Page Mackup-Final.Qxd
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

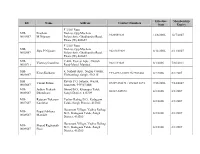
District Taluka Center Name Contact Person Address Phone No Mobile No
District Taluka Center Name Contact Person Address Phone No Mobile No Mhosba Gate , Karjat Tal Karjat Dist AHMEDNAGAR KARJAT Vijay Computer Education Satish Sapkal 9421557122 9421557122 Ahmednagar 7285, URBAN BANK ROAD, AHMEDNAGAR NAGAR Anukul Computers Sunita Londhe 0241-2341070 9970415929 AHMEDNAGAR 414 001. Satyam Computer Behind Idea Offcie Miri AHMEDNAGAR SHEVGAON Satyam Computers Sandeep Jadhav 9881081075 9270967055 Road (College Road) Shevgaon Behind Khedkar Hospital, Pathardi AHMEDNAGAR PATHARDI Dot com computers Kishor Karad 02428-221101 9850351356 Pincode 414102 Gayatri computer OPP.SBI ,PARNER-SUPA ROAD,AT/POST- 02488-221177 AHMEDNAGAR PARNER Indrajit Deshmukh 9404042045 institute PARNER,TAL-PARNER, DIST-AHMEDNAGR /221277/9922007702 Shop no.8, Orange corner, college road AHMEDNAGAR SANGAMNER Dhananjay computer Swapnil Waghchaure Sangamner, Dist- 02425-220704 9850528920 Ahmednagar. Pin- 422605 Near S.T. Stand,4,First Floor Nagarpalika Shopping Center,New Nagar Road, 02425-226981/82 AHMEDNAGAR SANGAMNER Shubham Computers Yogesh Bhagwat 9822069547 Sangamner, Tal. Sangamner, Dist /7588025925 Ahmednagar Opposite OLD Nagarpalika AHMEDNAGAR KOPARGAON Cybernet Systems Shrikant Joshi 02423-222366 / 223566 9763715766 Building,Kopargaon – 423601 Near Bus Stand, Behind Hotel Prashant, AHMEDNAGAR AKOLE Media Infotech Sudhir Fargade 02424-222200 7387112323 Akole, Tal Akole Dist Ahmadnagar K V Road ,Near Anupam photo studio W 02422-226933 / AHMEDNAGAR SHRIRAMPUR Manik Computers Sachin SONI 9763715750 NO 6 ,Shrirampur 9850031828 HI-TECH Computer -
0001S07 Prashant M.Nijasure F 3/302 Rutu Enclave,Opp.Muchal
Effective Membership ID Name Address Contact Numbers from Expiry F 3/302 Rutu MH- Prashant Enclave,Opp.Muchala 9320089329 12/8/2006 12/7/2007 0001S07 M.Nijasure Polytechnic, Ghodbunder Road, Thane (W) 400607 F 3/302 Rutu MH- Enclave,Opp.Muchala Jilpa P.Nijasure 98210 89329 8/12/2006 8/11/2007 0002S07 Polytechnic, Ghodbunder Road, Thane (W) 400607 MH- C-406, Everest Apts., Church Vianney Castelino 9821133029 8/1/2006 7/30/2011 0003C11 Road-Marol, Mumbai MH- 6, Nishant Apts., Nagraj Colony, Kiran Kulkarni +91-0233-2302125/2303460 8/2/2006 8/1/2007 0004S07 Vishrambag, Sangli, 416415 MH- Ravala P.O. Satnoor, Warud, Vasant Futane 07229 238171 / 072143 2871 7/15/2006 7/14/2007 0005S07 Amravati, 444907 MH MH- Jadhav Prakash Bhood B.O., Khanapur Taluk, 02347-249672 8/2/2006 8/1/2007 0006S07 Dhondiram Sangli District, 415309 MH- Rajaram Tukaram Vadiye Raibag B.O., Kadegaon 8/2/2006 8/1/2007 0007S07 Kumbhar Taluk, Sangli District, 415305 Hanamant Village, Vadiye Raibag MH- Popat Subhana B.O., Kadegaon Taluk, Sangli 8/2/2006 8/1/2007 0008S07 Mandale District, 415305 Hanumant Village, Vadiye Raibag MH- Sharad Raghunath B.O., Kadegaon Taluk, Sangli 8/2/2006 8/1/2007 0009S07 Pisal District, 415305 