Immune Checkpoint Blockade Enhances Shared Neoantigen-Induced T-Cell Immunity Directed Against Mutated Calreticulin in Myeloproliferative Neoplasms
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

4-1BB Signaling Beyond T Cells
Cellular & Molecular Immunology (2011) 8, 281–284 ß 2011 CSI and USTC. All rights reserved 1672-7681/11 $32.00 www.nature.com/cmi MINI REVIEW 4-1BB signaling beyond T cells Dass S Vinay1 and Byoung S Kwon1,2 Originally discovered as a T cell-activating molecule, 4-1BB (CD137) is now also recognized as an activator of non-T cells, thus imparting a new dimension to its potential in vivo effects. 4-1BB expression is seen on a variety of non-T cells including activated dendritic cells (DCs), monocytes, neutrophils, B cells and natural killer (NK) cells, and promotes their individual effector functions. The T cell- and non-T cell-activating ability of 4-1BB may be the basis of its powerful anti-cancer, anti-autoimmune and anti-viral effects. Here we discuss the consequence and importance of 4-1BB signaling in non-T cells. We consider its effects on immune regulation, and the distinct and/or overlapping pathways involved in these responses, as well as possible therapeutic applications. Cellular & Molecular Immunology (2011) 8, 281–284; doi:10.1038/cmi.2010.82; published online 10 January 2011 Keywords: APC; cytokines; natural killer cells; T cells; 4-1BB INTRODUCTION focus on the functions of 4-1BB in non-T cells including DCs, mono- 4-1BB (CD137; TNFRSF9), discovered originally on T cells,1 is a 50- cytes, neutrophils, B cells and NK cells, and discuss how its expression to 55-kDa protein concerned with progressive immunity.2,3 4-1BB might be manipulated to treat various immune diseases. expression is in most cases activation induced. -

Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse
Welcome to More Choice CD Marker Handbook For more information, please visit: Human bdbiosciences.com/eu/go/humancdmarkers Mouse bdbiosciences.com/eu/go/mousecdmarkers Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse CD3 CD3 CD (cluster of differentiation) molecules are cell surface markers T Cell CD4 CD4 useful for the identification and characterization of leukocytes. The CD CD8 CD8 nomenclature was developed and is maintained through the HLDA (Human Leukocyte Differentiation Antigens) workshop started in 1982. CD45R/B220 CD19 CD19 The goal is to provide standardization of monoclonal antibodies to B Cell CD20 CD22 (B cell activation marker) human antigens across laboratories. To characterize or “workshop” the antibodies, multiple laboratories carry out blind analyses of antibodies. These results independently validate antibody specificity. CD11c CD11c Dendritic Cell CD123 CD123 While the CD nomenclature has been developed for use with human antigens, it is applied to corresponding mouse antigens as well as antigens from other species. However, the mouse and other species NK Cell CD56 CD335 (NKp46) antibodies are not tested by HLDA. Human CD markers were reviewed by the HLDA. New CD markers Stem Cell/ CD34 CD34 were established at the HLDA9 meeting held in Barcelona in 2010. For Precursor hematopoetic stem cell only hematopoetic stem cell only additional information and CD markers please visit www.hcdm.org. Macrophage/ CD14 CD11b/ Mac-1 Monocyte CD33 Ly-71 (F4/80) CD66b Granulocyte CD66b Gr-1/Ly6G Ly6C CD41 CD41 CD61 (Integrin b3) CD61 Platelet CD9 CD62 CD62P (activated platelets) CD235a CD235a Erythrocyte Ter-119 CD146 MECA-32 CD106 CD146 Endothelial Cell CD31 CD62E (activated endothelial cells) Epithelial Cell CD236 CD326 (EPCAM1) For Research Use Only. -

