Autogenic Drainage: the Technique, Physiological Basis and Evidence
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Correlation Between Tidal Volume Measured by Spirometry and Impedance Pneumography
New Jersey Institute of Technology Digital Commons @ NJIT Theses Electronic Theses and Dissertations Fall 10-31-1994 Correlation between tidal volume measured by spirometry and impedance pneumography Krithika Seshadri New Jersey Institute of Technology Follow this and additional works at: https://digitalcommons.njit.edu/theses Part of the Biomedical Engineering and Bioengineering Commons Recommended Citation Seshadri, Krithika, "Correlation between tidal volume measured by spirometry and impedance pneumography" (1994). Theses. 1696. https://digitalcommons.njit.edu/theses/1696 This Thesis is brought to you for free and open access by the Electronic Theses and Dissertations at Digital Commons @ NJIT. It has been accepted for inclusion in Theses by an authorized administrator of Digital Commons @ NJIT. For more information, please contact [email protected]. Copyright Warning & Restrictions The copyright law of the United States (Title 17, United States Code) governs the making of photocopies or other reproductions of copyrighted material. Under certain conditions specified in the law, libraries and archives are authorized to furnish a photocopy or other reproduction. One of these specified conditions is that the photocopy or reproduction is not to be “used for any purpose other than private study, scholarship, or research.” If a, user makes a request for, or later uses, a photocopy or reproduction for purposes in excess of “fair use” that user may be liable for copyright infringement, This institution reserves the right to refuse to -

Lung Abscess: Analysis of 252 Consecutive Cases Diagnosed Between 1968 and 2004
136 Moreira JS, Camargo JJP, Felicetti JC, Goldenfun PR, Moreira ALS, Porto NS Artigo Original Abscesso pulmonar de aspiração: análise de 252 casos consecutivos estudados de 1968 a 2004* Lung abscess: analysis of 252 consecutive cases diagnosed between 1968 and 2004 JOSÉ DA SILVA MOREIRA1, JOSÉ DE JESUS PEIXOTO CAMARGO2, JOSÉ CARLOS FELICETTI2, PAULO ROBERTO GOLDENFUN3, ANA LUIZA SCHNEIDER MOREIRA4, NELSON DA SILVA PORTO2 RESUMO Objetivo: Apresentar a experiência de um serviço especializado em doenças respiratórias no manejo de casos de abscesso pulmonar de aspiração. Métodos: Descrevem-se aspectos diagnósticos e resultados terapêuticos de 252 casos consecutivos de pacientes com abscesso de pulmão, hospitalizados de 1968 a 2004. Resultados: Dos 252 casos, 209 ocorreram em homens e 43 em mulheres, com média de idade de 41,4 anos. Eram alcoolistas 70,2% dos pacientes. Tosse, expectoração, febre e comprometimento do estado geral ocorreram em mais de 97% dos casos, 64% tinham dor torácica, 30,2% hipocratismo digital, 82,5% apresentavam dentes em mau estado de conservação, 78,6% tiveram episódio de perda de consciência e 67,5% apresentavam odor fétido de secreções broncopulmonares. Em 85,3% dos casos as lesões localizavam-se nos segmentos posterior de lobo superior ou superior de lobo inferior, 96,8% delas unilateralmente. Em 24 pacientes houve associação de empiema pleural (9,5%). Flora mista foi identificada em secreções broncopulmonares ou pleurais em 182 pacientes (72,2 %). Todos os doentes foram inicialmente tratados com antibióticos (principalmente penicilina ou clindamicina) e 98,4 % deles foram submetidos à drenagem postural. Procedimentos cirúrgicos foram efetuados em 52 (20,6%) pacientes (24 drenagens de empiema, 22 ressecções pulmonares e 6 pneumostomias). -