MH- Omkar Mukund Devrashtra S.O., Palus Taluk, 8/2/2006 8/1/2007 0010S07 Vartak Sangli District, 415303 MH MH- Suhas Prabhakar Audumbar B.O., Tasgaon Taluk, 02346-230908, 09960195262 12/11/2007 12/9/2008 0011S07 Patil Sangli District 416303 MH- Vinod Vidyadhar Devrashtra S.O., Palus Taluk, 8/2/2006 8/1/2007 0012S07 Gowande Sangli District, 415303 MH MH- Shishir Madhav Devrashtra S.O., Palus Taluk, 8/2/2006 8/1/2007 0013S07 Govande Sangli District, 415303 MH Patel Pad, Dahanu Road S.O., MH- Mohammed Shahid Dahanu Taluk, Thane District, 11/24/2005 11/23/2006 0014S07 401602 3/4, 1st floor, Sarda Circle, MH- Yash W. -

Village Map Taluka: Karmala District: Solapur
Shrigonda Village Map Jamkhed Taluka: Karmala District: Solapur !( Khadaki Padali Punwar Jategaon Aljapur Karjat Taratgaon Kamone Limbewadi Wadgaon (N) Bitargaon (Shrigonde) µ Ghargaon Balewadi 4.5 2.25 0 4.5 9 13.5 Mangi Ravgaon Potegaon km Wadgaon Kh. Pothare Nilaj Paranda Borgaon Vanjarwadi BhoseHiwarwadi Wadachiwadi Dilmeshwar Gorewadi Karmala (Rural)DhaykhindiKhambewadi Location Index Pimpalwadi KARMALA Morwad Hulgewadi Roshewadi !( Devichamal Karmala (M Cl) Karanje District Index Korti Bhalewadi Nandurbar Veet Pande Mirghavan Bhandara Dhule Amravati Nagpur Gondiya Savadi Vihal Jalgaon Gharatwadi Deolali Akola Wardha Arjunnagar Buldana Kumbhargaon Kuskarwadi Nashik Washim Chandrapur Yavatmal Pondhvadi Hivare Kolgaon Palghar Aurangabad Anjandoh Jalna Hingoli Gadchiroli Kawalwadi Gulsadi Thane Ahmednagar Parbhani Bhilarwadi Hisare Mumbai Suburban Nanded Daund Shelgaon (K) Nimgaon (H) Bid Delwadi Khadakewadi Mumbai Divegavan Rajuri Phisare Pune Zare Raigarh Bidar Ramwadi Manjargaon Latur Gaundare Osmanabad Umrad Domgaon Sarapdoh Sounde Bhagatwadi Hingani Satara Solapur Jinnti Ritewadi Ratnagiri Parewadi Kumbhej Salse Awati Sangli Undargaon Gulmarwadi Maharashtra State Pophalaj Kolhapur Katraj Sade Kondhar Chincholi Sindhudurg Washibe Warkatne Jehurwadi Kondhej Dharwad Pomalwadi Sogaon Kedgaon Alsunde Khatgaon Ketur Nerle Takali (Rashin) Shetphal Jeur Goyegaon Taluka Index Lavhe Warkute Ghoti Nimbhore Karmala Dahigaon Chikhalthan Shelgaon (Wangi) Barshi Kugaon Pathurdi Madha Wangi Bhalavni Malwadi Wangi Malshiras Mohol Pangare Wangi -
Karmala an Open Defecation Free City in Maharashtra Declared on 2Nd October 2015
Swachha Maharashtra Mission (Urban) Karmala An Open Defecation Free City in Maharashtra Declared on 2nd October 2015 Journey of a town towards becoming ODF Urban Development Department Government of Maharashtra Contents 1 City Profile ................................................................................................................................ 1 2 Sanitation Scenario in Karmala prior to the launch of mission .............................................. 1 3 Targets set by the council under SMMU ................................................................................. 1 3.1 Making city open defecation free by bringing a behavioural change in citizens: .......... 