Tools for Cell Therapy and Immunoregulation
RnDSy-lu-2945 Tools for Cell Therapy and Immunoregulation Target Cell TIM-4 SLAM/CD150 BTNL8 PD-L2/B7-DC B7-H1/PD-L1 (Human) Unknown PD-1 B7-1/CD80 TIM-1 SLAM/CD150 Receptor TIM Family SLAM Family Butyrophilins B7/CD28 Families T Cell Multiple Co-Signaling Molecules Co-stimulatory Co-inhibitory Ig Superfamily Regulate T Cell Activation Target Cell T Cell Target Cell T Cell B7-1/CD80 B7-H1/PD-L1 T cell activation requires two signals: 1) recognition of the antigenic peptide/ B7-1/CD80 B7-2/CD86 CTLA-4 major histocompatibility complex (MHC) by the T cell receptor (TCR) and 2) CD28 antigen-independent co-stimulation induced by interactions between B7-2/CD86 B7-H1/PD-L1 B7-1/CD80 co-signaling molecules expressed on target cells, such as antigen-presenting PD-L2/B7-DC PD-1 ICOS cells (APCs), and their T cell-expressed receptors. Engagement of the TCR in B7-H2/ICOS L 2Ig B7-H3 (Mouse) the absence of this second co-stimulatory signal typically results in T cell B7-H1/PD-L1 B7/CD28 Families 4Ig B7-H3 (Human) anergy or apoptosis. In addition, T cell activation can be negatively regulated Unknown Receptors by co-inhibitory molecules present on APCs. Therefore, integration of the 2Ig B7-H3 Unknown B7-H4 (Mouse) Receptors signals transduced by co-stimulatory and co-inhibitory molecules following TCR B7-H5 4Ig B7-H3 engagement directs the outcome and magnitude of a T cell response Unknown Ligand (Human) B7-H5 including the enhancement or suppression of T cell proliferation, B7-H7 Unknown Receptor differentiation, and/or cytokine secretion. -

Megakaryopoiesis in Dengue Virus Infected K562 Cell Promotes Viral Replication Which Inhibits 2 Endomitosis and Accumulation of ROS Associated with Differentiation
bioRxiv preprint doi: https://doi.org/10.1101/2020.06.25.172544; this version posted June 26, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 1 Title: Megakaryopoiesis in Dengue virus infected K562 cell promotes viral replication which inhibits 2 endomitosis and accumulation of ROS associated with differentiation 3 Jaskaran Kaur *1, Yogita Rawat *1, Vikas Sood 2, Deepak Rathore1, Shrikant K. Kumar1, Niraj K. Kumar1 4 and Sankar Bhattacharyya1 5 1 Translational Health Science and Technology Institute, NCR Biotech Science Cluster, PO Box# 4, 6 Faridabad-Gurgaon expressway, Faridabad, Haryana-121001, India 7 2 Department of Biochemistry, School of Chemical and Life Sciences, Jamia Hamdard (Hamdard 8 University) Hamdard Nagar, New Delhi - 110062, India 9 10 *Equal contribution 11 Email for correspondence: [email protected] 12 13 14 Keywords: Dengue virus replication, Megakaryopoiesis, Reactive oxygen species, Endomitosis 15 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.06.25.172544; this version posted June 26, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 16 Abstract: In the human host blood Monocytes and bone marrow Megakaryocytes are implicated as major 17 sites supporting high replication. The human K562 cell line supports DENV replication and represent 18 Megakaryocyte-Erythrocyte progenitors (MEP), replicating features of in vivo Megakaryopoiesis upon 19 stimulation with Phorbol esters. In this article, we report results that indicate the mutual influence of 20 Megakaryopoiesis and DENV replication on each other, through comparison of PMA-induced 21 differentiation of either mock-infected or DENV-infected K562 cells. -
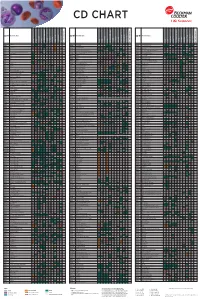
Flow Reagents Single Color Antibodies CD Chart
CD CHART CD N° Alternative Name CD N° Alternative Name CD N° Alternative Name Beckman Coulter Clone Beckman Coulter Clone Beckman Coulter Clone T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells CD1a T6, R4, HTA1 Act p n n p n n S l CD99 MIC2 gene product, E2 p p p CD223 LAG-3 (Lymphocyte activation gene 3) Act n Act p n CD1b R1 Act p n n p n n S CD99R restricted CD99 p p CD224 GGT (γ-glutamyl transferase) p p p p p p CD1c R7, M241 Act S n n p n n S l CD100 SEMA4D (semaphorin 4D) p Low p p p n n CD225 Leu13, interferon induced transmembrane protein 1 (IFITM1). p p p p p CD1d R3 Act S n n Low n n S Intest CD101 V7, P126 Act n p n p n n p CD226 DNAM-1, PTA-1 Act n Act Act Act n p n CD1e R2 n n n n S CD102 ICAM-2 (intercellular adhesion molecule-2) p p n p Folli p CD227 MUC1, mucin 1, episialin, PUM, PEM, EMA, DF3, H23 Act p CD2 T11; Tp50; sheep red blood cell (SRBC) receptor; LFA-2 p S n p n n l CD103 HML-1 (human mucosal lymphocytes antigen 1), integrin aE chain S n n n n n n n l CD228 Melanotransferrin (MT), p97 p p CD3 T3, CD3 complex p n n n n n n n n n l CD104 integrin b4 chain; TSP-1180 n n n n n n n p p CD229 Ly9, T-lymphocyte surface antigen p p n p n -

