An Enquiry Into Provision of Abortion Services in Madhya Pradesh Dr
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Forest of Madhya Pradesh
Build Your Own Success Story! FOREST OF MADHYA PRADESH As per the report (ISFR) MP has the largest forest cover in the country followed by Arunachal Pradesh and Chhattisgarh. Forest Cover (Area-wise): Madhya Pradesh> Arunachal Pradesh> Chhattisgarh> Odisha> Maharashtra. Forest Cover (Percentage): Mizoram (85.4%)> Arunachal Pradesh (79.63%)> Meghalaya (76.33%) According to India State of Forest Report the recorded forest area of the state is 94,689 sq. km which is 30.72% of its geographical area. According to Indian state of forest Report (ISFR – 2019) the total forest cover in M.P. increased to 77,482.49 sq km which is 25.14% of the states geographical area. The forest area in MP is increased by 68.49 sq km. The first forest policy of Madhya Pradesh was made in 1952 and the second forest policy was made in 2005. Madhya Pradesh has a total of 925 forest villages of which 98 forest villages are deserted or located in national part and sanctuaries. MP is the first state to nationalise 100% of the forests. Among the districts, Balaghat has the densest forest cover, with 53.44 per cent of its area covered by forests. Ujjain (0.59 per cent) has the least forest cover among the districts In terms of forest canopy density classes: Very dense forest covers an area of 6676 sq km (2.17%) of the geograhical area. Moderately dense forest covers an area of 34, 341 sqkm (11.14% of geograhical area). Open forest covers an area of 36, 465 sq km (11.83% of geographical area) Madhya Pradesh has 0.06 sq km. -

District Census Handbook, Satna, Part XIII-A, Series-11
lIltT XI1I-Cfi • • 1 ~. m. ~i, l I "fm(lq SI'~,,,f.f1fi ~"T i ~ iiJOIllVfff' I 'It-11' srnt I 1981 cENsas-PUBLlCATION PLAN (1981 Census Publi~Qtions, Series 11 in All India Series will be published in the following parts) GOVERNMENT OF INDIA PUBLICATIONS Part I-A Ad ministration Repo rt- Enumera tion Part I-B Administration Report-Tabulation P-art n ...:A General Population Tables Part U-B Primary Census Abstract Part 111 General Economic Tables Part IV Social and Cultural Tables Part V Migration Tables Part VI Fertility Tanles Part VII Tables on Houses and Disabled Population Part VIII Household Tables Part IX Special Tables on Scheduled Castes and Scheduled Tribes Part X-A Town Directory Part X-B . Survey Reports on selected Towns Part x-C Survey RepoFts on sele~ted Villages Part XI Ethnographic Notes and special studies on Schedultd Castes and Sched uled Tribes Part XTJ . Census Atlas Paper 1 of 1982 Primary Census Abstract for Sched~lled Castes and,Scheduled Tribes Paper 1 of 1984 HOllsehold Population by Religion of Head of Household STATE GOVERNMENT PUBLlCATIONS Part XIlI-A&B District Census Handbook for each of the 45 districts in the State. (Village and Town Directory and Primary Census Abstract) f~~~~ CONTENTS '{GQ W&I1T Pages 1 SIt"'fi"''' Foreword i-iv 2 sr,",,",,,, Preface v-vi 3 fiil~ "" ;mfT District Map 4 q~tCl1!.qf." Important Statistics vii 5 fcr~QV(rt~ fC!'tq'1'T Analytical Note ix-xnviii alfT~tI'T~l1Cfi fC'cqoit; ~,!~f"'ij' \ifTfij' ~T<:: ~~~f"{ij' Notes & Explanations; List of Scheduled ,;;r;:r~Tfu 'fir \I:"f1 ( «wTS"rr ) ~ fq~ll"'fi 1 9 76: Castes and Scheduled Tribes Order f::sr~T ~qlJ{;rT ~ftij''flT <fiT ~fij'~Ht IR"~ &i~ I (Amendment) Act, 1976. -

