Gonsalves Declaration
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

PRO BONO NEWS July 2015
PRO BONO NEWS JULY 2015 Why Pro Bono Matters IN THIS ISSUE SOMETIMES, PRO BONO WORK offers an opportunity to make a profound Click on an article to jump to it. difference in an individual’s or family’s life, such as by helping a veteran Proud to Help Lead the Fight obtain long-overdue disability benefits, or securing asylum for a family for Marriage Equality fleeing persecution. page 2 In other instances, pro bono service can bring lasting benefits to Resolution of New York thousands, hundreds of thousands or even millions of people. Recently, City Jails Reform Case a Ropes & Gray was privileged to play a key role in three pro bono matters Pro Bono Victory with that kind of sweeping social impact. page 2 In April, Douglas Hallward-Driemeier, head of the firm’s appellate & Supreme Court practice, argued before the Supreme Court on behalf of the plaintiffs in the landmark Public Service Honored at marriage equality case that has just given our LGBT friends, family members, neighbors 12th Annual Pro Bono Awards and their families a right that should have been theirs all along. The court’s June 26 decision page 3 will go down in history with other iconic civil rights milestones and will benefit an untold Q&A: Securing Voting Rights number of people in the years to come. in Massachusetts A few days earlier in June, the resolution of a class-action lawsuit alleging a pattern and page 4 practice of excessive force against inmates at Rikers Island and other New York City jails, in violation of their Eighth Amendment rights, capped one of the firm’s most significantpro New Associates Embrace bono matters. -

(CA Bar 157750) [email protected] Eliz
Case 5:19-cv-01546-JGB-SHK Document 207 Filed 07/13/20 Page 1 of 17 Page ID #:4195 1 Timothy P. Fox (CA Bar 157750) [email protected] 2 Elizabeth Jordan* [email protected] 3 CIVIL RIGHTS EDUCATION AND ENFORCEMENT CENTER 4 1245 E. Colfax Avenue, Suite 400 5 Denver, CO 80218 Tel: (303) 757-7901 6 Fax: (303) 872-9072 7 Lisa Graybill* [email protected] Stuart Seaborn (CA Bar 198590) 8 Jared Davidson* [email protected] [email protected] Melissa Riess (CA Bar 295959) 9 SOUTHERN POVERTY LAW [email protected] CENTER DISABILITY RIGHTS ADVOCATES 10 201 St. Charles Avenue, Suite 2000 2001 Center Street, 4th Floor 11 New Orleans, Louisiana 70170 Berkeley, California 94704 Tel: (504) 486-8982 Tel: (510) 665-8644 12 Fax: (504) 486-8947 Fax: (510) 665-8511 13 14 Attorneys for Plaintiffs (continued on next page) 15 UNITED STATES DISTRICT COURT 16 CENTRAL DISTRICT OF CALIFORNIA 17 EASTERN DIVISION – RIVERSIDE 18 FAOUR ABDALLAH FRAIHAT, et al., Case No.: 19-cv-01546-JGB(SHKx) 19 Plaintiffs, Plaintiffs’ Reply Brief in Support of 20 v. Motion to Enforce the April 20, 21 U.S. IMMIGRATION AND CUSTOMS 2020 Preliminary Injunction Order 22 ENFORCEMENT, et al., Hearing Date: July 13, 2020 23 Defendants. Time: 2:00 pm Hon. Jesus G. Bernal 24 25 26 27 28 Case 5:19-cv-01546-JGB-SHK Document 207 Filed 07/13/20 Page 2 of 17 Page ID #:4196 1 William F. Alderman (CA Bar 47381) Mark Mermelstein (CA Bar 208005) [email protected] [email protected] 2 Jake Routhier (CA Bar 324452) ORRICK, HERRINGTON & [email protected] SUTCLIFFE LLP 3 ORRICK, HERRINGTON & 777 South Figueroa Street SUTCLIFFE LLP Suite 3200 4 405 Howard Street Los Angeles, CA 90017 5 San Francisco, CA 94105 Tel: (213) 629-2020 Tel: (415) 773-5700 Fax: (213) 612-2499 6 Fax: (415) 773-5759 Leigh Coutoumanos* 7 Michael W. -