Pressure-Controlled Ventilation in Children with Severe Status Asthmaticus*
Feature Articles Pressure-controlled ventilation in children with severe status asthmaticus* Ashok P. Sarnaik, MD, FAAP, FCCM; Kshama M. Daphtary, MD; Kathleen L. Meert, MD, FAAP; Mary W. Lieh-Lai, MD, FAAP; Sabrina M. Heidemann, MD, FAAP Objective: The optimum strategy for mechanical ventilation in trolled ventilation, median pH increased to 7.31 (6.98–7.45, p < a child with status asthmaticus is not established. Volume-con- .005), and PCO2 decreased to 41 torr (21–118 torr, p < .005). For trolled ventilation continues to be the traditional approach in such patients with respiratory acidosis (PCO2 >45 torr) within 1 hr of children. Pressure-controlled ventilation may be theoretically starting pressure-controlled ventilation, the median length of time more advantageous in allowing for more uniform ventilation. We until PCO2 decreased to <45 torr was 5 hrs (1–51 hrs). Oxygen describe our experience with pressure-controlled ventilation in saturation was maintained >95% in all patients. Two patients had children with severe respiratory failure from status asthmaticus. pneumomediastinum before pressure-controlled ventilation. One Design: Retrospective review. patient each developed pneumothorax and subcutaneous emphy- Setting: Pediatric intensive care unit in a university-affiliated sema after initiation of pressure-controlled ventilation. All pa- children’s hospital. tients survived without any neurologic morbidity. Median duration Patients: All patients who received mechanical ventilation for of mechanical ventilation was 29 hrs (4–107 hrs), intensive care status asthmaticus. stay was 56 hrs (17–183 hrs), and hospitalization was 5 days Interventions: Pressure-controlled ventilation was used as the (2–20 days). initial ventilatory strategy. The optimum pressure control, rate, Conclusions: Based on this retrospective study, we suggest and inspiratory and expiratory time were determined based on that pressure-controlled ventilation is an effective ventilatory blood gas values, flow waveform, and exhaled tidal volume. -

Respiratory – Aspiration Precautions SECTION: 9.01 Strength of Evidence Level: 3
Respiratory – Aspiration Precautions SECTION: 9.01 Strength of Evidence Level: 3 PURPOSE: 4. Consult speech therapist for patients with Implement and educate patient/caregiver on precautions dysphagia, as needed, and as ordered by that prevent aspiration. healthcare provider. 5. Consult dietitian for diet evaluation, as needed CONSIDERATIONS: (requires physician’s order). 6. If patient receiving enteral feedings, See Digestive - 1. Precautions should be taken with all patients who Gastrostomy or Jejunostomy Tube Feeding. are unable to protect their airway to prevent the 7. Monitor patient when eating/drinking: involuntary inhalation of foreign substances, such a. Instruct family or caregiver to do the same. as gastric contents, oropharyngeal secretions, b. Observe adequacy of swallowing. food or fluids, into the tracheobronchial passages. c. SN: order ST eval for tube fed patients for 2. Patients at particular risk for aspiration include those swallow eval as appropriate. whose normal protective mechanisms are impaired. 8. Maintain calm environment when the patient is 3. Major risk factors include: eating or drinking. a. Decreased level of consciousness (confusion, 9. If patient is unable to manage own oral secretions, coma, sedation). nasopharyngeal suctioning may be indicated, b. Documented previous episode of aspiration. consult with healthcare provider and refer to c. Neuromuscular disease and structural nasopharyngeal suctioning policy as needed. abnormalities of the aerodigestive tract. 10. Keep wire cutters at HOB of patient with wired jaws d. Depressed protective reflexes (cough or gag). and instruct patient and caregiver in use. e. Presence of an endotracheal tube. 11. Notify healthcare provider immediately for any signs f. Persistently high gastric residual volumes. -

