Shared Leadership Underpinning of the MLCF
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
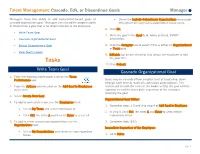
Manager Cascade, Edit, Or Discontinue Goal(S) in Workday
Talent Management: Cascade, Edit, or Discontinue Goals Manager Managers have the ability to add department-based goals or • Check the Include Subordinate Organizations to cascade cascade organization goal. Managers can also edit in-progress goals throughout all supervisory organization below yours. or discontinue a goal that is no longer relevant to the employee. 6. Click OK. • Write Team Goal 7. Write the goal in the Goal field. Add a detailed, SMART • Cascade Organizational Goal description. • Edit or Discontinue a Goal 8. Click the Category box to select if this is either an Organizational or Team goal. • View Team’s Goals 9. Editable will be pre-selected. This allows the employee to edit Tasks the goal title. 10. Click Submit. Write Team Goal Cascade Organizational Goal 1. From the Workday home page, click on the Team Performance app. Goals may be cascaded from a higher level of leadership, down through each level to reach all supervisory organizations. This 2. From the Actions column, click on the Add Goal to Employees section will include the steps of the leader writing the goal and the menu item. approval step of the immediate supervisor of the employee receiving the goal. 3. Select Create New Goal. Organizational Goal Writer: 4. To add to immediate team, use the Employees field: 1. Complete steps 1-3 and skip step 4 of Add Goal to Employee. • Select My Team and select individuals or 2. In step 5, click Ctrl, the letter A and Enter to select entire • Click Ctrl, the letter A and then hit Enter to select all. -

Chapter 6 – Group and Team Performance 90
Chapter 6 – Group and Team Performance 90 CHAPTER 6 – Group and Team Performance OBJECTIVES The major purpose of this chapter on group process and effectiveness is to introduce the student to ways to think about interacting groups so that they will become more effective members and leaders of them. Every student has had some experience with both social and task groups that they can call on as they study this topic. Our first objective in this chapter is to focus on how central these groups are to our lives. We also attempt to impress on the students that they will likely spend large proportions of their work hours in small group settings, because modern management appears to be making increasing use of teams or other small groups to solve problems, make decisions, and execute tasks. The next objective is to help student understand the many types of groups they may be involved with and how groups vary by purpose and organization. Another objective is to introduce students to a basic model of group effectiveness that includes influences from the environment within which the group operates. Environmental influences can have a critical impact on group effectiveness and the different types of influences are considered. At this point the chapter changes its focus to give more emphasis to internal group dynamics by covering such topics as cooperation and competition. Here, one objective is to introduce students to group development and the process by which groups become (or fail to become) mature. Another objective is to introduce the role of norms in influencing group member behavior. -

Team Leadership Styles
Team Leadership Styles Leadership Skills Team FME www.free-management-ebooks.com ISBN 978-1-62620-988-6 Copyright Notice © www.free-management-ebooks.com 2013. All Rights Reserved ISBN 978-1-62620-988-6 The material contained within this electronic publication is protected under International and Federal Copyright Laws and treaties, and as such any unauthorized reprint or use of this material is strictly prohibited. You may not copy, forward, or transfer this publication or any part of it, whether in elec- tronic or printed form, to another person, or entity. Reproduction or translation of any part of this work without the permission of the copy- right holder is against the law. Your downloading and use of this eBook requires, and is an indication of, your complete acceptance of these ‘Terms of Use.’ You do not have any right to resell or give away part, or the whole, of this eBook. TEAM LEADERSHIP STYLES Table of Contents Preface 2 Visit Our Website 3 Introduction 4 Team Examples 6 Development Team Example 7 Customer Support Team Example 9 Steering Team Example 10 Leadership Theories 13 Early Trait Theories 13 Leadership for Management 16 Transactional Leadership 17 Applied to the Team Examples 19 Transformational Leadership 22 Applied to the Team Examples 24 Situational Leadership® 26 Applied to the Team Examples 28 The Leadership Continuum 30 Applying this Style to the Team Examples 32 Summary 34 Other Free Resources 35 References 36 ISBN 978-1-62620-988-6 © www.free-management-ebooks.com 1 TEAM LEADERSHIP STYLES Preface This eBook has been written for managers who find themselves in a team leadership role. -

