest and inspiratory and expiratory time were determined based on that pressure-controlled ventilation is an effective ventilatory blood gas values, flow waveform, and exhaled tidal volume. -

Lung Volume Kit Be-Lungkit
LUNG VOLUME KIT BE-LUNGKIT Lung Volume is a broad term that actually refers to several different respiratory measurements: Tidal Volume - volume of air that is exhaled when breathing out normally. Expiratory Reserve - volume of air that that can still be exhaled after having breathed out normally. Inspiratory Reserve - additional volume of air that is available for strenuous activity. This is the volume of air that can still enter your lungs after taking a normal breath. Vital Capacity - total useable volume of air. Residual Volume - unusable volume of air. (Residual volume cannot be measured with this kit.) Assembly You can measure the lung volumes of an individual using this kit. To assemble it, please follow these instructions: 1. Insert the mouthpiece halfway through the opening of the volume bag. Secure the mouthpiece with the rubber bands. 2. While sitting, hold the bag on your knee and press a paper towel against it to force the air out of the bag. Start with the sealed end and push the air out toward the mouthpiece. Measure Tidal Volume 1. Wipe the mouthpiece with a cotton ball dipped in alcohol to clean it. 2. Take a normal breath in, hold your nose and take a normal breath out into the lung volume bag mouthpiece. Slide a paper towel along the bag to push all the air to the lower end and measure the volume of air it contains. (The bag has liter and 1/10 liter graduations.) Record this as tidal volume. 3. Remove all the air from the lung volume bag by sliding the paper towel along its length. -

Effects of Intrapulmonary Percussive Ventilation on Airway Mucus Clearance: a Bench Model 11/2/17, 7�22 AM
Effects of intrapulmonary percussive ventilation on airway mucus clearance: A bench model 11/2/17, 7'22 AM World J Crit Care Med. 2017 Aug 4; 6(3): 164–171. PMCID: PMC5547430 Published online 2017 Aug 4. doi: 10.5492/wjccm.v6.i3.164 Effects of intrapulmonary percussive ventilation on airway mucus clearance: A bench model Lorena Fernandez-Restrepo, Lauren Shaffer, Bravein Amalakuhan, Marcos I Restrepo, Jay Peters, and Ruben Restrepo Lorena Fernandez-Restrepo, Lauren Shaffer, Bravein Amalakuhan, Marcos I Restrepo, Jay Peters, Ruben Restrepo, Division of Pediatric Critical Care, Division of Pulmonary and Critical Care, and Department of Respiratory Care, University of Texas Health Science Center and the South Texas Veterans Health Care System, San Antonio, TX 78240, United States Author contributions: All authors contributed equally to the literature search, data collection, study design and analysis, manuscript preparation and final review. Correspondence to: Dr. Bravein Amalakuhan, MD, Division of Pediatric Critical Care, Division of Pulmonary and Critical Care, and Department of Respiratory Care, University of Texas Health Science Center and the South Texas Veterans Health Care System, 7400 Merton Minter Blvd, San Antonio, TX 78240, United States. [email protected] Telephone: +1-210-5675792 Fax: +1-210-9493006 Received 2017 May 7; Revised 2017 Jun 1; Accepted 2017 Jun 30. Copyright ©The Author(s) 2017. Published by Baishideng Publishing Group Inc. All rights reserved. Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. -
Introduction to Airway Clearance Techniques – Brenda
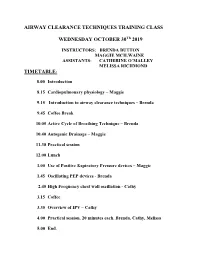
AIRWAY CLEARANCE TECHNIQUES TRAINING CLASS WEDNESDAY OCTOBER 30Th 2019 INSTRUCTORS: BRENDA BUTTON MAGGIE MCILWAINE ASSISTANTS: CATHERINE O’MALLEY MELISSA RICHMOND TIMETABLE: 8.00 Introduction 8.15 Cardiopulmonary physiology – Maggie 9.15 Introduction to airway clearance techniques – Brenda 9.45 Coffee Break 10.05 Active Cycle of Breathing Technique – Brenda 10.40 Autogenic Drainage – Maggie 11.30 Practical session 12.00 Lunch 1.00 Use of Positive Expiratory Pressure devices – Maggie 1.45 Oscillating PEP devices - Brenda 2.45 High Frequency chest wall oscillation - Cathy 3.15 Coffee 3.35 Overview of IPV – Cathy 4.00 Practical session. 20 minutes each. Brenda, Cathy, Melissa 5.00 End. 8/1/2019 Airway Clearance Techniques Training class Dr Maggie McIlwaine and Dr Brenda Button Catherine O’Malley Melissa Richmond Objectives • Explain the physiology, and theory behind airway clearance techniques currently used in the treatment of cystic fibrosis. • Demonstrate the airway clearance techniques of Active cycle of breathing techniques, autogenic drainage, PEP, oscillating PEP, HFCWO and IPV. • Compose the scientific evidence supporting the use of each of these techniques. Timetable • 8.00 Introduction: Maggie • 8.15 Cardiopulmonary physiology – Maggie • 9.15 Introduction to airway clearance and breathing techniques – Brenda • 9.45 Coffee break • 10.05 The Active Cycle of Breathing Techniques - Brenda • 10.40 Autogenic Drainage Maggie • 11.30 Practical session • 12.00 Lunch M. McIlwaine 1 8/1/2019 Timetable • 1.00 Use of Positive Expiratory Pressure Devices – Maggie • 1.45 Oscillating PEP Devices – Brenda • 2.45 C High Frequency Chest wall Oscillation (HFCWO) therapy-Coffee • 3.15 Coffee • 3.35 Overview of IPV – Cathy • 4.00 Practical session. -