Chest Physiotherapy Page 1 of 10
UTMB RESPIRATORY CARE SERVICES Policy 7.3.9 PROCEDURE - Chest Physiotherapy Page 1 of 10 Chest Physiotherapy Effective: 10/12/94 Revised: 04/05/18 Formulated: 11/78 Chest Physiotherapy Purpose To standardize the use of chest physiotherapy as a form of therapy using one or more techniques to optimize the effects of gravity and external manipulation of the thorax by postural drainage, percussion, vibration and cough. A mechanical percussor may also be used to transmit vibrations to lung tissues. Policy Respiratory Care Services provides skilled practitioners to administer chest physiotherapy to the patient according to physician’s orders. Accountability/Training • Chest Physiotherapy is administered by a Licensed Respiratory Care Practitioner trained in the procedure(s). • Training must be equivalent to the minimal entry level in the Respiratory Care Service with the understanding of age specific requirements of the patient population treated. Physician's A written order by a physician is required specifying: Order Frequency of therapy. Lung, lobes and segments to be drained. Any physical or physiological difficulties in positioning patient. Cough stimulation as necessary. Type of supplemental oxygen, and/or adjunct therapy to be used. Indications This therapy is indicated as an adjunct in any patient whose cough alone (voluntary or induced) cannot provide adequate lung clearance or the mucociliary escalator malfunctions. This is particularly true of patients with voluminous secretions, thick tenacious secretions, and patients with neuro- muscular disorders. Drainage positions should be specific for involved segments unless contraindicated or if modification is necessary. Drainage usually in conjunction with breathing exercises, techniques of percussion, vibration and/or suctioning must have physician's order. -

A Comparison of the Therapeutic Effectiveness
A COMPARISON OF THE THERAPEUTIC EFFECTIVENESS AND ACCEPTANCE OF CONVENTIONAL POSTURAL DRAINAGE AND PERCUSSION, INTRAPULMONARY PERCUSSIVE VENTILATION AND IDGH FREQUENCY CHEST WALL COMPRESSION IN HOSPITALIZED PATIENTS WITH CYSTIC FIBROSIS A Thesis Presented in Partial Fulfillment of the Requirements for the Degree Master of Science in the Graduate School of The Ohio State University By Sarah Meredith Varekojis, B.S. ***** The Ohio State University 1998 Master's Examination Committee: Approved by Mr. F. Herbert Douce, Adviser Dr. Phil Hoberty Adviser Dr. Karen McCoy School of Allied Medical Professions ABSTRACT A significant clinical manifestation of cystic fibrosis is abnormally abundant and viscous bronchial secretions. This leads to obstruction of bronchi in the lungs and predisposes the individual to chronic pulmonary infections. Bronchopulmonary hygiene is an essential part of the care of a patient with cystic fibrosis in order to enhance mucociliary clearance. Currently, several modalities of therapy are available, including high frequency chest wall compressions (HFCC), intrapulmonary percussive ventilation (IPV) and conventional postural drainage and percussion (PD&P). This study was designed to directly compare the sputum produced with HFCC, IPV and PD&P. Twenty-seven hospitalized patients were recruited for the study. Each patient received two consecutive days of each form of therapy in random order. All therapies were delivered three times a day for thirty minutes. Any sputum produced during the treatment time was expectorated and collected. Sputum was collected for a total of sixty minutes: fifteen minutes before the treatment during aerosol delivery, during the thirty minute treatment and for fifteen minutes post therapy. Sputum expectorated during each session was weighed wet and then dried and weighed again. -

Lung Volume Kit Be-Lungkit
LUNG VOLUME KIT BE-LUNGKIT Lung Volume is a broad term that actually refers to several different respiratory measurements: Tidal Volume - volume of air that is exhaled when breathing out normally. Expiratory Reserve - volume of air that that can still be exhaled after having breathed out normally. Inspiratory Reserve - additional volume of air that is available for strenuous activity. This is the volume of air that can still enter your lungs after taking a normal breath. Vital Capacity - total useable volume of air. Residual Volume - unusable volume of air. (Residual volume cannot be measured with this kit.) Assembly You can measure the lung volumes of an individual using this kit. To assemble it, please follow these instructions: 1. Insert the mouthpiece halfway through the opening of the volume bag. Secure the mouthpiece with the rubber bands. 2. While sitting, hold the bag on your knee and press a paper towel against it to force the air out of the bag. Start with the sealed end and push the air out toward the mouthpiece. Measure Tidal Volume 1. Wipe the mouthpiece with a cotton ball dipped in alcohol to clean it. 2. Take a normal breath in, hold your nose and take a normal breath out into the lung volume bag mouthpiece. Slide a paper towel along the bag to push all the air to the lower end and measure the volume of air it contains. (The bag has liter and 1/10 liter graduations.) Record this as tidal volume. 3. Remove all the air from the lung volume bag by sliding the paper towel along its length. -

