An Overview of Thermal Infrared Imaging-Based Screenings During Pandemic Emergencies
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

What Do “Infrared Thermometers” Measure?
What do “infrared thermometers” measure? Overview These days, infrared (or “non-contact”) thermometers are popular items in hardware stores, auto parts stores, and stores that carry high-end cooking equipment. You point the thermometer at an object, and it reads the temperature. You can see how this could be useful to a chef or mechanic. But... What does such a thermometer actually measure? If you’re baking a potato, there’s a good chance that the reading will correspond to the surface temperature. But the truth is not always so simple — for example, if you’ve wrapped your potato in aluminum foil, you won’t see anything like the temperature of the spud itself! In the title, we’ve put “infrared thermometer” in quotes because this device doesn’t measure temperature directly; rather, temperature is inferred from a different measurement. So just what does the device measure? This is a good open question that you can ask your students to explore. Theory All matter is made of atoms, and all the atoms are in constant random motion. This is the molecular view of thermal energy. Atoms ,in turn, are composed of charged particles. And when you accelerate a charged particle (as occurs perpetually in the atomic motion associated with thermal energy), it emits electromagnetic waves. Does this mean that all objects will emit electromagnetic waves? Indeed it does. (Well, it does for any object with a temperature greater than absolute zero — that is, any object you’re apt to ever encounter.) Hotter objects emit more of this thermal radiation, objects at different temperatures emit different wavelengths, and some objects (metals, for instance) are pretty poor emitters. -

Thermal Imaging Guidebook for Industrial Applications
THERMAL IMAGING GUIDEBOOK FOR INDUSTRIAL APPLICATIONS An informative guide for the use of thermal imaging cameras in industrial applications 1 Content page 1. The thermal imaging camera and how it works 6 2. Why use thermal imaging? 8 3. Using thermal imaging for industrial applications 12 4. Choosing the right thermal imaging camera supplier 24 5. Thermal physics for industrial applications 26 6. Finding the best solution 30 7. How to carry out thermal inspections 42 This booklet is produced in close cooperation with the Infrared Training Centre (ITC). All images used are for illustrative purposes only. SPECIFICATIONS ARE SUBJECT TO CHANGE WITHOUT NOTICE © Copyright 2011, FLIR Systems AB. All other brand and product names are trademarks of their respective owners. 3 Introduction Ever since the first commercial thermal imaging camera was sold in 1965 for high voltage power line inspections, by what would later become FLIR Systems, the use of thermal imaging 1 cameras for industrial applications has been an important market segment for FLIR. Since then thermal imaging technology has evolved. Thermal imaging cameras have become compact systems that look just like a digital video camera or digital photo camera. They are easy to use and generate crisp real-time high-resolution images. Thermal imaging technology has become one of the most valuable diagnostic tools for industrial applications. By detecting anomalies that are usually invisible to the naked eye, thermal imaging allows corrective action to be taken before costly system failures occur. Thermal imaging cameras are a unique tool to determine when and where maintenance is needed, for electrical and mechanical installations tend to get hot before they fail. -

