Automated Immunohistochemical Analysis of the Orbitofrontal Cortex in Patients with Schizophrenia, Bipolar Disorder and Major Depressive Disorder
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nomina Histologica Veterinaria, First Edition
NOMINA HISTOLOGICA VETERINARIA Submitted by the International Committee on Veterinary Histological Nomenclature (ICVHN) to the World Association of Veterinary Anatomists Published on the website of the World Association of Veterinary Anatomists www.wava-amav.org 2017 CONTENTS Introduction i Principles of term construction in N.H.V. iii Cytologia – Cytology 1 Textus epithelialis – Epithelial tissue 10 Textus connectivus – Connective tissue 13 Sanguis et Lympha – Blood and Lymph 17 Textus muscularis – Muscle tissue 19 Textus nervosus – Nerve tissue 20 Splanchnologia – Viscera 23 Systema digestorium – Digestive system 24 Systema respiratorium – Respiratory system 32 Systema urinarium – Urinary system 35 Organa genitalia masculina – Male genital system 38 Organa genitalia feminina – Female genital system 42 Systema endocrinum – Endocrine system 45 Systema cardiovasculare et lymphaticum [Angiologia] – Cardiovascular and lymphatic system 47 Systema nervosum – Nervous system 52 Receptores sensorii et Organa sensuum – Sensory receptors and Sense organs 58 Integumentum – Integument 64 INTRODUCTION The preparations leading to the publication of the present first edition of the Nomina Histologica Veterinaria has a long history spanning more than 50 years. Under the auspices of the World Association of Veterinary Anatomists (W.A.V.A.), the International Committee on Veterinary Anatomical Nomenclature (I.C.V.A.N.) appointed in Giessen, 1965, a Subcommittee on Histology and Embryology which started a working relation with the Subcommittee on Histology of the former International Anatomical Nomenclature Committee. In Mexico City, 1971, this Subcommittee presented a document entitled Nomina Histologica Veterinaria: A Working Draft as a basis for the continued work of the newly-appointed Subcommittee on Histological Nomenclature. This resulted in the editing of the Nomina Histologica Veterinaria: A Working Draft II (Toulouse, 1974), followed by preparations for publication of a Nomina Histologica Veterinaria. -
Limbic Areas Have Been Quantitatively Stud Tex: an Outer Layer of Small Granular Type Cells, An
CHAPTER 15 Development of the Limbic Cortical Areas 15.1 Neurogenetic Gradients in the Lateral Limbic 15.2.3 The Retrosplenial Area, 195 Areas, 187 15.2.4 Gradients Between Areas, 197 15.1.1 Radial and Transverse Neurogenetic 15.3 Neurogenetic Gradients in- the Orbital Cortex, Gradients, 188 197 15.1.2 Unique Longitudinal Neurogenetic 15.4 Correlations Between Neurogenetic Gradients Gradients, 188 and Anatomical Connections in the Limbic 15.2 Neurogenetic Gradients in the Medial Limbic Cortex, 198 Areas, 191 15.4.1 Connections of the Anterior Thalamic 15.2.1 The Dorsal Peduncular and Infralimbic Nuclear Complex with the Medial Limbic Areas, 191 Cortex, 198 15.2.2 The Cingulate Areas, 193 15.4.2 Thalamocortical Connections of the Gustatory Cortex, 198 As early as 1664, Thomas Willis wrote that the cortex hypothesis and named the interconnected cortical and on the borders of the cerebral hemispheres had unique subcortical structures the limbic system. Since then, anatomical features resembling a "hem" or "limbus." anatomical and functional links in the limbic system in In his 1878 paper, Broca called that area the "grande general and the medial limbic cortex in particular have lobe limbique" (reviewed in White, 1965). In rats as been widely studied in relation to behavior (Isaacson, well as in man, the limbic lobe is a continuous cortical 1974) and support has been provided for Papez' orig band encircling the neocortex. In this chapter, we use inal hypothesis. The participation of the lateral limbic the term limbic cortex to include parts of Broca's cortex in other circuits involved with emotional be limbic lobe that have been traditionally considered havior was' emphasized by Livingston and Escobar neocortex by some (Papez, 1937; MacLean, 1952; (1971). -

Neuronal Properties and Synaptic Connectivity in Rodent Presubiculum Jean Simonnet