Effects of Intrapulmonary Percussive Ventilation on Airway Mucus Clearance: a Bench Model 11/2/17, 7�22 AM
Effects of intrapulmonary percussive ventilation on airway mucus clearance: A bench model 11/2/17, 7'22 AM World J Crit Care Med. 2017 Aug 4; 6(3): 164–171. PMCID: PMC5547430 Published online 2017 Aug 4. doi: 10.5492/wjccm.v6.i3.164 Effects of intrapulmonary percussive ventilation on airway mucus clearance: A bench model Lorena Fernandez-Restrepo, Lauren Shaffer, Bravein Amalakuhan, Marcos I Restrepo, Jay Peters, and Ruben Restrepo Lorena Fernandez-Restrepo, Lauren Shaffer, Bravein Amalakuhan, Marcos I Restrepo, Jay Peters, Ruben Restrepo, Division of Pediatric Critical Care, Division of Pulmonary and Critical Care, and Department of Respiratory Care, University of Texas Health Science Center and the South Texas Veterans Health Care System, San Antonio, TX 78240, United States Author contributions: All authors contributed equally to the literature search, data collection, study design and analysis, manuscript preparation and final review. Correspondence to: Dr. Bravein Amalakuhan, MD, Division of Pediatric Critical Care, Division of Pulmonary and Critical Care, and Department of Respiratory Care, University of Texas Health Science Center and the South Texas Veterans Health Care System, 7400 Merton Minter Blvd, San Antonio, TX 78240, United States. [email protected] Telephone: +1-210-5675792 Fax: +1-210-9493006 Received 2017 May 7; Revised 2017 Jun 1; Accepted 2017 Jun 30. Copyright ©The Author(s) 2017. Published by Baishideng Publishing Group Inc. All rights reserved. Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. -

Postural Drainage Fact Sheet 7-28-05
Consumer Fact Sheet An Introduction to Postural Drainage & Percussion Postural Drainage and Percussion (PD & P), also known why PD & P treatments are effective, and how each lung as chest physical therapy, is a widely accepted technique segment is drained. to help people with cystic fibrosis (CF) breathe with less Draining the Lung Segments difficulty and stay healthy. PD & P uses gravity and per- cussion to loosen the thick, sticky mucus in the lungs so it The goal of PD & P is to clear mucus from each of the five can be removed by coughing. Unclogging the airways is lobes of the lungs by draining mucus into the larger air- critical to reducing the severity of lung infections. ways so that it can be coughed out. The right lung is composed of three lobes: the upper lobe, the middle lobe PD & P is easy to perform using the techniques you will and the lower lobe. The left lung is made up of only two learn here. For the child with CF, PD & P can be lobes: the upper lobe and the lower lobe. performed by physical therapists, respiratory therapists, nurses, parents, siblings and even friends. The lobes are divided into smaller divisions called seg- ments. The upper lobes on the left and right sides are PD & P is sometimes used along with other types of treat- each made up of three segments: apical, posterior and ments, such as inhaled bronchodilators and antibiotics. If anterior. The left upper lobe includes the lingual, which ordered, bronchodilators should be taken before PD & P corresponds to the middle lobe on the right. -
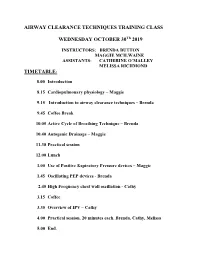
Introduction to Airway Clearance Techniques – Brenda
AIRWAY CLEARANCE TECHNIQUES TRAINING CLASS WEDNESDAY OCTOBER 30Th 2019 INSTRUCTORS: BRENDA BUTTON MAGGIE MCILWAINE ASSISTANTS: CATHERINE O’MALLEY MELISSA RICHMOND TIMETABLE: 8.00 Introduction 8.15 Cardiopulmonary physiology – Maggie 9.15 Introduction to airway clearance techniques – Brenda 9.45 Coffee Break 10.05 Active Cycle of Breathing Technique – Brenda 10.40 Autogenic Drainage – Maggie 11.30 Practical session 12.00 Lunch 1.00 Use of Positive Expiratory Pressure devices – Maggie 1.45 Oscillating PEP devices - Brenda 2.45 High Frequency chest wall oscillation - Cathy 3.15 Coffee 3.35 Overview of IPV – Cathy 4.00 Practical session. 20 minutes each. Brenda, Cathy, Melissa 5.00 End. 8/1/2019 Airway Clearance Techniques Training class Dr Maggie McIlwaine and Dr Brenda Button Catherine O’Malley Melissa Richmond Objectives • Explain the physiology, and theory behind airway clearance techniques currently used in the treatment of cystic fibrosis. • Demonstrate the airway clearance techniques of Active cycle of breathing techniques, autogenic drainage, PEP, oscillating PEP, HFCWO and IPV. • Compose the scientific evidence supporting the use of each of these techniques. Timetable • 8.00 Introduction: Maggie • 8.15 Cardiopulmonary physiology – Maggie • 9.15 Introduction to airway clearance and breathing techniques – Brenda • 9.45 Coffee break • 10.05 The Active Cycle of Breathing Techniques - Brenda • 10.40 Autogenic Drainage Maggie • 11.30 Practical session • 12.00 Lunch M. McIlwaine 1 8/1/2019 Timetable • 1.00 Use of Positive Expiratory Pressure Devices – Maggie • 1.45 Oscillating PEP Devices – Brenda • 2.45 C High Frequency Chest wall Oscillation (HFCWO) therapy-Coffee • 3.15 Coffee • 3.35 Overview of IPV – Cathy • 4.00 Practical session. -