1 4 Initiatives by the council .......................................................................................................... 1 4.1 Regular Repair and Maintenance of the Community Toilets ........................................ 2 4.2 Awareness Generation campaigns to encourage use of toilets ...................................... 2 4.3 Sensitization of public ..................................................................................................... 3 4.4 Involvement of citizens ................................................................................................... 4 4.5 Monitoring of likely Open Defecation (OD) spots to prevent OD ................................ 4 4.6 Encourage construction and use of individual toilets .................................................... 4 4.7 Faecal sludge management............................................................................................. -

THE MAHARASHTRA STATE CO-OPERATIVE BANK LTD., MUMBAI (Incorporating the Vidarbha Co-Op Bank Ltd.,)
THE MAHARASHTRA STATE CO-OPERATIVE BANK LTD., MUMBAI (Incorporating The Vidarbha Co-op Bank Ltd.,) Head Office - Sir Vithhaldas Thackersey Memorial Building, 9, Maharashtra Chamber of Commerce Lane, Fort, Mumbai - 400 001 Post Box No. 472 Tel Nos. 91-022-22800747/22876020 Regional Office: - 915/2, Dr Sule Marg, Shivajinagar, P.B. No. 882, Pune-411004 Tel No. (020-25676305/25651021/25654945/25654497/9011741023) Website: https://mscbank.com Reference No. MSCB/RO PUNE/2021-22 Dated:16.06.2021 TENDER FORM FOR SALE OF PLEDGED SUGAR STOCK of Shri Makai SSK Ltd., Bhilarwadi, Tal Karmala, Dist Solapur, The Maharashtra State Co-Operative Bank Ltd., Regional office, Pune hereby invites Bids/Offers in sealed envelopes for sale of the Pledged Sugar stock as per Sub-section (11) of Section 13 of the SECURITISATION AND RECONSTRUCTION OF FINANCIAL ASSETS AND ENFORCEMENT OF SECURITY INTEREST ACT, 2002 (SARFAESI Act, 2002) E:\Proforma Re Tender Sale - Makai SSK Ltd.doc THE MAHARASHTRA STATE CO-OPERATIVE BANK LTD., MUMBAI (Incorporating The Vidarbha Co-Op Bank Ltd.) (Scheduled Bank) Head Office: 9, Maharashtra Chamber of Commerce Lane, Fort, Mumbai – 400 001, Post Box No. 472 Tel Nos. 91-022-22800747/22876020. Website: https://mscbank.com Regional Office: - 915/2, Dr Sule Marg, Shivajinagar, P.B. No. 882, Pune-411004 Tel No. (020-25676305/25651021/25654945/25654497/9011741023) TENDER NOTICE FOR SALE OF PLEDGED SUGAR STOCK The Maharashtra State Co-Operative Bank Ltd., Regional office, Pune hereby invites Bids/Offers in sealed envelopes for sale of the following Pledged Sugar stock of Shri Makai SSK Ltd., Bhilarwadi, Tal Karmala, Dist Solapur, as per Sub-section (11) of Section 13 of the SECURITISATION AND RECONSTRUCTION OF FINANCIAL ASSETS AND ENFORCEMENT OF SECURITY INTEREST ACT, 2002 (SARFAESI Act, 2002) Brief Description of the pledged sugar as per RG 1 Register:- Name of the Particulars of sugar Reserve Price EMD Inspection Tender Opening M.S.C.Bank Unit (In Rs) Date/ Time, date & Outstanding Time place as on 23.05.2021 1 2 3 4 5 6 7 Shri Makai Produced Grade Qnty. -