Digital Infrared Thermometer
Model #480742 DIGITAL INFRARED THERMOMETER CAREFULLY READ THROUGH THE ENTIRE OWNER’S MANUAL BEFORE OPERATING YOUR DIGITAL INFRARED THERMOMETER. KEEP MANUAL WITH IMPORTANT RECORDS FOR SAFETY INSTRUCTIONS, OPERATING PROCEDURES AND WARRANTY. Please retain these instructions for future reference. If you encounter any problems or difficulties, please contact our toll free Customer Service Department at: 1-800-423-3598 1431 VIA PLATA 1-310-522-9008 (California only) LONG BEACH, CA 90810-1462 www.alltradetools.com FOR CUSTOMER SERVICE 1-310-522-9066 Fax © Copyright 2004, Alltrade Tools LLC Rev.1 1-800-423-3598 SPECIFICATIONS: GENERAL Congratulations on your purchase of the Digital Infrared Thermometer! Your Digital Infrared Thermometer is fitted with optical filters that allow you to safely take infrared surface temperature Display 4 digit LCD display readings when contact with the object is not an option. Its convenient laser targeting and high Measurement Ranges -40˚C to 500˚C (-40˚F to 932˚F) with 0.1˚C (32.18˚F) resolution distance-to-spot ratio gives you the flexibility to take accurate temperatures of hard to read objects. Sample rate Approximately 1 second Laser power <1mW output at 675µm wave length. (Class II laser product) SAFETY & WARNINGS Storage Temperature -20˚C to 50˚C (-4˚F to 122˚F) The Digital Infrared Thermometer is a laser device and should be used with caution and care. Operating Temperature 0˚C to 50˚C (32˚F to 122˚F) Please observe the following guidelines when using this device. Operating Humidity Max. 80% • Infrared thermometers only measure surface temperature. Therefore when used in food applications, Power Supply One 9V battery (included) critical temperatures must be verified with an internal temperature-measuring device. -

Basics of Non Contact Temperature Measurement 2 Physical Basics
More Precision. Basics of non contact temperature measurement 2 Physical Basics With our eyes we see the world in visible light. Whereas visible light fills only a small part of the radiation spectrum, the invisible light covers most of the remaining spectral range. The radiation of invisible light carries much more additional information. The Infrared Temperature Measurement System Each body with a temperature above the absolute zero (-273.15°C = 0 Kelvin) emits an electromagnetic radiation from its surface, which is proportional to its intrinsic temperature. A part of this so-called intrinsic radiation is infrared radiation, which can be used to measure a body’s temperature. This radiation penetrates the atmosphere. With the help of a lens (input optics) the beams are focused on a detector element, which William Herschel (1738 - 1822) generates an electrical signal proportional to the radiation. The signal is amplified and, using successive digital signal processing, is transformed Discovery of the Infrared Radiation into an output signal proportional to the object temperature. The measu- Searching for new optical material William Herschel by chance found the ring value may be shown in a display or released as analog output signal, infrared radiation in 1800. He blackened the peak of a sensitive mercury which supports an easy connection to control systems of the process thermometer. This thermometer, a glass prism that led sun rays onto a ta- management. ble made his measuring arrangement. With this, he tested the heating of different colors of the spectrum. Slowly moving the peak of the blackened thermometer through the colors of the spectrum, he noticed the increas- ing temperature from violet to red. -
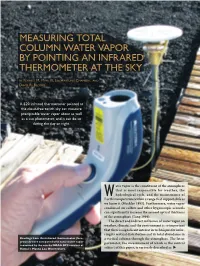
Measuring Total Column Water Vapor by Pointing an Infrared Thermometer at the Sky
MEASURING TOTAL COLUMN WATER VAPOR BY POINTING AN INFRARED THERMOMETER AT THE SKY BY FORREST M. MIMS III, LIN HARTUNG CHAMBERS, AND DAVID R. BROOKS A $20 infrared thermometer pointed at the cloud-free zenith sky can measure precipitable water vapor about as well as a sun photometer, and it can do so during the day or night. ater vapor is the constituent of the atmosphere that is most responsible for weather, the W hydrological cycle, and the maintenance of Earth’s temperature within a range that supports life as we know it (Mockler 1995). Furthermore, water vapor condensed on sulfate and other hygroscopic aerosols can significantly increase the aerosol optical thickness of the atmosphere (Tang 1996). The direct and indirect influence of water vapor on weather, climate, and the environment is so important that there is significant interest in techniques for infer- ring its vertical distribution and its total abundance in Readings from this infrared thermometer (fore- a vertical column through the atmosphere. The latter ground) were compared with total water vapor measured by the nearby NOAA GPS receiver at parameter, the measurement of which is the central Hawaii’s Mauna Loa Observatory. subject of this paper, is variously described as X total column water vapor, integrated water vapor heating of these sensors, and the wake effect of the (IWV), precipitable water (PW), and integrated ascending balloon. precipitable water (IPW). Each of these phrases speci- Precipitable water can also be measured by a fies the depth of liquid water that would result if all microwave radiometer tuned to frequencies emitted of the water vapor in a vertical column through the by liquid and gaseous water molecules (Liljegren atmosphere were brought to the surface at standard 1994). -