1St Quarter 2002 Medicare a Bulletin
In This Issue... ICD-9-CM Coding for Diagnostic Tests Clarification and examples on reporting the appropriate code for these Services .... 5 New Medicare Enrollment Application New Provider Enrollment Application version CMS 855 has been implemented .... 10 Coverage of Sacral Nerve Stimulation Coverage and Billing Guidelines .............................................................................. 12 Inpatient Rehabilitation Facilities Guidelines for the Implementation of Prospective Payment System ......................... 18 End Stage Renal Disease Blood Pricing for 2002.............................................................................................. 23 Final Medical Review Policies 10060, 11600, 29540, 33282, 76075, 78460, 80061, 80162, 82270, 93224, 93350, 94010, 94240, 95115, J0150, J7190, and J9999 ................................................... 25 Respiratory Services under SNF PPS Bulletin Issues Concerning Billing for Respiratory Therapy ................................................. 81 Outpatient Prospective Payment System Clarification of Activity Therapy and Patient Education/Training Services ............ 88 Features he Medicare A Bulletin From the Medical Director 3 Tshould be shared with all Administrative 4 health care practitioners and managerial members of the General Information 5 provider/supplier staff. General Coverage 11 Publications issued after Fraud and Abuse 16 October 1, 1997, are available at no-cost from our provider Hospital Services 17 Web site at End Stage Renal Disease 23 www.floridamedicare.com. -

Posture in Thoracic Surgery by A
Thorax: first published as 10.1136/thx.3.3.161 on 1 September 1948. Downloaded from Thorax (1948), 3, 161. POSTURE IN THORACIC SURGERY BY A. I. PARRY BROWN From the Thoracic Surgical Unit, Harefield, Middlesex It is important in thoracic surgery to find a pneumonectomy is turned from the lateral to the position upon the operating table which will com- supine position at the end of the operation the bine good surgical access with the minimum pleural pressure on the operation side is also in- interference with respiration. Present practice creased, so that in a well-grown adult it may be favours a postero-lateral approach for most thora- necessary to aspirate 600 to 800 c.cm. of air in cotomies, and for this the patient is placed with the order to produce normal readings and to centralize gobod side of the chest under. The lateral position the mediastinum. These conditions show an is maintained by a pad against the front of the increase in the capacity of the upper hemithorax chest and by pelvic and buttock supports which at the expense of the lower in the lateral position. prevent rolling or slipping if the table is tilted. A Penman (1941), in an investigation of cases who padded wedge or pillow is sometimes placed under had " mediastinal flap," and who were treated by the thorax so as to bow the chest, opening the rib artificial pneumothorax, found the same thing, and spaces on the upper side and so facilitating the in treating mediastinal displacement he used low exposure. Sellors' " chest-rest" combines the pressures and nursed the patients as far as possible wedge and the anterior support in one piece.