Neuronal properties and synaptic connectivity in rodent presubiculum Jean Simonnet To cite this version: Jean Simonnet. Neuronal properties and synaptic connectivity in rodent presubiculum. Neurons and Cognition [q-bio.NC]. Université Pierre et Marie Curie - Paris VI, 2014. English. NNT : 2014PA066435. tel-02295014 HAL Id: tel-02295014 https://tel.archives-ouvertes.fr/tel-02295014 Submitted on 24 Sep 2019 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. THÈSE DE DOCTORAT DE L’UNIVERSITÉ PIERRE ET MARIE CURIE Spécialité Neurosciences École doctorale Cerveau – Cognition – Comportement Présentée par : Jean Simonnet Pour obtenir le grade de DOCTEUR DE L’UNIVERSITÉ PIERRE ET MARIE CURIE Sujet de la thèse : Neuronal properties and synaptic connectivity in rodent presubiculum Soutenue le 23.09.2014 devant le jury composé de : Dr Jean-Christophe Poncer Président Dr Dominique Debanne Rapporteur Dr Maria Cecilia Angulo Rapportrice Pr Hannah Monyer Examinatrice Dr Bruno Cauli Examinateur Dr Desdemona Fricker Directrice de thèse Université Pierre & Marie Curie - Paris 6 Tél. Secrétariat : 01 42 34 68 35 Bureau d’accueil, inscription des doctorants Fax : 01 42 34 68 40 et base de données Tél. pour les étudiants de A à EL : 01 42 34 68 41 Esc. -

4 Bayer Exp Neurol 107 1
EXPERIMENTALNEUROLOGY 107,11&131(1990) Development of the Lateral and Medial Limbic Cortices in the Rat in Relation to Cortical Phylogeny SHIRLEY A. BAYER Department of Biology, Indiana-Purdue University, Indianapolis, Indiana 46205 limbique” (as reviewed in Ref. (45)). In rats and in man, [‘H]Thymidine autoradiography was used to investi- the limbic lobe is a continuous cortical band encircling gate neurogenesis of the lateral limbic cortex and mor- the neocortex. Phylogenetic relationships within the phogenesis of the medial and lateral limbic cortices in limbic lobe and with the neocortex were often the sub- adult and embryonic rat brains. Ontogenetic patterns jects of contradicting opinions and confusing terminol- in the limbic cortex are unique because some neuroge- ogy in the classical neuroanatomical literature (1,2,22, netic gradients are linked to those in neocortex, others 40). None of the hypotheses has found general accep- are linked to those in paleocortex. These findings are tance, and interest in the topic of evolutionary origin has related to hypotheses of cortical phylogeny. The experi- waned in recent years. Since ontogenetic patterns are mental animals used for neurogenesis were the off- important clues to phylogenetic links, a comprehensive spring of pregnant females injected with [‘Hlthymidine developmental study of the limbic lobe as a whole would on 2 consecutive days: Embryonic Day (E)13-E14, shed new light on old controversies. In 1974, Bayer and E14-E15, . E21-E22, respectively. On Postnatal Altman (10) started using the comprehensive labeling Day (P)60, the proportion of neurons originating dur- method of [3H]thymidine autoradiography to quantita- ing 24-h periods were quantified at nine anteroposte- tively determine timetables of neuronal birthdays rior levels and one sagittal level. -

Multimodal Mapping and Analysis of the Cyto- and Receptorarchitecture of the Human Hippocampus
Brain Structure and Function (2020) 225:881–907 https://doi.org/10.1007/s00429-019-02022-4 ORIGINAL ARTICLE Multimodal mapping and analysis of the cyto‑ and receptorarchitecture of the human hippocampus Nicola Palomero‑Gallagher1,2,3 · Olga Kedo1 · Hartmut Mohlberg1 · Karl Zilles1,4 · Katrin Amunts1,3 Received: 19 June 2019 / Accepted: 26 December 2019 / Published online: 18 January 2020 © The Author(s) 2020 Abstract The human hippocampal formation is relevant for various aspects of memory and learning, and the diferent hippocampal regions are diferentially afected by neuropsychiatric disorders. Therefore, the hippocampal formation has been subject of numerous cytoarchitectonic and other mapping studies, which resulted in divergent parcellation schemes. To understand the principles of hippocampal architecture, it is necessary to integrate diferent levels of hippocampal organisation, going beyond one modality. We here applied a multimodal mapping approach combining cyto- and multi-receptorarchitectonic analyses, and generated probabilistic maps in stereotaxic space of the identifed regions. Cytoarchitecture in combination with the regional and laminar distribution of 15 neurotransmitter receptors visualized