How Relevant Are Bone Marrow-Derived Mast Cells (Bmmcs) As Models for Tissue Mast Cells? a Comparative Transcriptome Analysis of Bmmcs and Peritoneal Mast Cells
cells Article How Relevant Are Bone Marrow-Derived Mast Cells (BMMCs) as Models for Tissue Mast Cells? A Comparative Transcriptome Analysis of BMMCs and Peritoneal Mast Cells 1, 2, 1 1 2,3 Srinivas Akula y , Aida Paivandy y, Zhirong Fu , Michael Thorpe , Gunnar Pejler and Lars Hellman 1,* 1 Department of Cell and Molecular Biology, Uppsala University, The Biomedical Center, Box 596, SE-751 24 Uppsala, Sweden; [email protected] (S.A.); [email protected] (Z.F.); [email protected] (M.T.) 2 Department of Medical Biochemistry and Microbiology, Uppsala University, The Biomedical Center, Box 589, SE-751 23 Uppsala, Sweden; [email protected] (A.P.); [email protected] (G.P.) 3 Department of Anatomy, Physiology and Biochemistry, Swedish University of Agricultural Sciences, Box 7011, SE-75007 Uppsala, Sweden * Correspondence: [email protected]; Tel.: +46-(0)18-471-4532; Fax: +46-(0)18-471-4862 These authors contributed equally to this work. y Received: 29 July 2020; Accepted: 16 September 2020; Published: 17 September 2020 Abstract: Bone marrow-derived mast cells (BMMCs) are often used as a model system for studies of the role of MCs in health and disease. These cells are relatively easy to obtain from total bone marrow cells by culturing under the influence of IL-3 or stem cell factor (SCF). After 3 to 4 weeks in culture, a nearly homogenous cell population of toluidine blue-positive cells are often obtained. However, the question is how relevant equivalents these cells are to normal tissue MCs. By comparing the total transcriptome of purified peritoneal MCs with BMMCs, here we obtained a comparative view of these cells. -

The Thrombopoietin Receptor : Revisiting the Master Regulator of Platelet Production
This is a repository copy of The thrombopoietin receptor : revisiting the master regulator of platelet production. White Rose Research Online URL for this paper: https://eprints.whiterose.ac.uk/175234/ Version: Published Version Article: Hitchcock, Ian S orcid.org/0000-0001-7170-6703, Hafer, Maximillian, Sangkhae, Veena et al. (1 more author) (2021) The thrombopoietin receptor : revisiting the master regulator of platelet production. Platelets. pp. 1-9. ISSN 0953-7104 https://doi.org/10.1080/09537104.2021.1925102 Reuse This article is distributed under the terms of the Creative Commons Attribution (CC BY) licence. This licence allows you to distribute, remix, tweak, and build upon the work, even commercially, as long as you credit the authors for the original work. More information and the full terms of the licence here: https://creativecommons.org/licenses/ Takedown If you consider content in White Rose Research Online to be in breach of UK law, please notify us by emailing [email protected] including the URL of the record and the reason for the withdrawal request. [email protected] https://eprints.whiterose.ac.uk/ Platelets ISSN: (Print) (Online) Journal homepage: https://www.tandfonline.com/loi/iplt20 The thrombopoietin receptor: revisiting the master regulator of platelet production Ian S. Hitchcock, Maximillian Hafer, Veena Sangkhae & Julie A. Tucker To cite this article: Ian S. Hitchcock, Maximillian Hafer, Veena Sangkhae & Julie A. Tucker (2021): The thrombopoietin receptor: revisiting the master regulator of platelet production, Platelets, DOI: 10.1080/09537104.2021.1925102 To link to this article: https://doi.org/10.1080/09537104.2021.1925102 © 2021 The Author(s). -