Aerosol Bronchodilator Therapy During Noninvasive Positive-Pressure Ventilation: a Peek Through the Looking Glass
Aerosol Bronchodilator Therapy During Noninvasive Positive-Pressure Ventilation: A Peek Through the Looking Glass Exacerbations of chronic obstructive pulmonary disease Variations in the type of aerosol generator employed (COPD) are a common cause of acute respiratory failure,1 (MDI or nebulizer), the position of the aerosol generator, leading to over 700,000 hospitalizations annually in the type of ventilator, inspiratory flow rate, ventilator settings, United States.2 Approximately 50% of patients suffering position of the leak port, circuit conditions, the density of hypercapnic respiratory failure from exacerbations of the inhaled gas, type of mask employed, mask size, amount COPD require some form of ventilatory support.3 The ven- of leak, and patient characteristics are just some of the tilatory strategy employed in such patients has evolved factors that could affect inhaled drug delivery during NPPV. during the past decade, and noninvasive positive-pressure High inspiratory flow rates employed during NPPV in- ventilation (NPPV) is now considered as a first-line mo- crease turbulent flow and produce higher inertial forces, dality of mechanical ventilation for patients with exacer- causing greater impaction of particles in more central air- bations of COPD resulting in hypercapnic respiratory fail- ways.14,15 On the other hand, application of positive pres- ure.4–6 In NPPV, alveolar ventilation is augmented by sure increases tidal volume and reduces the respiratory application of positive pressure through a nasal or oral rate, which are both factors that tend to enhance aerosol mask, thereby avoiding the need for an endotracheal or delivery.16 Moreover, increase in expiratory time could tracheostomy tube. -

Alternative Methods for Assessing Bronchodilator Reversibility In
Thorax 2001;56:713–720 713 Alternative methods for assessing bronchodilator Thorax: first published as 10.1136/thx.56.9.713 on 1 September 2001. Downloaded from reversibility in chronic obstructive pulmonary disease J Hadcroft, P M A Calverley Abstract Chronic obstructive pulmonary disease Background—Bronchodilator reversibil- (COPD) is characterised by airflow limitation ity testing is recommended in all patients which varies little over several months of with chronic obstructive pulmonary dis- observation or after treatment.12 The assess- ease (COPD) but does not predict im- ment of airflow limitation usually relies on provements in breathlessness or exercise spirometric testing and, in particular, the performance. Two alternative ways of forced expiratory volume in 1 second (FEV1) assessing lung mechanics—measurement which is the usual outcome measure in of end expiratory lung volume (EELV) diagnostic bronchodilator reversibility testing.3 using the inspiratory capacity manoeuvre Although useful diagnostically and prognosti- and application of negative expiratory cally,4 spirometric abnormalities are poor pressure (NEP) during tidal breathing to descriptors of the severity of breathlessness in detect tidal airflow limitation—do relate 5 COPD. Likewise, significant changes in FEV1 to the degree of breathlessness in COPD. after inhaled bronchodilators are not necessary Their usefulness as end points in broncho- for improvement in exercise performance or dilator reversibility testing has not been dyspnoea to occur.5–7 Two alternative tech- examined. niques of measuring lung mechanics relatively Methods—We studied 20 patients with easily are now available. Both are better corre- clinically stable COPD (mean age 69.9 lates of breathlessness than FEV , but their (1.5) years, 15 men, forced expiratory vol- 1 reproducibility and sensitivity to change in ume in one second (FEV ) 29.5 (1.6)% pre- 1 response to bronchodilator drugs has not been dicted) with tidal flow limitation as assessed—an important consideration if they assessed by their maximum flow-volume loop. -