Panchayat Samiti Elections in Maharashtra: a Data Analysis (1994-2013)
PANCHAYAT SAMITI ELECTIONS IN MAHARASHTRA: A DATA ANALYSIS (1994-2013) Rajas K. Parchure ManasiV. Phadke Dnyandev C. Talule GOKHALE INSTITUTE OF POLITICS AND ECONOMICS (Deemed to be a University)` Pune (India), 411 001 STUDY TEAM Rajas K. Parchure : Team Leader Manasi V. Phadke : Project Co-ordinator Dnyandev C. Talule Project Co-ordinator Rajesh R. Bhatikar : Editorial Desk Anjali Phadke : Statistical Assistant Ashwini Velankar : Research Assistant Vaishnavi Dande Research Assistant Vilas M. Mankar : Technical Assistance PANCHAYAT SAMITI ELECTIONS IN MAHARASHTRA : A DATA ANALYSIS (1994-2013) 2016 TABLE OF CONTENTS CHAPTER CONTENT PAGE NO. NO. Foreword v Acknowledgements vi 1 A Historical Perspective on Local Governance 1 2 Defining Variables and Research Questions 18 3 Data Analysis: Behaviour of Main Variables 25 Across Different Rounds of Elections 4 Data Analysis: Correlations Between Key 85 Variables 5 Conclusion 86 References Appendix – A Data on VT, POL, SCST and REVERSE COMP 89 Across Rounds of Elections Appendix – B Average Values of VT, POL, RESERVE COMP 105 and IND Appendix – C Cluster Analysis of VT, POL, REVERSE COMP, 124 IND and RES Appendix – D Councils Relevant for Immediate Launch of Voter 144 Awareness Programs Appendix – E Councils Relevant for MCC Implementation 146 Gokhale Institute of Politics and Economics, Pune i PANCHAYAT SAMITI ELECTIONS IN MAHARASHTRA : A DATA ANALYSIS (1994-2013) 2016 LIST OF TABLES Tables Content Page No. No. 3.1 Trends in VT across Successive Rounds of Elections 25 3.2 Panchayat Samitis belonging -
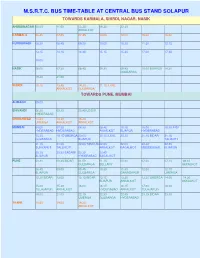
M.S.R.T.C. Bus Time-Table at Central Bus Stand Solapur
M.S.R.T.C. BUS TIME-TABLE AT CENTRAL BUS STAND SOLAPUR TOWARDS KARMALA, SHIRDI, NAGAR, NASIK AHMEDNAGAR 08.00 11.00 13.25 16.30 22.30 AKKALKOT KARMALA 06.45 07.00 07.45 10.00 12.00 15.30 16.00 KURDUWADI 08.30 08.45 09.20 10.00 10.30 11.30 12.15 13.15 14.15 14.45 15.15 15.30 17.00 17.45 18.00 NASIK 06.00 07.30 08.45 09.30 09.45 10.00 BIJAPUR 14.30 GULBARGA 19.30 21.00 SHIRDI 10.15 13.45 14.30 21.15 ILKAL AKKALKOT GULBARGA TOWARDS PUNE, MUMBAI ALIBAGH 09.00 BHIVANDI 06.30 09.30 20.45 UDGIR HYDERABAD CHINCHWAD 13.30 14.30 15.30 UMERGA AKKALKOT AKKALKOT MUMBAI 04.00 07.30 08.30 08.45 10.15 15.00 15.30 INDI HYDERABAD HYDERABAD AKKALKOT BIJAPUR HYDERABAD 15.30 19.15 UMERGA 20.00 20.15 ILKAL 20.30 21.15 BIDAR 21.15 GULBARGA BIJAPUR TALIKOTI 21.15 21.30 22.00 TANDUR 22.00 22.00 22.30 22.45 SURYAPET TALLIKOTI AKKALKOT BAGALKOT MUDDEBIHAL BIJAPUR 23.15 23.30 BADAMI 23.30 23.45 BIJAPUR HYDERABAD BAGALKOT PUNE 00.30 00.45 BIDAR 01.00 01.15 05.30 07.00 07.15 08.15 GULBARGA BELLARY AKKALKOT 08.45 09.00 09.45 10.30 11.30 12.00 12.15 BIJAPUR GULBARGA GANAGAPUR UMERGA 12.30 BIDAR 13.00 13.15 BIDAR 13.15 13.30 13.30 UMERGA 14.00 14.30 BIJAPUR AKKALKOT AKKALKOT 15.00 15.30 16.00 16.15 16.15 17.00 18.00 TULAJAPUR AKKALKOT HYDERABAD AKKALKOT TULAJAPUR 19.00 21.00 22.15 22.30 22.45 23.15 BIDAR 23.30 UMERGA GULBARGA HYDERABAD THANE 10.45 19.00 19.30 AKKALKOT TOWARDS AKKALKOT, GANAGAPUR, GULBARGA AKKALKOT 04.15 05.45 06.00 08.15 09.15 09.15 10.30 10.45 11.00 11.30 11.45 12.15 13.45 14.15 15.30 16.00 16.30 16.45 17.00 GULBARGA 02.00 PUNE 05.15 06.15 07.30 08.15 -