Role of ADAM10 and ADAM17 in Regulating CD137 Function
International Journal of Molecular Sciences Article Role of ADAM10 and ADAM17 in Regulating CD137 Function Jana Seidel 1, Sinje Leitzke 1, Björn Ahrens 1, Maria Sperrhacke 1, Sucharit Bhakdi 2 and Karina Reiss 1,* 1 Department of Dermatology, University of Kiel, 24105 Kiel, Germany; [email protected] (J.S.); [email protected] (S.L.); [email protected] (B.A.); [email protected] (M.S.) 2 Independent Researcher, 24105 Kiel, Germany; [email protected] * Correspondence: [email protected] Abstract: Human CD137 (4-1BB), a member of the TNF receptor family, and its ligand CD137L (4-1BBL), are expressed on immune cells and tumor cells. CD137/CD137L interaction mediates bidirectional cellular responses of potential relevance in inflammatory diseases, autoimmunity and oncology. A soluble form of CD137 exists, elevated levels of which have been reported in patients with rheumatoid arthritis and various malignancies. Soluble CD137 (sCD137) is considered to represent a splice variant of CD137. In this report, however, evidence is presented that A Disintegrin and Metalloproteinase (ADAM)10 and potentially also ADAM17 are centrally involved in its generation. Release of sCD137 by transfected cell lines and primary T cells was uniformly inhibitable by ADAM10 inhibition. The shedding function of ADAM10 can be blocked through inhibition of its interaction with surface exposed phosphatidylserine (PS), and this effectively inhibited sCD137 generation. The phospholipid scramblase Anoctamin-6 (ANO6) traffics PS to the outer membrane and thus modifies ADAM10 function. Overexpression of ANO6 increased stimulated shedding, and hyperactive ANO6 led to maximal constitutive shedding of CD137. -

Cytokine Profiling in Myeloproliferative Neoplasms
cells Review Cytokine Profiling in Myeloproliferative Neoplasms: Overview on Phenotype Correlation, Outcome Prediction, and Role of Genetic Variants 1,2, , 1, 1 3 3 Elena Masselli * y , Giulia Pozzi y, Giuliana Gobbi , Stefania Merighi , Stefania Gessi , Marco Vitale 1,2,* and Cecilia Carubbi 1 1 Department of Medicine and Surgery, Anatomy Unit, University of Parma, Via Gramsci 14, 43126 Parma, Italy; [email protected] (G.P.); [email protected] (G.G.); [email protected] (C.C.) 2 University Hospital of Parma, AOU-PR, Via Gramsci 14, 43126 Parma, Italy 3 Department of Morphology, Surgery and Experimental Medicine, University of Ferrara, 44121 Ferrara, Italy; [email protected] (S.M.); [email protected] (S.G.) * Correspondence: [email protected] (E.M.); [email protected] (M.V.); Tel.: +39-052-190-6655 (E.M.); +39-052-103-3032 (M.V.) These authors contributed equally to this work. y Received: 1 September 2020; Accepted: 19 September 2020; Published: 21 September 2020 Abstract: Among hematologic malignancies, the classic Philadelphia-negative chronic myeloproliferative neoplasms (MPNs) are considered a model of inflammation-related cancer development. In this context, the use of immune-modulating agents has recently expanded the MPN therapeutic scenario. Cytokines are key mediators of an auto-amplifying, detrimental cross-talk between the MPN clone and the tumor microenvironment represented by immune, stromal, and endothelial cells. This review focuses on recent advances in cytokine-profiling of MPN patients, analyzing different expression patterns among the three main Philadelphia-negative (Ph-negative) MPNs, as well as correlations with disease molecular profile, phenotype, progression, and outcome. -

Engineering Strategies to Enhance TCR-Based Adoptive T Cell Therapy
cells Review Engineering Strategies to Enhance TCR-Based Adoptive T Cell Therapy Jan A. Rath and Caroline Arber * Department of oncology UNIL CHUV, Ludwig Institute for Cancer Research Lausanne, Lausanne University Hospital and University of Lausanne, 1015 Lausanne, Switzerland * Correspondence: [email protected] Received: 18 May 2020; Accepted: 16 June 2020; Published: 18 June 2020 Abstract: T cell receptor (TCR)-based adoptive T cell therapies (ACT) hold great promise for the treatment of cancer, as TCRs can cover a broad range of target antigens. Here we summarize basic, translational and clinical results that provide insight into the challenges and opportunities of TCR-based ACT. We review the characteristics of target antigens and conventional αβ-TCRs, and provide a summary of published clinical trials with TCR-transgenic T cell therapies. We discuss how synthetic biology and innovative engineering strategies are poised to provide solutions for overcoming current limitations, that include functional avidity, MHC restriction, and most importantly, the tumor microenvironment. We also highlight the impact of precision genome editing on the next iteration of TCR-transgenic T cell therapies, and the discovery of novel immune engineering targets. We are convinced that some of these innovations will enable the field to move TCR gene therapy to the next level. Keywords: adoptive T cell therapy; transgenic TCR; engineered T cells; avidity; chimeric receptors; chimeric antigen receptor; cancer immunotherapy; CRISPR; gene editing; tumor microenvironment 1. Introduction Adoptive T cell therapy (ACT) with T cells expressing native or transgenic αβ-T cell receptors (TCRs) is a promising treatment for cancer, as TCRs cover a wide range of potential target antigens [1]. -