State Zone Commissionerate Name Division Name Range Name
Commissionerate State Zone Division Name Range Name Range Jurisdiction Name Gujarat Ahmedabad Ahmedabad South Rakhial Range I On the northern side the jurisdiction extends upto and inclusive of Ajaji-ni-Canal, Khodani Muvadi, Ringlu-ni-Muvadi and Badodara Village of Daskroi Taluka. It extends Undrel, Bhavda, Bakrol-Bujrang, Susserny, Ketrod, Vastral, Vadod of Daskroi Taluka and including the area to the south of Ahmedabad-Zalod Highway. On southern side it extends upto Gomtipur Jhulta Minars, Rasta Amraiwadi road from its intersection with Narol-Naroda Highway towards east. On the western side it extend upto Gomtipur road, Sukhramnagar road except Gomtipur area including textile mills viz. Ahmedabad New Cotton Mills, Mihir Textiles, Ashima Denims & Bharat Suryodaya(closed). Gujarat Ahmedabad Ahmedabad South Rakhial Range II On the northern side of this range extends upto the road from Udyognagar Post Office to Viratnagar (excluding Viratnagar) Narol-Naroda Highway (Soni ni Chawl) upto Mehta Petrol Pump at Rakhial Odhav Road. From Malaksaban Stadium and railway crossing Lal Bahadur Shashtri Marg upto Mehta Petrol Pump on Rakhial-Odhav. On the eastern side it extends from Mehta Petrol Pump to opposite of Sukhramnagar at Khandubhai Desai Marg. On Southern side it excludes upto Narol-Naroda Highway from its crossing by Odhav Road to Rajdeep Society. On the southern side it extends upto kulcha road from Rajdeep Society to Nagarvel Hanuman upto Gomtipur Road(excluding Gomtipur Village) from opposite side of Khandubhai Marg. Jurisdiction of this range including seven Mills viz. Anil Synthetics, New Rajpur Mills, Monogram Mills, Vivekananda Mill, Soma Textile Mills, Ajit Mills and Marsdan Spinning Mills. -

Territoires Infectés À La Date Du 7 Juillet 1960 — Infected Areas As on 7
— 308 Territoires infectés à la date du 7 juillet 1960 — Infected areas as on 7 July 1960 Notifications reçues aux termes du Règlement sanitaire Notifications received under the International Sanitary international concernant les circonscriptions infectées ou Regulations relating to infected local areas and to areas les territoires oà la présence de maladies guarantenaires in which the presence o f quarantinable diseases was a été signalée (voir page 167). reported (see page 167), ■ = Circonscriptions ou territoires notifiés aux termes de l’artide 3 • = Areas notified under Article 3 on the date indicated. à la date donnée. Autres territoires où la présence de maladies quarantenaires a été' Other areas in which the presence of quarantinable diseases was notifiée aux termes des articles 4, 5 et 9 a: notified under Articles 4, 5 and 9 (a): Â — pendant la période indiquée sous le nom de chaque maladie; A = during the period indicated under the heading of each disease; B = antérieurement à la période indiquée sous le nom de chaque B = prior to the period indicated under the heading of each maladie. disease. PESTE — PLAGXJE Andhra Pradesh, State FIEVRE JAUNE COTE D ’IVOIRE — IVORY COAST 19. VI-7 .VII East Godavari, District . ■ 28.XII.59 YELLOW FEVER Abengourou, Cercle. A 30.VI Guntur District .... ■ 31.XII.59 Abidjan, Cercle .... A 30.VI Amérique America Krishna, District .... ■ 27.VIII.59 io.iv-7.vn Agboville, Cercle .... A 23.VI Srikakulam, District . ■ ll.VI Bondoukou, Cercle . A 9.VI ÉQUATEUR — ECUADOR West Godavari, District . ■ 27,VIII.59 Afrique — Africa Bouaflé, Cercle............... A 23.VI Bouaké, Cercle .... -