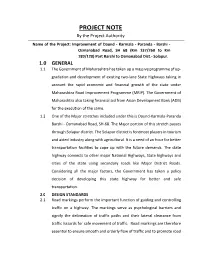
PROJECT NOTE by the Project Authority
PROJECT NOTE By the Project Authority Name of the Project: Improvement of Daund - Karmala - Paranda - Barshi - Osmanabad Road, SH 68 (Km 137/260 to Km 189/120) Part Barshi to Osmanabad Dist.- Solapur. 1.0 GENERAL 1.1 The Government of Maharashtra has taken up a massive programme of up- gradation and development of existing two-lane State Highways taking in account the rapid economic and financial growth of the state under Maharashtra Road Improvement Programme (MRIP). The Government of Maharashtra also taking financial aid from Asian Development Bank (ADB) for the execution of the same. 1.2 One of the Major stretches included under this is Daund-Karmala-Paranda Barshi - Osmanabad Road, SH-68. The Major portion of this stretch passes through Solapur district. The Solapur district is foremost players in tourism and aided industry along with agricultural. It is a need of an hour for better transportation facilities to cope up with the future demands. The state highway connects to other major National Highways, State highways and cities of the state using secondary roads like Major District Roads. Considering all the major factors, the Government has taken a policy decision of developing this state highway for better and safe transportation. 2.0 DESIGN STANDARDS 2.1 Road markings perform the important function of guiding and controlling traffic on a highway. The markings serve as psychological barriers and signify the delineation of traffic paths and their lateral clearance from traffic hazards for safe movement of traffic. Road markings are therefore essential to ensure smooth and orderly flow of traffic and to promote road safety. -

Review of Research Journal:International Monthly Scholarly
ISSN 2249-894X Impact Factor : 3.1402 (UIF) Volume - 5 | Issue - 3 | Dec - 2015 Review Of Research _________________________________________________________________________________ SOCIAL AUDIT OF NATIONAL RURAL EMPLOYMENT GUARANTEE SCHEME IN SOLAPUR DISTRICT Dr. S. V. Shinde Associate Professor , D. A. V. Velankar College of Commerce, Solapur. ABSTRACT : INTRODUCTION : National Rural Employment Guarantee Act 2005 (or, NREGA The act was first No 42, later renamed as the "Mahatma Gandhi National Rural proposed in 1991 by Narasimha Employment Guarantee Act", MGNREGA), is an Indian labour law Rao. In 2006, it was finally and social security measure that aims to guarantee the 'right to work'. accepted in the parliament and It aims to enhance livelihood security in rural areas by commenced implementation in providing