The Importance of Vertical and Shared Leadership Within New Venture Top Management Teams: Implications for the Performance of Startups☆ ⁎ Michael D
The Leadership Quarterly 17 (2006) 217–231 The importance of vertical and shared leadership within new venture top management teams: Implications for the performance of startups☆ ⁎ Michael D. Ensley a,1, Keith M. Hmieleski b,2, Craig L. Pearce c, a Rensselaer Polytechnic Institute, Lally School of Management and Technology, Troy, NY 12180-3590, USA b Texas Christian University, M. J. Neeley School of Business, Fort Worth, TX 76129, USA c Claremont Graduate University, Peter F. Drucker and Masatoshi Ito Graduate School of Management, Claremont Graduate University, Claremont, CA 91711, USA Abstract The current study investigated the relative influence of vertical versus shared leadership within new venture top management teams on the performance of startups using two different samples. Vertical leadership stems from an appointed or formal leader of a team (e.g., the CEO), whereas shared leadership is a form of distributed leadership stemming from within a team. Transformational, transactional, empowering, and directive dimensions of both vertical and shared leadership were examined. New venture performance was considered in terms of revenue growth and employee growth. The first sample was comprised of 66 top management teams of firms drawn from Inc. Magazine's annual list of America's 500 fastest growing startups. The seconded sample consisted of 154 top management teams of startups randomly drawn from Dun and Bradstreet, which compiles the most extensive database available for identifying relatively young American-based ventures. Both vertical and shared leadership were found to be highly significant predictors of new venture performance. Further, hierarchical regression analysis found the shared leadership variables to account for a significant amount of variance in new venture performance beyond the vertical leadership variables. -

Organizational Change and Development Chapter 12
Organizational Change and Development Chapter 12 ORGANIZATIONAL CHANGE AND DEVELOPMENT Introduction Change is a constant, a thread woven into the fabric of our personal and professional lives. Change occurs within our world and beyond -- in national and international events, in the physical environment, in the way organizations are structured and conduct their business, in political and socioeconomic problems and solutions, and in societal norms and values. As the world becomes more complex and increasingly interrelated, changes seemingly far away affect us. Thus, change may sometimes appear to occur frequently and randomly. We are slowly becoming aware of how connected we are to one another and to our world. Organizations must also be cognizant of their holistic nature and of the ways their members affect one another. The incredible amount of change has forced individuals and organizations to see “the big picture” and to be aware of how events affect them and vice versa. Organizational development (OD) is a field of study that addresses change and how it affects organizations and the individuals within those organizations. Effective organizational development can assist organizations and individuals to cope with change. Strategies can be developed to introduce planned change, such as team-building efforts, to improve organizational functioning. While change is a “given,” there are a number of ways to deal with change -- some useful, some not. Organizational development assists organizations in coping with the turbulent environment, both internally and externally, frequently doing so by introducing planned change efforts. Organizational development is a relatively new area of interest for business and the professions. While the professional development of individuals has been accepted and fostered by a number of organizations for some time, there is still ambiguity surrounding the term organizational development. -

Supported Employment Fidelity Review Manual
SUPPORTED EMPLOYMENT FIDELITY REVIEW MANUAL Deborah R. Becker Sarah J. Swanson Sandra L. Reese Gary R. Bond Bethany M. McLeman Copyright © 2008, 2015 by all original copyright holders. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, without the written permission of the rights holder. SUPPORTED EMPLOYMENT FIDELITY REVIEW MANUAL A companion guide to the evidence-based IPS Supported Employment Fidelity Scale Deborah R. Becker Sarah J. Swanson Sandra L. Reese Gary R. Bond Bethany M. McLeman Dartmouth Psychiatric Research Center Third Edition December, 2015 TABLE OF CONTENTS PREFACE .......................................................................................................................... iv INTRODUCTION .............................................................................................................. v Chapter 1: Introduction to IPS Supported Employment Fidelity .............................. 1 IPS Supported Employment Overview ........................................................................... 1 Overview of the IPS Supported Employment Fidelity Scale .......................................... 3 Sources of Information ............................................................................................... 5 What is Rated? ............................................................................................................ 5 Unit of Analysis ......................................................................................................... -