CLINICAL RESEARCH PROJECT Protocol #11-H-0134 Drug Name: Eltrombopag (Promacta®) IND Number: 104,877 IND Holder: NHLBI OCD Date: January 2, 2019
CLINICAL RESEARCH PROJECT Protocol #11-H-0134 Drug Name: eltrombopag (Promacta®) IND number: 104,877 IND holder: NHLBI OCD Date: January 2, 2019 Title: A Pilot Study of a Thrombopoietin-receptor Agonist (TPO-R agonist), Eltrombopag, in Moderate Aplastic Anemia Patients Other Identifying Words: Hematopoiesis, autoimmunity, thrombocytopenia, neutropenia, anemia, stem cells, cytokine, Promacta® (eltrombopag) Protocol Principal Investigator: *Cynthia E. Dunbar, M.D., TSCBB, NHLBI (E) Medically and Scientifically Responsible Investigator: *Cynthia E. Dunbar, M.D., TSCBB, NHLBI (E) Associate Investigators: *Georg Aue, M.D., OCD, NHLBI (E) *Neal S. Young, M.D., Chief, HB, NHLBI (E) *André Larochelle, M.D., Ph.D., CMTB, NHLBI (E) David Young, M.D., TSCBB, NHLBI (E) Susan Soto, M.S.N., R.N., Research Nurse, OCD, NHLBI(E) Olga Rios, RN, Research Nurse, OCD, NHLBI (E) Evette Barranta, R.N, Research Nurse, OCD, NHLBI (E) Jennifer Jo Kyte, DNP, Research Nurse, OCD, NHLBI (E) Colin Wu, PhD, Biostatistician, OBR, NHLBI (E) Xin Tian, PhD, Biostatistician, OBR/NHLBI (E) *Janet Valdez, MS, PAC, OCD, NHLBI (E) *Jennifer Lotter, MSHS, PA-C., OCD, NHLBI (E) Qian Sun, Ph.D., DLM, CC (F) Xing Fan, M.D., HB, NHLBI (F) Non-NIH, Non-Enrolling Engaged Investigators: Thomas Winkler, M.D., NHLBI, HB (V)# # Covered under the NIH FWA Independent Medical Monitor: John Tisdale, MD, NHLBI, OSD 402-6497 Bldg. 10, 9N116 * asterisk denotes who can obtain informed consent on this protocol Subjects of Study: Number Sex Age-range 38 Either ≥ 2 years and weight >12 kg Project Involves Ionizing Radiation? No (only when medically indicated) Off-Site Project? No Multi center trial? No DSMB Involvement? Yes 11-H-0134 1 Cynthia E. -

Development and Validation of a Protein-Based Risk Score for Cardiovascular Outcomes Among Patients with Stable Coronary Heart Disease
Supplementary Online Content Ganz P, Heidecker B, Hveem K, et al. Development and validation of a protein-based risk score for cardiovascular outcomes among patients with stable coronary heart disease. JAMA. doi: 10.1001/jama.2016.5951 eTable 1. List of 1130 Proteins Measured by Somalogic’s Modified Aptamer-Based Proteomic Assay eTable 2. Coefficients for Weibull Recalibration Model Applied to 9-Protein Model eFigure 1. Median Protein Levels in Derivation and Validation Cohort eTable 3. Coefficients for the Recalibration Model Applied to Refit Framingham eFigure 2. Calibration Plots for the Refit Framingham Model eTable 4. List of 200 Proteins Associated With the Risk of MI, Stroke, Heart Failure, and Death eFigure 3. Hazard Ratios of Lasso Selected Proteins for Primary End Point of MI, Stroke, Heart Failure, and Death eFigure 4. 9-Protein Prognostic Model Hazard Ratios Adjusted for Framingham Variables eFigure 5. 9-Protein Risk Scores by Event Type This supplementary material has been provided by the authors to give readers additional information about their work. Downloaded From: https://jamanetwork.com/ on 10/02/2021 Supplemental Material Table of Contents 1 Study Design and Data Processing ......................................................................................................... 3 2 Table of 1130 Proteins Measured .......................................................................................................... 4 3 Variable Selection and Statistical Modeling ........................................................................................