Infrared Temperature Measuring Instrument
testo-826-P01 16.08.2012 12:24 Seite 1 We measure it. Infrared temperature measuring instrument testo 826 Non-contact measurement of surface temperature, ideally °C suitable for the food sector 6:1 optics for fast and accurate measurement 1-point laser measurement spot marking Combined instrument with infrared and penetration measurement Two adjustable limit values Waterproof and robust thanks to dishwasher-safe protective cover TopSafe, according to protection class IP65 Hold function and display of min./max. values HACCP from every point of view: the testo 826 series has The advantages: just been optimized. A higher resolution thanks to the new • Always monitor, measure and document temperature processor ensures even more accurate measurement accurately, cleanly and quickly. results. This allows the temperature to be recorded to an • Fulfil HACCP regulations, and be able to provide proof at accuracy of 0.1 °C. The min./max. display shows the limit any time. values of the last measurement. You can measure and • Maintain the cold chain in storage and transport. monitor the temperature of the goods reliably and safely. • Reduce the quantities of spoiled goods and use resources efficiently. • Measuring instruments calibrated according to strict regulations. • Conform to HACCP as well as EN 13485. testo-826-P02 16.08.2012 12:55 Seite 2 testo 826 We measure it. Technical data General technical data testo 826-T2 Spectral range 8 to 14 μm Measurement rate 0,5 s testo 826-T2, infrared thermometer with 1 point Distance to 6:1 laser sighting, alarm function, incl. TopSafe and measurement spot wall/belt holder Emissivity 0,1 to 1 Meas. -

BASIC PRINCIPLES of Non-Contact Temperature Measurement
innovative infrared technology BASIC PRINCIPLES of Non-Contact Temperature Measurement Content Site Physical Basics ............................................................. 4 – 9 Emissivity and Temperature Measurement ............... 10 – 14 Optics, Sighting Techniques and Electronics ............. 15 – 18 Infrared Thermometers and Applications .................. 19 – 24 Thermal Imagers and Applications ............................ 25 – 31 Literature ........................................................................... 32 Appendix: Glossary ........................................................... 33 Appendix: Emissivity Table ........................................ 34 – 38 Appendix: Selection Criteria for IR temperature measurement devices .............................. 39 3 Physical Basics With our eyes we see the world in visible light. Whereas Physical Basics visible light fills only a small part of the radiation spectrum, the invisible light covers most of the remaining spectral range. The radiation of invisible light carries much more additional information. The Infrared Temperature Measurement System Each body with a temperature above the absolute zero (–273,15 °C = 0 Kelvin) emits an electromagnetic radiation from its surface, which is proportional to its intrinsic tempera- ture. A part of this so-called intrinsic radiation is infrared radiation, which can be used to measure a body’s tempera- ture. This radiation penetrates the atmosphere. With the help of a lens (input optics) the beams are focused on a detector -
Infrared Temperature Measuring Instrument (2-Channel)
testo-810-P01 04.10.2011 15:40 Seite 1 We measure it. Infrared temperature measuring instrument (2-channel) testo 810 Handy pocket-sized combi instrument for non-contact °C measurement of the surface temperature and air temperature measurement 1-point laser measurement point marking and 6:1 optics Hold-function, display of max./min. values and the difference between air and surface temperature Settable emissivity Display illumination Incl. protective cap for safe storage, wrist strap and beltholder Illustration 1:1 The testo 810 is a handy temperature measuring instrument Thanks to its handy design, the testo 810 is quickly to hand which measures air temperature, and simultaneously and easy to stow, for example in a trouser pocket. The surface temperature by infrared. For example, the infrared measurement is carried out with a 1-point laser temperature of a radiator, an air outlet or a window can be measurement spot marking and 6:1 optics. The emissivity easily and conveniently compared to the air temperature in can be individually set depending on the application, and the room. The difference between air and surface with the help of the min./max. function, the minimum and temperature is automatically displayed. maximum values are shown in the display. www.testo.com testo-810-P02 04.10.2011 15:41 Seite 2 testo 810 We measure it. Technical data / Accessories General technical data testo 810 Distance to 6:1 measurement spot testo 810; 2-channel temperature measuring Meas. spot marking 1-point laser instrument with infrared thermometer with laser spot marking and integrated NTC air Emissivity Adjustable 0.2 to 0.99 thermometer, incl. -