Groups & Teams
Organizational Behavior and Organizational Change Groups & Teams Roger N. Nagel Senior Fellow & Wagner Professor Lehigh University 1 CSE & Enterprise Systems Center Lehigh University Roger N. Nagel © 2006 Topics in this Presentation Why people join groups The Five-Stage Model of Group Development Group Structure: ¾ Conformity, Status, Cohesiveness Group - Decision Making e l e v e n t h e d i t i o n ¾ Group - Decision Making Techniques » Group think, Groupshift o r g a n i z a t i o n a l b e h a v i o r ¾ Interacting Groups ¾ Nominal Group Technique ¾ Brainstorming stephen p. robbins ¾ Electronic Meeting 2 Evaluating Group Effectiveness Why Have Teams Become So Popular? “Organizational“Organizational behavior” behavior” Team Versus Group: What’s the Difference EleventhEleventh Edition Edition ¾ Comparing Work Groups and Work Teams ByBy Steve Steve Robbins Robbins Types of Teams ISBNISBN 0-13-191435-9 0-13-191435-9 A Team-Effectiveness Model ReferenceReference Book Book Beware: Teams Aren’t Always the Answer 2 CSE & Enterprise Systems Center Lehigh University Roger N. Nagel © 2006 Groups A group is defined as two or more individuals ¾ Interacting and interdependent, ¾ who have come together to achieve particular objectives. Groups can be either formal or informal. Members similar or dissimilar 3 CSE & Enterprise Systems Center Lehigh University Roger N. Nagel © 2006 Why People Join Groups • Security • Status • Self-esteem • Affiliation • Power • Goal Achievement E X H I B I T 8–1 E X H I B I T 8–1 Page 239 Page 239 4 CSE & Enterprise Systems Center Lehigh University Roger N. -

Position-Specific Rugby Skills Handbook About This Handbook
POSITION-SPECIFIC RUGBY SKILLS HANDBOOK ABOUT THIS HANDBOOK Thank you for downloading the Ruck Science position-specifc rugby skills handbook. This handbook is designed for amateur rugby players, coaches and parents as a guide to creating tailored training programs that meet the needs of each individual position on a rugby team. The handbook will take readers through the specifc physical and technical demands of each position as well as the training associated with building the requisite skill set. We would like to use this opportunity to thank several organizations without whom this handbook would not have been possible. Firstly, the Canadian Rugby Union who created a similar guide in 2009. This version has drawn a lot of inspiration from that original work which was itself a derivative of a manual set up by the English Rugby Union. Secondly, the writing team of Tudor Bompa & Frederick Claro whose trans-formative work Periodization in Rugby was also published in 2009. “Periodization in Rugby” is, without a doubt, the most complete analysis of periodized training for amateur rugby players and should be essential reading for all rugby coaches who are working with young players. Sincerely, Tim Howard Founder Ruck Science TABLE OF CONTENTS 2. About this handbook 4. Physical preparation for rugby 5. Warming up 5. Cooling down 6. Key rugby skills 6. Healthy eating 7. Prop 15. Hooker 21. Lock 27. Flanker 36. Number 8 42. Scrumhalf 47. Flyhalf 52. Center 56. Wing 61. Fullback Riekert Hattingh SEATTLE SEAWOLVES RUGBY SHORTS WITH POCKETS The world’s most comfortable rugby shorts, with deep, strong pockets on both sides. -
Teams, Team Process, and Team Building
Loyola University Chicago Loyola eCommons School of Business: Faculty Publications and Other Works Faculty Publications 2014 Teams, Team Process, and Team Building James W. Bishop Dow Scott Loyola University Chicago, [email protected] Stephanie Maynard-Patrick Lei Wang Follow this and additional works at: https://ecommons.luc.edu/business_facpubs Part of the Business Administration, Management, and Operations Commons, and the Performance Management Commons Recommended Citation Bishop, James W.; Scott, Dow; Maynard-Patrick, Stephanie; and Wang, Lei. Teams, Team Process, and Team Building. Clinical Laboratory Management, 2nd Edition, , : 373-391, 2014. Retrieved from Loyola eCommons, School of Business: Faculty Publications and Other Works, http://dx.doi.org/10.1128/ 9781555817282.ch18 This Book Chapter is brought to you for free and open access by the Faculty Publications at Loyola eCommons. It has been accepted for inclusion in School of Business: Faculty Publications and Other Works by an authorized administrator of Loyola eCommons. For more information, please contact [email protected]. This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 3.0 License. © ASM Press 2014 18 Introduction Teams, Team Process, Definition of a Team Distinguishing Teams from Work Groups • Types and Classifications of Teams • Why Define a “Team” So and Team Building Precisely? Group Process and Teams James W. Bishop, K. Dow Scott, Guidelines for Choosing Whether To Have Teams Stephanie Maynard-Patrick, and Lei Wang Common -