United States District Court District of Connecticut
UNITED STATES DISTRICT COURT DISTRICT OF CONNECTICUT DAVID TUTTLE, Plaintiff, v. No. 3:17-cv-1507 (JAM) SCOTT SEMPLE, et al., Defendants. INITIAL REVIEW ORDER Plaintiff David Tuttle has filed this pro se complaint that principally alleges a violation of his rights under the Eighth Amendment while he was subject to solitary confinement for about one year at the Northern Correctional Institution in Connecticut. I think it is likely that defendants have qualified immunity, but rather than summarily dismissing the complaint at this time I will allow it to be served on defendants while also allowing plaintiff to file an amended complaint within 30 days if he believes that there are additional facts that would suffice to withstand a motion to dismiss on grounds of qualified immunity. BACKGROUND Plaintiff has filed this lawsuit against the Connecticut Department of Correction’s Commissioner Scott Semple, Warden Nick Rodriguez, Health Services Administrator Brian Liedel, Dr. Mark Frayne, and Dr. Gerard Gagne. Plaintiff sues each of these defendants for money damages in their personal and official capacity, and plaintiff also seeks injunctive relief. The following facts are assumed to be true solely for purposes of my initial evaluation of the adequacy of the allegations in the second amended complaint. Plaintiff was originally convicted and sentenced in Massachusetts before being transferred in 2012 to Connecticut in accordance with an arrangement under an interstate corrections compact. In late January 2017, 1 he was transferred from the Corrigan -
FROM BLUEPRINT to BUILDING Lifting the Torch for Multilingual Students in New York State
JANIE TANKARD CARNOCK FROM BLUEPRINT TO BUILDING Lifting the Torch for Multilingual Students in New York State NOVEMBER 2016 About the Authors About New America Janie Tankard Carnock is a program New America is committed to renewing American politics, associate with the Education Policy prosperity, and purpose in the Digital Age. We generate big program at New America. She is a ideas, bridge the gap between technology and policy, and member of the DLL National Work Group, curate broad public conversation. We combine the best of where she provides research and analysis a policy research institute, technology laboratory, public on policies related to language learners. forum, media platform, and a venture capital fund for ideas. We are a distinctive community of thinkers, writers, researchers, technologists, and community activists who believe deeply in the possibility of American renewal. Acknowledgments Find out more at newamerica.org/our-story. This work would not be possible without generous support from the Heising-Simons and McKnight Foundations. Research took place over eight months, and benefited from the advice, counsel, and wisdom of many individuals. About the Education Policy Program New America colleagues Conor Williams, Amaya Garcia, Lisa Guernsey, Kaylan Connally, and Lindsey Tepe provided New America’s Education Policy program uses original considerable editorial insight. Kristina Rodriguez and research and policy analysis to solve the nation’s critical Sammi Wong provided research and editing support. education problems, serving as a trusted source of Sabrina Detlef copyedited. A number of other individuals objective analysis and innovative ideas for policymakers, shared valuable knowledge, including Andrea Honigsfeld, educators, and the public at large. -