Pyrolaser Emissivity Measuring Infrared Thermometer Fundamental
Operating Experience with An Emissivity Measuring Laser Based Infrared Pyrometer Non Contact Infrared Thermometer Temperature Measurement International Test and Transducer Conference Sensors & Systems E. K. Mathews and G. J. Kilford Introduction: While in use in many industrial applications and research activities, the measurement of temperature utilizing infrared greatest deficiency is quite fundamental; IR thermometers measure radiance received from a target i.e. one variable, while integration of Planck’s law governing the relationship between the radiance and temperature requires knowledge of a second variable, the target surface emissivity. Heretofore, the solution has been a combination of operator estimates based on experience, or use of dual and multi-wavelength pyrometers, which sidestep the mathematical problem by ratioing-out the emissivity using two or more simultaneous measurements of the radiance. The assumptions here are that the surface is a grey body, with constant emissivity (e) or fixed ratios between emissivities at two or more wavelengths. In many industrial applications these assumptions are not valid. Emissivity varies with surface condition, temperature, wavelength and indeed, with time. Industrial processes have dynamic characteristics and the targets have varying properties; the simple emissivity assumptions are not valid. The second chronic error in industrial infrared temperature measurement is that caused by background radiation irradiance or energy reflected by the target to the measuring instrument. The instrument receives infrared energy from the target composed of the emitted energy plus that source by furnace walls or a combustion front and reflected by the target to the measuring instrument. We thus have a two-fold effect of target emissivity: Where (r ) is the target reflectivity and the subscript (l ) refers to wavelength. -

Comparison of Rectal and Infrared Thermometry Temperatures in Anesthetized Swine (Sus Scrofa)
Journal of the American Association for Laboratory Animal Science Vol 59, No 2 Copyright 2020 March 2020 by the American Association for Laboratory Animal Science Pages 221–225 Comparison of Rectal and Infrared Thermometry Temperatures in Anesthetized Swine (Sus scrofa) Kerrie L Farrar,1,* Amy E Field,3 Sarah L Norris,2 and Kenneth O Jacobsen1 Infrared thermometry (IRTM) is a noncontact method to measure temperature. The purpose of this study was to compare rectal temperature and IRTM in healthy anesthetized swine, with the hypothesis that IRTM would be an accurate, noninva- sive alternative for rectal temperature measurement. Two groups of female Yorkshire-cross swine (n = 14 and n = 12) were sedated with Tiletamine–zolazepam (0.5 mg/kg) for blood collection during a routine physical examination. While sedated, rectal temperatures were measured using a SureTemp Plus 690 (Welch Allyn) and IRTM measurements were taken using a FLIR E5 thermal imaging camera. The 2 anatomic sites used for thermography measurements were the area surrounding the eye and the neck at the base of the ear. The distance from the imaging camera and the animal during IRTM measurements was 24 to 32 inches, a distance that would allow camera access in a standard swine enclosure. The infrared imaging camera’s surface temperature measurement exhibited a proportional bias when compared with the rectal temperature. All rectal tem- perature measurements were between 98.7 °F to 101.3 °F, with a mean temperature of 100.4 °F. IRTM tended to underestimate rectal temperatures at lower values, and overestimate rectal temperatures at higher values by approximately (+) or (-) 0.8 °F of rectal temperature. -