District Disaster Management Plan Sidhi
District Disaster Management Plan Sidhi By Nishant Maheshwari (MBA-IIT Kanpur) MP School of Good Governance & Policy analysis In Consultation with School of Good Governance & Policy Analysis, Bhopal Seeds Technical Services Government of Madhya Pradesh District Administration, Sidhi District Disaster Management Plan [DDMP] Template Preface Sidhi Disaster Management Plan is a part of multi-level planning advocated by the Madhya Pradesh State Disaster Management Authority (MPSDMA) under DM Act of 2005 to help the District administration for effective response during the disaster. Sidhi is prone to natural as well as man- made disasters. Earthquake, Drought, Epidemic (Malaria) are the major Natural Hazards and forest fire, rail/ road accidents etc. are the main man-made disaster of the district. The Disaster Management plan includes facts and figures those have been collected from various departments. This plan is first attempt of the district administration and is a comprehensive document which contains various chapters and each chapter has its own importance. The plan consist Hazard & Risk Assessment, Institutional Mechanism, Response Mechanism, Standard Operating Procedure, inventory of Resources etc. Hazard & Risk Assessment is done on the basis of past thirty year disaster data & is collected from all departments. It is suggested that the District level officials of different department will carefully go through the plan and if have any suggestions & comments be free to convey the same so that same can be included in the next edition. It is hoped that the plan would provide concrete guidelines towards preparedness and quick response in case of an emergency and help in realizing sustainable Disaster Risk Reduction & mitigate/minimizes the losses in the district in the long run. -
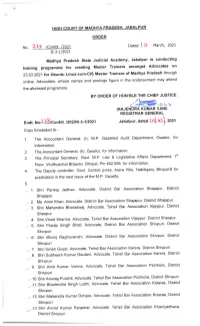
Trajenffijfri[,.Try REGISTRAR GENERAL
E±oH CouRT oF MADrTVA PRADESH, jABALP±±B ORDER Dated |0 March, 2021 NO. Confdl. 11-3-1/2021 Madhya Pradesh State Judicial Academy, Jabalpur is conducting training programme for creating Master Trainers amongst Advocates on 23.03.2021 for Ubuntu Linux-cum-CIS Master Trainers of Madhya Pradesh through online. Advocates, whose names and postings figure in the endorsement may attend the aforesaid programme. BY ORDER 0F HON'BLE THE CHIEF JUSTICE tRAjENffijfri[,.try REGISTRAR GENERAL Endt. No2.I.8/Confdl. /2020/11-3-1/2021 Jabalpur,dated.Ig|..Q3.},2021 Copy forwarded to:- 1. The Accountant General, (I), M.P. Gazetted Audit Department, Gwalior, for information. 2. The Accountant General, (ll), Gwalior, for information. 3. The Principal Secretary, Govt. M.P. Law & Legislative Affairs Department, 1st Floor, Vindhyachal Bhawan, Bhopal, Pin 462 006, for information. 4. The Deputy controller, Govt. Central press, Arera Hills, Habibganj, Bhopal-6 for publication in the next issue of the M.P. Gazette. 5. r,1. Shri Pankaj Jadhav, Advocate, District Bar Association Shajapur, District Shajapur 2. Ms. Amin Khan, Advocate, District Bar Association Shajapur, District Shajapur 3. Shri Mahendra Bharadwaj, Advocate, Tehsil Bar Association Vijaypur, District Sheopur 4. Shri Vinod Sharma, Advocate, Tehsil Bar Association Vijaypur, District Sheopur 5. Shri Pradip Singh Bhati, Advocate, District Bar Association Shivpuri, District Shivpuri + 6. Shri Monoj Raghuvanshi, Advocate, District Bar Association Shivpuri, District Shivpuri 7. Shri Girish Goyal, Advocate, Tehsil Bar Association Karera, District Shivpuri 8. Shri Subheem Kumar Gautam, Advocate, Tehsil Bar Association Karera, District '. shivpuri 9. Shri Amit Kumar Verma, Advocate, Tehsil Bar Association Pichhore, District Shivpuri gr 10. -

2006-07 2006-07 2005-06 2004-05*** 2003-04 2002-03** 2001-02 2000-01 1999-00 1998-99 1997-98 PROFITABILITY Mn US$*
Mr. G. D. Birla and Mr. Aditya Birla, our founding fathers. We live by their values. Integrity, Commitment, Passion, Seamlessness and Speed M C M C Y K Y K Hindalco’s well-crafted growth and integration hinges on the three cornerstones of COST COMPETITIVENESS Reflected through its strong manufacturing base and operational efficiencies QUALITY Through its versatile range of products serving core applications for diverse industries; and Integrated Aluminium Complex Integrated Copper Complex Power Plant Aluminium Extrusions Plant GLOBAL REACH Bauxite Mines Coal Mines Aluminium Foil Plant Competing in markets across more Alumina Refineries Aluminium Wire Rod Aluminium Alloy Wheels Plant than 40 countries Aluminium Smelter Aluminium Rolled Products Plant R & D Centre Creating Superior Value The Hindalco story unfolds with the establishment of the Company in 1958, the commissioning of the aluminium facility at Renukoot in 1962 and the Renusagar Power Plant in 1967. Over the years, Hindalco has grown into the largest vertically integrated aluminium company in the country and among the largest primary producers of aluminium in Asia. Its copper smelter is today the world’s largest custom smelter at a single location. HINDALCO BUSINESS Share of Net Sales Value Rolled Products 14% Aluminium Extrusions Ingots & Billets 3% Conductor Redraw Rods Top Quartile of lowest cost 9% 5% Aluminium Foil, Alloy Aluminium producers globally Hydrate & Alumina Wheels & Others (Standard & Special) 5% 4% ALUMINIUM Primary Aluminium and Copper 40% registered on the London Metal SAP, DAP & Complexes, Precious Metals & Others Exchange 9% Concast Copper Rods COPPER 20% Star Trading House Status. 60% National Awards in Exports Copper Cathodes 31% M C M C Y K Y K HINDALCO – OUR VISION ALUMINIUM METAL PRODUCTION To be a premium metals major, global in size and reach, with a passionpassion forfor excellence.excellence. -