at least 100 days of wage employment in a financial year to 200 districts of India. Based on every household whose adult members volunteer to do unskilled this pilot experience, NREGA manual work. was scoped up to covered all the districts of India from 1 April 2008. The MGNREGA was initiated with the objective of "enhancing livelihood security inrural areas by providing at least 100 days of guaranteed wage employment in a financial year, to every household whose adult members volunteer to do unskilled manual work". Another aim of MGNREGA is to create durable assets (such as roads, canals, ponds, wells). Employment is to be provided within 5 km of an applicant's residence, and minimum wages are to be paid. If work is not provided within 15 days of applying, applicants are entitled to an unemployment allowance. Thus, employment under MGNREGA is a legal entitlement. -

Solapur District Maharashtra
1805/DBR/2013 भारत सरकार जल संसाधन मंत्रालय कᴂ द्रीय भुममजल बो셍ड GOVERNMENT OF INDIA MINISTRY OF WATER RESOURCES CENTRAL GROUND WATER BOARD महाराष्ट्र रा煍य के अंतर्डत सोलापुर जजले की भूजल विज्ञान जानकारी GROUND WATER INFORMATION SOLAPUR DISTRICT MAHARASHTRA By 饍वारा Dr. AGS REDDY 셍ा. ए.जी. एस. रे蕍셍ी Scientist-D िैज्ञाननक - घ म鵍य क्षेत्र, नार्पुर CENTRAL REGION, NAGPUR 2013 SOLAPUR DISTRICT AT A GLANCE 1. GENERAL INFORMATION Geographical Area : 14895 sq. km. Administrative Divisions : Taluka-11; N. Solapur, S. Solapur, Barshi, Akkalkot, Pandharpur, Malshiras, Sangola, Mangal Wedha, Madha, Moho, Karmala. Villages : 1158 Population (2001 Census) : 43,15,527 Normal Annual Rainfall 524 mm to 707 mm 2. GEOMORPHOLOGY Major Physiographic unit : Four; Valleys, Denudational Hills (Sahaydri), Highly Dissected Basaltic Plateau, Moderately Dissected Basaltic Plateau, and Moderately Dissected Basaltic Plateau Major Drainage : Tributaries of Bhima River 3. LAND USE (2010-11) Forest Area : 342 sq. km. Non Cutivation Area : 788.97 sq. km. Cultivation Area : 11315.22 sq. km. GW Irrigated Area : 1788.09 sq km 4. SOIL TYPE Very Shallow, Shallow, Medium and Deep Soils 5. IRRIGATION BY DIFFERENT SOURCES (2006-07 MI CENSUS) - Nos./Potential Created /Potential Utilised(ha) Dugwells : 132842/327709 Borewells : 28786/65308 Total GW Potential Created 393017 Surface Flow Schemes : 174/265 Surface Lift Schemes : 37874/98404 Net Potential Created : 494686 ha 6. GROUND WATER MONITORING WELLS (As on Nov 2012) Dugwells : 53 Piezometers : 6 7. GEOLOGY Quarterny to Recent : Alluvium Upper Cretaceous-Lower Eocene: Basalt (Deccan Trap) 8. -
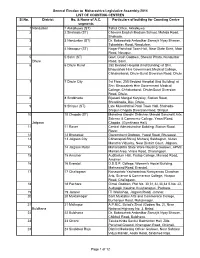
V E 2014 Counting Centres