by in vitro receptor autoradiography were analysed in seven hemispheres from 6 unfxed shock frozen and serially sectioned brains. Cytoarchitectonic delineations for generation of probabilistic maps were carried out on histological sections from ten fxed, parafn embedded and serially sectioned brains. Nine cyto- and receptorarchitectonically distinct regions were identifed within the hippocampal formation (i.e., fascia dentata, cornu Ammonis (CA) regions 1–4, prosubiculum, subiculum proper, presubiculum and parasubiculum), as well as the hippocampal-amygdaloid transition area and the periallocortical transsubiculum. Subsequently generated probabilistic maps quantify intersubject variability in the size and extent of these cyto- and receptorarchitectonically distinct regions. -

History, Anatomical Nomenclature, Comparative Anatomy and Functions of the Hippocampal Formation
Bratisl Lek Listy 2006; 107 (4): 103106 103 TOPICAL REVIEW History, anatomical nomenclature, comparative anatomy and functions of the hippocampal formation El Falougy H, Benuska J Institute of Anatomy, Faculty of Medicine, Comenius University, Bratislava, [email protected] Abstract The complex structures in the cerebral hemispheres is included under one term, the limbic system. Our conception of this system and its special functions rises from the comparative neuroanatomical and neurophysiological studies. The components of the limbic system are the hippocampus, gyrus parahippocampalis, gyrus dentatus, gyrus cinguli, corpus amygdaloideum, nuclei anteriores thalami, hypothalamus and gyrus paraterminalis Because of its unique macroscopic and microscopic structure, the hippocampus is a conspicuous part of the limbic system. During phylogenetic development, the hippocampus developed from a simple cortical plate in amphibians into complex three-dimensional convoluted structure in mammals. In the last few decades, structures of the limbic system were extensively studied. Attention was directed to the physi- ological functions and pathological changes of the hippocampus. Experimental studies proved that the hippocampus has a very important role in the process of learning and memory. Another important functions of the hippocampus as a part of the limbic system is its role in regulation of sexual and emotional behaviour. The term hippocampal formation is defined as the complex of six structures: gyrus dentatus, hippocampus proprius, subiculum proprium, presubiculum, parasubiculum and area entorhinalis In this work we attempt to present a brief review of knowledge about the hippocampus from the point of view of history, anatomical nomenclature, comparative anatomy and functions (Tab. 1, Fig. 2, Ref. -

PDF Hosted at the Radboud Repository of the Radboud University Nijmegen
PDF hosted at the Radboud Repository of the Radboud University Nijmegen The following full text is a publisher's version. For additional information about this publication click this link. http://hdl.handle.net/2066/113728 Please be advised that this information was generated on 2021-10-11 and may be subject to change. THE HIPPOCAMPAL FORMATION IN NORMAL AGING AND ALZHEIMER'S DISEASE A MORPHOMETRIC STUDY HARKE DE VRIES THE HXX'X'OCÄJVLE'AX. FOFtlVITVrX CMST I IST JsiORjyrzvx. ÍVGXISÍ<3 ÎVISTD г х^ZH:E:xiynE:R » s XiXSEASE г^. ІУІОЬІ^НОІУЕЕТІІХС; STXXDY THE HIPPOCAMPAL FORMATION IN NORMAL· AGING AND ALZHEIMER'S DISEASE A MORPHOMETRIC STUDY een wetenschappelijke proeve op het gebied van de geneeskunde en tandheeIkunde Proefschrift ter verkrijging van de graad van doctor aan de Katholieke Universiteit te Nijmegen volgens besluit van het college van decanen in het openbaar te verdedigen op woensdag 21 februari 1990 des namiddags te 1.30 uur precies door geboren op 27 augustu199s 0195 7 te Badhocvedorp Drukkerij Leijn te Nijmegen Promotores: Prof. dr. R. Nieuwenhuys Prof. dr. G.J. ZwaniJOcen Co-promotor: Dr. J. Meek ...In the beginner's mind there is no thought "I have attained something"... (Shunryu Suzuki, in: Zen Mind, Beginner's Mind) Dedicated to my mother, In memory of my father. ISBN 90-9003283-5 CONTENTS CHAPTER 1 GENERAL INTRODUCTION 2 1.1 Epidemiology of Alzheimer's disease 3 1.2 Diagnosis of Alzheimer's disease 4 1.3 Hypotheses on the etiology of Alzheimer's disease....4 1.4 Infectious agents 5 1. 5 Neurotoxic agents 6 1.6 Dysfunction of the blood-brain barrier 6 1.7 Neurotransmitter and receptor deficiencies, neurotransmitter cytotoxicity 7 1. -