Comparison of Tidal Breathing Flow-Volume Loops Generated by a Respiratory Volume Monitor and Spirometry
Comparison of Tidal Breathing Flow-Volume Loops Generated by a Respiratory Volume Monitor and Spirometry Presenting Author: Jenny Freeman, MD, Respiratory Motion Inc. Co-Authors: Wael Saasouh, MD, Detroit Medical Center, Man Ching Cheung, PhD, Jasmin Imsirovic, PhD, Respiratory Motion Inc. Introduction: Flow-volume loops (FVLs) are used to diagnose and monitor the progression and treatment oF lung disorders such as COPD and asthma. The gold standard For generating FVLs is a spirometry-based Forced vital capacity test, which requires the use oF a mouthpiece or FacemasK and patient cooperation to generate maximum eFFort breaths. These tests cannot be perFormed by young children and adults unable to Follow instructions. For these patients, the use oF tidal breathing Flow-volume loops (TBFVLs) has been proposed but has not been widely adopted due to lacK oF a reliable, non-invasive, technological solution. An impedance-based respiratory volume monitor (RVM) non-invasively measures minute ventilation and can be used to generate TBFVLs. The objectives oF this study were: 1) to use a spirometer to evaluate TBFVLs measured by the RVM in healthy volunteers and 2) to monitor TBFVLs in post-operative patients using only the RVM over an extended period oF time. Methods: As part oF an IRB approved study, 20 healthy adult volunteers were simultaneously monitored with a RVM (ExSpiron 1Xi, Respiratory Motion Inc, Waltham, MA) and a pneumotachometer (SpiroAir-LT, Morgan ScientiFic, Haverhill, MA) while breathing at rest for 10 minutes. Another 20 patients recovering From abdominal surgery were monitored with only the RVM For up to 48 hours on a hospital Floor. -

Tidal Volume Settings in Adult Mechanical Ventilation
Setting the Tidal Volume In Adults Receiving Mechanical Ventilation: Lessons Learned From Recent Investigations Todd Bocklage, MPA, RRT Assistant Manager – Respiratory Care Services & Pulmonary Function Lab University of Missouri Health Care University Hospital & Women’s and Children’s Hospital Columbia, Missouri Robert A. Balk, MD J. Bailey Carter, MD Professor of Medicine Director – Division of Pulmonary and Critical Care Medicine Rush Medical College and Rush University Medical Center Chicago, IL Corresponding Author: Robert A. Balk, MD Division of Pulmonary and Critical Care Medicine Rush University Medical Center 1725 W. Harrison, Suite 054 Chicago, IL 60612 T 312-942-2552 F 312-942-8187 Email [email protected] Disclosure: Both authors are members of the National Board of Respiratory Care. Neither author has other real or potential conflicts of interest or other disclosures to declare. Introduction Selecting the optimum tidal volume for adult patients on ventilatory support is critical to achieving the best clinical outcomes. Over the years, guidelines about tidal volumes have varied including times when sigh breaths were set to prevent the development of atelectasis. The purpose of this article is to describe the transition that examination committees have made over the last several years in which lung protection has become the primary goal when making decisions about mechanical ventilation. Ventilator Induced Lung Injury Since the introduction of mechanical ventilatory support over 60 years ago, there has been an increasing body of -