General Election to Maharashtra Legislative Assembly-2014 LIST OF COUNTING CENTRES Sl.No. District No. & Name of A.C. Particulars of building for Counting Centre segments 1 Nandurbar 1 Akkalkuwa (ST) Tahsil Office, Akkalkuwa 2 2 Shahada (ST) Chavara English Medium School, Mohida Road, Shahada. 3 3 Nandurbar (ST) Dr. Babasaheb Ambedkar Samajik Nyay Bhavan, Tokartalav Road, Nandurbar. 4 4 Nawapur (ST) Nagar Parishad Town Hall, Near State Bank, Main Road, Navapur. 5 5 Sakri (ST) Govt. Grain Godown, Shewali Phata, Nandurbar Dhule Road, Sakri. 6 6 Dhule Rural 250 Bedded Hospital (Iind Building) at Shri. Bhausaheb Hire Government Medical College, Chhakarbardi, Dhule-Surat Diversion Road, Dhule. 7 7 Dhule City 1st Floor, 250 Bedded Hospital (Iind Building) at Shri. Bhausaheb Hire Government Medical College, Chhakarbardi, Dhule-Surat Diversion Road, Dhule. 8 8 Sindkheda Bijasani Mangal Karyalay, Station Road, Shindkheda, Dist. Dhule. 9 9 Shirpur (ST) Late Mukeshbhai Patel Town Hall, Shahada- Shirpur-Chopda Diversion Road, Shirpur. 10 10 Chopda (ST) Mahatma Gandhi Shikshan Mandal Sanchalit Arts, Science & Commerce College, Yawal Road, Jalgaon Chopda. (Gymkhana Hall) 11 11 Raver Central Administrative Building, Station Road, Raver. 12 12 Bhusawal Government Godown, Yawal Road, Bhusawal. 13 13 Jalgaon City Chhatrapati Shivaji Maharaj Sabhagruh, Nutan Maratha Vidyalay, Near District Court, Jalgaon. 14 14 Jalgaon Rural Maharashtra State Ware Housing Godown, APMC Market Area, Virare Road, Dharangaon. 15 15 Amalner Auditorium Hall, Pratap College, Marwad Road, Amalner. 16 16 Erandol D.D.S.P. College, Women's Hostel Building, Mahsawad Road, Erandol. 17 17 Chalisgaon Nanasaheb Yashwantrao Narayanrao Chawhan Arts, Science & Commerece College, Hirapur Road, Chalisgaon. -
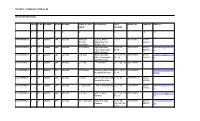
Sr No Pc No Pc Name Ac No Ac Name Zonal Officer Name
DISTRICT COMMUNICATION PLAN SECTOR OFFICER DETAILS SR NO PC NO PC NAME AC NO AC NAME ZONAL OFFICER DESIGNATION AREA MOBILE NO LANDLINE EMAIL ID NAME COVERED 1 2 3 4 5 6 7 8 9 10 11 244 KARMALA 1 43 Madha 244 Karmala Kaustubh Dy.Eng. Bhima 1 To 9 9011032477 02182- Narendr Upasa Sinchan 222033 Saundane Sub.Div. No.1 245 KARMALA 2 43 Madha 244 Karmala S.G.Polake AgriKarmala Supervisor 10 To 14 , 9421031474 02182- [email protected] Taluka Agriculuter 36,77 220516 m Office Karmala 246 KARMALA 3 43 Madha 244 Karmala M.B.Nale Block Education 15 To 20, 34, 9975780099 02182- [email protected] Officer Panchayat 35, 78 221658 n Samiti Karmala 247 KARMALA 4 43 Madha 244 Karmala B P Patil I T I Karmala 21 To 26 , 33 9021182996 248 KARMALA 5 43 Madha 244 Karmala R B Darade Sectengr gramin Pani 27 To 32 95 9423202042 debn.karmala@rediffm Purwatha Karmala To 98 ail.com 249 KARMALA 6 43 Madha 244 Karmala J S Patil Z P Construction Sub 37 To 44 7083631579 02182- Division Karmala 220358 250 KARMALA 7 43 Madha 244 Karmala R C Bansode T Agri office,Karmala 45 To 51 9423389183 02182- [email protected] 220516 m 251 KARMALA 8 43 Madha 244 Karmala D R Tijore Asst. Register 52 To 55, 130 9011541697 [email protected] Karmala To 133 om 252 KARMALA 9 43 Madha 244 Karmala M. S. Kambale Nagar Parishad 56 To 60, 9404318482 02182- [email protected] Karmala 125,126,128, 222033 om 129 253 KARMALA 10 43 Madha 244 Karmala A A Jarande O S P S Karmla , P S 61 To 64, 9421263018 02182- [email protected] Karmala 121,122,124, 220315 m 127 254 KARMALA 11 43 Madha