47270-001: Due Diligence Report on Social Safeguards
Due Diligence Report on Social Safeguard July 2014 IND: Madhya Pradesh District Connectivity Sector Project Sample Subprojects: 1. Chitrangi–Kasar Road 2. Dabra–Bhitawar–Harsi Road 3. Mahua–Chuwahi Road 4. Ujjain–Maksi Road Prepared by the Government of Madhya Pradesh through the Madhya Pradesh Road Development Corporation for the Asian Development Bank CURRENCY EQUIVALENTS Currency unit – Indian Rupees (INR) (as of June 6, 2014) INR1.00 = $ 0.01690 $1.00 = INR 59.0361 ABBREVIATIONS ADB - Asian Development Bank AP - Affected Person CPS - Country Partnership Strategy DP - Displaced Person DDR - due diligence report DPR - Detail Project Report EA - Executive Agency FYP - Five Year Plan GM - General Manager GOMP - Government of Madhya Pradesh GRC - Grievance Redress Committee GRM - Grievance Redress Mechanism HDI - Human Development Index MPRDC - Madhya Pradesh Road Development Corporation PPTA - Project Preparatory Technical Assistance RP - Resettlement Plan This due diligence report is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or staff, and may be preliminary in nature. Your attention is directed to the “terms of use” section of this website. In preparing any country program or strategy, financing any project, or by making any designation of or reference to a particular territory or geographic area in this document, the Asian Development Bank does not intend to make any judgments as to the legal or other status of any territory or area. TABLE OF CONTENTS I. PROJECT OVERVIEW ................................................................................................... 1 A. Project Background ..................................................................................................... 1 II. OBJECTIVES OF DUE DILIGENCE REPORT (DDR) ..................................................... 1 A. Methodology of due diligence ..................................................................................... -

Ecological Studies of the Amphibian Fauna and Their Distribution of Sidhi District (M.P.)
International Journal of Zoology Studies International Journal of Zoology Studies ISSN: 2455-7269; Impact Factor: RJIF 5.14 Received: 23-03-2020; Accepted: 25-04-2020; Published: 28-04-2020 www.zoologyjournals.com Volume 5; Issue 2; 2020; Page No. 27-30 Ecological studies of the amphibian fauna and their distribution of Sidhi district (M.P.) Balram Das1, Urmila Ahirwar2 1 Assistant Professor & Head, Department of Zoology, Govt. College, Amarpatan, Distt. Satna, Madhya Pradesh, India 2 Research Scholar, S.G.S. Govt. P.G. College, Sidhi, A.P.S. University, Rewa, Madhya Pradesh, India Abstract The amphibians was represented by 15 species belonging to 13 genera of 6 families and 2 orders from Sidhi district, Madhya Pradesh, India, during 2018 to 2019. Considering number of species in each family Bufonids with 2 species, Dicroglossids 5 species, Microhylids 2 species, Ranids 2 species, Rhacophorids 2 species and 2 species of Ichthyophids. The highest number of amphibian species was recorded from Gopad Banas tehsil (13 species), while the lowest number of species was observed in Sihawal tehsil (2 species). Status of amphibians shows that 5 species are abundant, 2 are common and 8 species are rare in the study sites. Keywords: Amphibian diversity, distribution, status, Sidhi district 1. Introduction distribution, habitat and status. This survey affords baseline The growing attention of populace in cities and the sizeable information and scientific facts for conservation of pace of development and growth of city areas have led to amphibians from arid zone. the emergence of unique prerequisites forming populations and communities, which range notably from the natural. -