Variability of Tidal Volume in Patient-Triggered Mechanical Ventilation in ARDS
RESPIRATORY CARE Paper in Press. Published on August 1, 2017 as DOI: 10.4187/respcare.05415 Variability of Tidal Volume in Patient-Triggered Mechanical Ventilation in ARDS Sophie Perinel-Ragey MD, Loredana Baboi PhD, and Claude Gue´rin MD PhD BACKGROUND: Limiting tidal volume (VT) in patients with ARDS may not be achieved once patient-triggered breaths occur. Furthermore, ICU ventilators offer numerous patient-triggered modes that work differently across brands. We systematically investigated, using a bench model, the effect of patient-triggered modes on the size and variability of VT at different breathing frequencies (f), patient effort, and ARDS severity. METHODS: We used a V500 Infinity ICU ventilator con- nected to an ASL 5000 lung model whose compliance was mimicking mild, moderate, and severe ARDS. Thirteen patient-triggered modes were tested, falling into 3 categories, namely volume control ventilation with mandatory minute ventilation; pressure control ventilation, including air- way pressure release ventilation (APRV); and pressure support ventilation. Two levels of f and effort were tested for each ARDS severity in each mode. Median (first-third quartiles) VT was compared across modes using non-parametric tests. The probability of VT > 6 mL/kg ideal body weight was assessed by binomial regression and expressed as the odds ratio (OR) with 95% CI. VT variability was measured from the coefficient of variation. RESULTS: VT distribution over all f, effort, and ARDS categories significantly differed across modes (P < .001, Kruskal–Wallis test). VT was significantly greater with pressure support (OR 420 mL, 95% CI 332–527 mL) than with any other mode except for variable pressure support level. -
Ventilator Waveform Analysis
VENTILATOR WAVEFORM ANALYSIS By Dr. M. V. Nagarjuna 1 Seminar Overview 1. Basic Terminology ( Types of variables,,, Breaths, modes of ventilation) 2. Ideal ventilator waveforms (()Scalars) 3. Diagnosing altered physiological states 4. Ventilator Patient Asynchrony and its management. 5. Loops (Pressure volume and Flow volume) 2 Basics phase variables………….. A. Trigger ……. BC What causes the breath to begin? B. Limit …… A What regulates gas flow during the breath? C. Cycle ……. What causes the breath to end? VARIABLES 1. TRIGGER VARIABLE : Initiates the breath Flow (Assist breath) Pressure (Assist Breath) Time (Control Breath) Newer variables (Volume, Shape signal, neural) Flow trigge r better th an Pressure tri gger . With the newer ventilators, difference in work of triggering is of minimal clinical significance. British Journal of Anaesthesia, 2003 4 2. TARGET VARIABLE : Controls the gas delivery during the breath Flow ( Volume Control modes) Pressure ( Pressure Control modes) 3. CYCLE VARIABLE : Cycled from inspiration into expiiiration Volume ( Volume control) Time (Pressure control) Flow (pressure Support) Pressure (Sft(Safety cycling varibl)iable) 5 Modes of Ventilation Mode of ventilation Breath types available Volume Assist Control Volume Control, Volume Assist Pressure Assist Control Pressure Control, Pressure Assist Volume SIMV Volume Control, Volume Assist, Pressure Support Pressure SIMV Pressure Control, Pressure Assist, Pressure Support Pressure Support Pressure support 6 SCALARS 7 FLOW vs TIME 8 Flow versus time Never forget to look at the expiratory limb of the flow waveform The expiratory flow is determined by the elastic recoil of the respiratory system and resistance of intubated airways 9 Types of Inspiratory flow waveforms a. Square wave flow b. -

Bronchodilator Therapy in COPD: Physiological Effects
Breathe review bronch therapy.qxd 21/05/2008 16:19 Page 2 This article has been adapted from an ERS Research Seminar held in Como, Italy in 2007. The original slides and other material can be found at www.ers-education.org D.E. O'Donnell Bronchodilator therapy in Professor of Medicine and Physiology COPD: physiological effects Division of Respiratory and Critical Care Medicine Queen's University Richardson House 102 Stuart Street K7L 2V6 Kingston, ON Canada Fax: 1 6135491459 Email: [email protected] Competing interests The author has served on advisory boards, accepted speaker’s fees and received research funding from GlaxoSmithKline, Pfizer and Boehringer Ingelheim. Provenance Adapted from an ERS Research Seminar Educational aims k To review current concepts of the mechanisms of symptom relief and improved exercise tolerance following pharmacological treatment in chronic obstructive pulmonary disease (COPD). k To examine the relative responsiveness of new physiological outcome parameters in clinical trials. Summary Bronchodilator therapy is the first step in improving dyspnoea and exercise endurance in patients with COPD. Recent studies have challenged the long-held view that airway obstruc- tion in COPD is irreversible. We now know that even in the setting of minor or no change in traditional spirometry, bronchodilator therapy is associated with consistent, and often impressive, reduction in lung hyperinflation. This pharmacological lung volume reduction is linked to improved inspiratory muscle function and enhanced neuro- mechanical coupling of the respiratory system during activity, even in those with advanced disease. Moreover, these improvements in dynamic mechanics provide a sound physiological rationale for observed bronchodilator-induced improvements in the important patient-centred outcomes of reduced dyspnoea and activity limitation.