Limbic System)
Telencephalon Structure of telencephalon Gray matter Cortex (pallium) Basal ganglia (striatum) White matter - pathways Projection Commissural Association Cerebral cortex ALLOCORTEX 3-5 layers a) palleocortex (rhinencephalon) archicortex b) archicortex (limbic system) MESOCORTEX = palleocortex peripaleocortex, periarchicortex NEOCORTEX (ISOCORTEX) 6 layers Rhinencephalon Limbic lobe Bulbus olfactorius Gyrus cinguli Tractus olfactorius Gyrus parahippocampalis Tuberculum olf. Indusium griseum Stria olf. med. et lat. HippocampalARCHICORTEX complex: Hippocampus (cornu ammonis, CA) Gyrus dentatus Subiculum Fornix Limbic system – classic conception Papez‘s circuit (James Papez 1939) without specific function ncl. anterior thalami tr. mammilo-thalamicus ncl. mamillaris gyrus cinguli fornix gyrus parahippocampalis hippocampus RECENT CONCEPTION OF LIMBIC FOREBRAIN • basomedial telencephalon, structures of diencephalon and mesencephalon for emotion and motivation of our behavior Regular structures • g. cinguli, g. parahippocampalis, hippocampus, insular cortex, neocortical regions of forebrain - basal frontotemporal regions, orbital cortex • area septalis, amygdalar ncll., ventral striatum (pallidum) • ncl. anterior et medialis dorsalis thalami, habenulla • hypothalamus (ncl. mammillaris) Limbic system – classic conception Papez‘s circuit (James Papez 1939) Image of tooth pain Image of fear Reminiscence of music hearing Brodman’s map (cytoarchitectonic map of cortex) 11 regiones 52 areae Functional regions of cortex Primary motor c. (a 4), primary -

Download the Atlas Plates and Related Structures
bioRxiv preprint doi: https://doi.org/10.1101/2021.07.14.452297; this version posted July 14, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Cellular resolution anatomical and molecular atlases for prenatal human brains Song‐Lin Ding1,*, Joshua J. Royall1, Phil Lesnar1, Benjamin A.C. Facer1, Kimberly A. Smith1, Yina Wei1,4, Kristina Brouner1, Rachel A. Dalley1, Nick Dee1, Tim A. Dolbeare1, Amanda Ebbert1, Ian A. Glass2, Katie Glattfelter1, Nika H. Keller1, Felix Lee1, Tracy A. Lemon1, Julie Nyhus1, Julie Pendergraft1, Robert Reid1, Melaine Sarreal1, Nadiya V. Shapovalova1, Aaron Szafer1, John W. Phillips1, Susan M. Sunkin1, John G. Hohmann1, Allan R. Jones1, Michael J. Hawrylycz1, Patrick R. Hof3, Lydia Ng1, Amy Bernard1, Ed S. Lein1,* 1. Allen Institute for Brain Science, Seattle, WA 98109 2. Department of Pediatrics and Medicine, University of Washington School of Medicine, Seattle, WA 98105 3. Nash Family Department of Neuroscience and Friedman Brain Institute, Icahn School of Medicine at Mount Sinai, New York, NY 11029 4. Zhejiang Lab, Hangzhou, Zhejiang, China *correspondence: [email protected] or [email protected] Keywords: human brain atlas, gene expression, brain development, cerebral cortex, hippocampal formation, amygdala, thalamic nuclei, olfactory bulb, ganglionic eminence, subventricular zone. 1 bioRxiv preprint doi: https://doi.org/10.1101/2021.07.14.452297; this version posted July 14, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. -
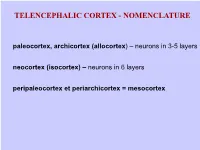
Paleocortex, Archicortex (Allocortex) – Neurons in 3-5 Layers Neocortex (Isocortex) – Neurons in 6 Layers Peripaleocortex Et Periarchicortex = Mesocortex
TELENCEPHALIC CORTEX - NOMENCLATURE paleocortex, archicortex (allocortex) – neurons in 3-5 layers neocortex (isocortex) – neurons in 6 layers peripaleocortex et periarchicortex = mesocortex LOCATION OF MAIN FUNCTIONAL REGIONS OF TELENCEPHALIC CORTEX somatosenzory and senzory motor cortex of limbic forebrain association cortex a43 CORTICAL AREAS FOR SPEECH - I Broca‘s (motor) cortical area - g. front. inf. a44, 45 for right-hander in L-hemisphere, for left-hander in R-hemisphere Wernicke‘s (sensory) cortical area - a 22,39,40 in dominant hemi- sphere CORTICAL AREAS FOR SPEECH - II A SCHEMATIC DRAWING OF 3D ARRANGEMENT OF SOME TELENCEFALIC STRUCTURES Limbic system – classic conception Papez‘s circuit (James Papez 1939) without specific function ncl. anterior thalami tr. mammilo-thalamicus ncl. mamillaris gyrus cinguli fornix gyrus parahippocampalis hippocampus RECENT CONCEPTION OF LIMBIC FOREBRAIN • basomedial telencephalon, structures of diencephalon and mesencephalon for emotion and motivation of our behavior Regular structures • g. cinguli, g. parahippocampalis, hippocampus, insular cortex • neocortical regions of forebrain - basal frontotemporal regions, orbital cortex, ventral striatum (pallidum) • area septalis, amygdalar ncll., hypothalamus (ncl. mammillaris) • ncl. anterior et medialis dorsalis thalami • habenulla Limbic system – classic conception Papez‘s circuit (James Papez 1939) notion of tooth pain notion of fear memory of listening to music AMYGDALAR NUCLEI BASAL GANGLIA AND RELATED STRUCTURES ncl. caudatus, putamen, globus pallidus, claustrum and amygdalar ncll. functional: + thalamus, substantia nigra and ncl. subthalamicus ncl. caudatus + putamen = neostriatum (striatum) globus pallidus (ext. + int. segment) = paleostriatum (pallidum) globus pallidus + putamen = ncl. lentiformis BASAL GANGLIA AND RELATED STRUCTURES ncl. caudatus dorsal striatum striatum (neostriatum) putamen ncl. accumbens ventral striatum Basal ganglia lat. (external) seg. globus pallidus dorsal pallidum (pallidum, paleostriatum) med. -
A Cortical Brain MRI Atlas Following a Phylogenetic Approach
bioRxiv preprint doi: https://doi.org/10.1101/2020.07.15.205401; this version posted July 16, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. PhyloBrain atlas: a cortical brain MRI atlas following a phylogenetic approach Zhernovaia M, MD. PhD1; Dadar M, PhD 2-3; Mahmoud S1. MD; Zeighami Y, PhD3; Maranzano, MD, PhD1;3. (1) Anatomy Department, Université du Québec à Trois-Rivières (2) Radiology Department, Faculty of Medicine, LavaL University (3) McConneL Brain Imaging Center, MontreaL NeurologicaL Institute, McGiLL University Corresponding author: Josefina Maranzano, MD, PhD. [email protected] [email protected] - University of Québec in Trois-Rivières, Department of Anatomy. PaviLLon Léon-Provancher. LocaL 3501. 3351, boulevard des Forges, Trois-Rivières, Québec, Canada. G8Z 4M3. - McGiLL University, Department of Neurology and Neurosurgery, MontréaL NeurologicaL Institute. 3801 Rue University, Room WB327, MontréaL, Québec, Canada, H3A 2B4 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.07.15.205401; this version posted July 16, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. ABSTRACT CorticaL atLases constitute a consistent division of the human cortex into areas that have common structuraL as weLL as meaningful and distinctive functionaL characteristics. -

Postnatal Development of the Human Hippocampal Formation (Advances
Reviews and critical articles covering the entire field of normal anatomy (cytology, histology, cyto- and histochemistry, electron microscopy, macroscopy, experi- mental morphology and embryology and comparative anatomy) are published in Advancesin Anatomy, Embryology and Cell Biology. Papers dealing with anthro- pology and clinical morphology that aim to encourage cooperation between anatomy andrelated disciplines will also be accepted. Papers are normally com- missioned. Original papers and communications may be submitted and will be considered for publication provided they meet the requirements of a review article and thus fit into the scope of “Advances”. English language is preferred. It is a fundamental condition that submitted manuscripts have not been and will not simultaneously be submitted or published elsewhere. With the acceptance of a manuscript for publication, the publisher acquires full and exclusive copyright for all languages and countries. Twenty-five copies of each paper are supplied free of charge. Manuscripts should be addressed to Co-ordinating Editor Prof. Dr. H.-W. KORF, Zentrum der Morphologie, Universita¨t Frankfurt, Theodor-Stern Kai 7, 60595 Frankfurt/Main, Germany e-mail: [email protected] Editors Prof. Dr. F. BECK, Howard Florey Institute, University of Melbourne, Parkville, 3000 Melbourne, Victoria, Australia e-mail: [email protected] Prof. Dr. F. CLASCA´ , Department of Anatomy, Histology and Neurobiology Universidad Auto´noma de Madrid, Ave. Arzobispo Morcillo s/n, 28029 Madrid, Spain e-mail: [email protected] Prof. Dr. M. FROTSCHER, Institut fu¨r Anatomie und Zellbiologie, Abteilung fu¨r Neuroanatomie, Albert-Ludwigs-Universita¨t Freiburg, Albertstr. 17, 79001 Freiburg, Germany e-mail: [email protected] Prof.