Here Are Some Easy Starter Tips for Teaching the Game of Tchoukball to Your PE Students
Here are some easy starter tips for teaching the game of Tchoukball to your PE students • Don’t tell them they can score at either rebounder. At first tell your teams they can only score at the opposite end. This will get them used to moving the ball up and down the court. You can add the both frame rule down the road. • Remember the rules of 3: 3 sec to hold the ball, only three steps, and when you are attacking both ends you cannot throw at the same rebounder after 3 trys. • When there is a change of possession make sure there is a “reset” by the new team. A reset is done by touching the ball to the floor with both hands on the ball. This can be done anywhere; it does not have to be at the goal line. • Don’t allow students to guard, intercept or even get in the way of a student who is trying to throw or catch a ball. No blocking out, screening, standing in the way of the rebounder is allowed. The team without the ball actually must make a concentrated effort to stay out of the way of the offensive team. • Once the ball leaves the hand of the team trying to score, they must now make sure they are not interfering with the other team trying to catch their ball. Any interference here is a foul and loss of possession/no score. • Small sided games are the best….3-5 players on a team. You can have a third team rotate in after a score. -

Journal of Applied Psychology
Journal of Applied Psychology Initiating and Utilizing Shared Leadership in Teams: The Role of Leader Humility, Team Proactive Personality, and Team Performance Capability Chia-Yen (Chad) Chiu, Bradley P. Owens, and Paul E. Tesluk Online First Publication, September 12, 2016. http://dx.doi.org/10.1037/apl0000159 CITATION Chiu, C.-Y. (C.), Owens, B. P., & Tesluk, P. E. (2016, September 12). Initiating and Utilizing Shared Leadership in Teams: The Role of Leader Humility, Team Proactive Personality, and Team Performance Capability. Journal of Applied Psychology. Advance online publication. http:// dx.doi.org/10.1037/apl0000159 Journal of Applied Psychology © 2016 American Psychological Association 2016, Vol. 101, No. 10, 000 0021-9010/16/$12.00 http://dx.doi.org/10.1037/apl0000159 Initiating and Utilizing Shared Leadership in Teams: The Role of Leader Humility, Team Proactive Personality, and Team Performance Capability Chia-Yen (Chad) Chiu Bradley P. Owens University of South Australia Brigham Young University Paul E. Tesluk University at Buffalo, State University of New York The present study was designed to produce novel theoretical insight regarding how leader humility and team member characteristics foster the conditions that promote shared leadership and when shared leadership relates to team effectiveness. Drawing on social information processing theory and adaptive leadership theory, we propose that leader humility facilitates shared leadership by promoting leadership-claiming and leadership- granting interactions among team members. We also apply dominance complementary theory to propose that team proactive personality strengthens the impact of leader humility on shared leadership. Finally, we predict that shared leadership will be most strongly related to team performance when team members have high levels of task-related competence. -

Team Leadership
The Leadership Quarterly 12 (2001) 451–483 Team leadership Stephen J. Zaccaroa,*, Andrea L. Rittmana, Michelle A. Marksb aPsychology Department, George Mason University, 3064 David T. Langehall, 4400 University Drive, Fairfax, VA 22030-4444, USA bFlorida International University, Miami, FL, USA Abstract Despite the ubiquity of leadership influences on organizational team performance and the large literatures on leadership and team/group dynamics, we know surprisingly little about how leaders create and handle effective teams. In this article, we focus on leader–team dynamics through the lens of ‘‘functional leadership.’’ This approach essentially asserts that the leader’s main job is to do, or get done, whatever functions are not being handled adequately in terms of group needs. We explicate this functional leadership approach in terms of 4 superordinate and 13 subordinate leadership dimensions and relate these to team effectiveness and a range of team processes. We also develop a number of guiding propositions. A key point in considering such relationships is the reciprocal influence, whereby both leadership and team processes influence each other. D 2002 Elsevier Science Inc. All rights reserved. 1. Introduction Effective team performance derives from several fundamental characteristics (Zaccaro & Klimoski, in press). First, team members need to successfully integrate their individual actions. They have specific and unique roles, where the performance of each role contributes to collective success. This means that the causes of team failure may reside not only in member inability, but also in their collective failure to coordinate and synchronize their individual contributions. Team processes become a critical determinant of team performance, and often mediate the influences of most other exogenous variables.