Fibre Optic Coupled, Infrared Thermometers For
FIBRE OPTIC COUPLED, INFRARED THERMOMETERS FOR PROCESSES INCURRING HARSH CONDITIONS Andrew David Heeley Registration Number 150143161 This thesis is submitted in partial fulfilment of the requirements for the degree of Doctor of Philosophy The University of Sheffield Faculty of Engineering Department of Electronic and Electrical Engineering 18th December 2019 The template used to compile this thesis was produced by Malcolm Morgan and Kayla Friedman for the Centre for Sustainable Development, University of Cambridge, UK ⁘ “The socialism I believe in isn’t really politics. It is a way of living. It is humanity. I believe the only way to live and to be truly successful is by collective effort, with everyone working for each other, everyone helping each other and everyone having a share in the rewards at the end of the day. That might be asking a lot but it is the way I see football, the way I see life.” Bill Shankly ⁘ There are those who sow divisions and those who grow visions. Wisdom teaches us to live in the shelter of each other. ⁘ i DECLARATION I, Andrew David Heeley, confirm that this thesis is my own work and includes nothing that is the outcome of work done in collaboration except where specifically indicated in the text. I am aware of the University’s Guidance on the Use of Unfair Means (www.sheffield.ac.uk/ssid/unfair-means). This work has not been previously submitted, in part or whole, to any university for any degree or other qualification. Signed: A D Heeley Date: 18th December 2019 Andrew David Heeley Sheffield, UK ii FIBRE OPTIC COUPLED, INFRARED THERMOMETERS FOR PROCESSES INCURRING HARSH CONDITIONS ANDREW D HEELEY, DECEMBER 2019 ABSTRACT This study undertook the development and testing of fibre optic coupled infrared thermometers (IRTs) that could substitute for thermocouples in harsh conditions that would affect contact temperature measurements deleteriously. -

Basic Principles of Non-Contact Temperature Measurement
Basic Principles Of Non-Contact Temperature Measurement InnovatedInnovativeInnovative Infrared InfraredInfrared technology TechnologyTechnology 1 Innovative Infrared Technology 22 Inhalt Content 4-8 Physical Basics 9-11 Emissivity and Temperature Measurement 12-14 Optics, Sighting Techniques and Electronics 15-19 Infrared Thermometer and Applications 20-24 Thermal Imager and Applications 25 Literature 26 Appendix: Glossary 27-30 Appendix: Emissivity Table 31 Appendix: Selection Criteria for Infrared Thermometers Innovative Infrared Technology InnovatedInnovativewww.optris.com InfraredInfrared technologyTechnology 3 Physical Basics With our eyes we see the world in visible light. Whereas visible light fills only a small part of the radiation spectrum, the invisible light covers most of the remaining spectral range. The radiation of invisible light carries much more additional information. The Infrared Temperature Measurement System Each body with a temperature above the absolute zero (-273.15°C = 0 Kelvin) emits an electromagnetic radiation William Herschel (1738 - 1822) from its surface, which is proportional to its intrinsic tem- perature. A part of this so-called intrinsic radiation is inf- thermometer, a glass prism that led sun rays onto a table rared radiation, which can be used to measure a body’s made his measuring arrangement. With this, he tested temperature. This radiation penetrates the atmosphere. the heating of different colors of the spectrum. Slowly mo- With the help of a lens (input optics) the beams are fo- ving the peak of the blackened thermometer through the cused on a detector element, which generates an elec- colors of the spectrum, he noticed the increasing tempe- trical signal proportional to the radiation. The signal is rature from violet to red.