Sidhi District
SIDHI DISTRICT MADHYA PRADESH Ministry of Water Resources Central Ground Water Board North Central Region Government of India 2013 SIDHI DISTRICT AT A GLANCE S.No. Items Statistics 1 General Information i) Geographical Area 485400 Ha District Head Quarter Sidhi ii) Administrative Division Number of Tehsil/Block 5 Block Number of Villages (2012) 1882 Population (As per census 2011) 1126515 Normal Annual Rainfall (mm) 1154.2 2. Geomorphology 1. Major Physiographic Units : Kaimur Range Central Part hills Southern Part hills 2. Major Drainage : Son River, Gopad River, Banas nadi, Rihand River 3. Land use a) Forest Area 433533 ha b) Net area sown 275391 ha c) Cultivable area 3745 ha 4. Major Soil Types Red soil, Alluvial & Latertic soil 5. Area Under Principal Crops Paddy, Wheat, Gram, Pulses, maize 6. Irrigation By Different Sources Structures Nos. Area (ha) Dug Wells 11541 26970 Tube wells/Bore wells 11541 12095 Tanks/Ponds 17 453 Canals 160 12453 Other sources 10516 63431 Net irrigated Area - 266976 Gross Irrigated Area - 6343 7. Number of Ground Water Monitoring Wells of CGWB Dug Wells 22 No. of Piezometers 5 8. Predominant Geological Formations Granites, Gneisses, Sandstone, Alluvium 9. Hydrogeology i) Major water bearing formation Gondwana, Vindhayan. ii) Pre monsoon depth to water level 2.60-23.66 mbgl. during 2012 iii) Post monsoon depth to water level 1.05-15.17 mbgl. during 2012 iv) Long term water level trend in 10 0.02-0.21 m/year years (2003-12) falling 10. Ground Water Exploration by CGWB Exploration well EW-17, OW-1, Pz-7 11 -

Working Paper 142 Suresh Reddy May. 2018.P65
Working Paper No. 142 May, 2018 Patterns of Agricultural Transition in Tribal Areas of Madhya Pradesh: A Macro and Micro analysis Dr. B. Suresh Reddy CENTRE FOR ECONOMIC AND SOCIAL STUDIES Begumpet, Hyderabad-500016 Patterns of Agricultural Transition in Tribal Areas of Madhya Pradesh: A Macro and Micro analysis Dr. B. Suresh Reddy* Abstract The agricultural practices have been undergoing changes in all the parts of India in view of the advancements in technology through agricultural research, extension, credit, institutional and policy support extended in different ways. The primary objective of the present paper was to look into the transition taking place in agriculture in tribal areas with a focus on arriving at macro and micro level pictures. The issue of land alienation, forest rights act implementation status and the influence of non-tribals on the farming practices of tribals have also been discussed in this paper. The study is largely drawn both from the primary and secondary data sources. A total of 20 villages were selected in the Jhabua, Mandla and Sidhi districts of M.P. A total sample of 400 Households were selected for the study with twenty households in each village. Focused group discussions(FGDs) were also done with the tribal communities in Jhabua, Mandla and Sidhi districts of M.P. The empirical evidence indicates that agriculture in the tribal areas has shifted to a settled agriculture, excepting a few cases. Under settled agriculture, we could see that a majority have adopted both a combination of modern and traditional methods of farming techniques. We have observed that a small number of sample households continue with conventional agricultural practices which are sustainable in nature and ecologically sound. -

Through Ministry of Roads & Highways
Draft Environment Impact Assessment Report for Four laning with Page No. 1 paved shoulders Sidhi - Singrauli NH-75E 1.1 INTRODUCTION The Govt. of India (GOI) through Ministry of Roads & Highways (MORT&H) is contemplating to enhance the traffic capacity and safety for efficient transshipment of Goods as well as passenger traffic on few of the Selected heavily trafficked stretches/paved shoulder of National Highways. MP Road Development Corporation (MPRDC) plans to take up the development of the selected stretches/corridor of National Highway in the state of Madhya Pradesh on BOT basis. Project will be a Public Private Partnership (PPP) venture in Design – Build – Finance – Operate (DBFO) format. The project road is a part of NH-75E connecting Sidhi to Singrauli. The Project road is the stretch between Km. 83/4 & start at end of Sidhi Bypass and terminates at Km. 195/8 of NH-75E near MP/UP Border in Madhya Pradesh, is 2 lane road of average carriageway of 7.0m which has been planned for “Four- laning with paved shoulder” (the “Project”) through public- private partnership on Design, Build, Finance, Operate and Transfer (the "DBFOT") basis. The land, carriageway and structures comprising the Site are described below. Existing length of Project is 112.2 Kms. Project Description The Project Highway Sidhi-Singrauli Section (NH-75 E) starts from Km. 83/4 at Sidhi Bypass and terminates at Km. 195/6 of NH-75E near MP/UP Border. Hence, the total existing length of the Project Highway is Km. 112.2. Under the proposal, the existing carriageway from Km 83/4 to Km 195/6 is proposed to be widened from 2 lane to 4 lane width with 1.5m wide paved shoulder & 1.0 m granular shoulder along side.