1 United States District Court for the Southern District of Mississippi Northern Division Brittany Waddell, Roger Ewing, Tony Sm
Case 3:20-cv-00340-TSL-RHW Document 6 Filed 05/25/20 Page 1 of 6 UNITED STATES DISTRICT COURT FOR THE SOUTHERN DISTRICT OF MISSISSIPPI NORTHERN DIVISION BRITTANY WADDELL, ROGER EWING, TONY SMITH, DANIEL HATTEN, DOUGLASS TRIPLETT, ERIK LEWIS, BOB HENDERSON, THOMAS HOLDER, and JAMARCUS DAVIS, individually and on behalf of a class of all others similarly situated, Civil Action No. 3:20-cv-340-TSL-RHW Plaintiffs, v. TOMMY TAYLOR, in his official capacity as Interim Commissioner of the Mississippi ORAL ARGUMENT REQUESTED Department of Corrections; RON KING, in his official capacity as Superintendent of Central Mississippi Correctional Facility; and JOE ERRINGTON, in his official capacity as Superintendent of South Mississippi Correctional Institution, Defendants. PLAINTIFFS’ MOTION FOR A TEMPORARY RESTRAINING ORDER AND PRELIMINARY INJUNCTION 1 Case 3:20-cv-00340-TSL-RHW Document 6 Filed 05/25/20 Page 2 of 6 1. Plaintiffs respectfully request that the Court enter a temporary restraining order and preliminary injunction requiring the Defendants to effectively implement COVID-19 prevention and management protocols consistent with established standards of care for infection control and CDC guidelines. Pursuant to Local Rule 7(b)(6)(A), Plaintiffs respectfully request oral argument on this motion. 2. The Plaintiffs, who have brought this action on behalf of themselves and others similarly situated, are Brittany Waddell, Roger Ewing, Tony Smith, Daniel Hatten, Douglass Triplett, Erik Lewis, Bob Henderson, Thomas Holder, and Jamarcus Davis. They are residents of Mississippi’s two largest prisons, Central Mississippi Correctional Facility (CMCF) and South Mississippi Correctional Institution (SMCI), home to nearly 6,000 residents, combined.1 3. -
Gonsalves Reply Declaration
Case 1:20-cv-10617-WGY Document 33-5 Filed 04/02/20 Page 1 of 18 IN THE UNITED STATES DISTRICT COURT FOR THE DISTRICT OF MASSACHUSETTS Maria Alejandra Celimen Savino, et al., Petitioners-Plaintiffs, Civil Action No. 1:20-cv-10617- WGY v. Steven J. Souza, Respondent-Defendant. REPLY DECLARATION OF GREGG GONSALVES I, Gregg S. Gonsalves, upon my personal knowledge, and in accordance with 28 U.S.C. § 1746, declare as follows: 1. I am an epidemiologist at the Yale School of Medicine and School of Public Health. I have worked at the schools of medicine and public health since 2017. I submit this to respond to the information provided by the Defendant in his opposition to the motion for temporary restraining order and as a supplement to my prior declaration in ths case. See ECF No. 12-2. I understand that my CV was inadvertently not filed with my first declaration and so I attach it here as Exhibit A. 2. I have reviewed the relevant filings in this matter, Savino v. Souza, including the statements and declarations of Plaintiffs, putative Plaintiffs’ class members and their families, lawyers with familiarity with the Bristol County House of Correction and immigration facilities (“BCHOC”), as well as arguments and declarations filed by Defendant. Dkt. Nos. 1-4, 1-5, 12-2, 12-3, 12-4, 12-5, 12-6, 12-7, 12-8, 12-9, 20-3, 20-4, 26, 26-1, 26-2, 26-3. 3. The following represents my expert opinion as to several of Defendant’s claims based on my review of these filings and drawing on my knowledge and experience. -

RFA Summit & State Education Fellowship Convening Agenda
RFA Summit & State Education Fellowship Convening Agenda October 2-4, 2019 Eaton Hotel,1201 K Street, NW, Washington, DC Contents Convening At-A-Glance……………………………………….………………………………..2 State Education Fellowship Convening Agenda………………………………...………….. 3 Convening Logistics………………………………………………………...…………………..9 Contact Information…………………………………………………………….……………...14 Speaker Biographies…………………………………………………………………………..20 Convening At-A-Glance Date Agenda Item Start Time Location Welcome 5:30 PM Wild Days Wednesday, Reception Eaton Hotel Rooftop October 2 1201 K Street NW Washington, DC 20005 Breakfast 8:00 AM Salon (2nd Floor) Eaton Hotel 1201 K Street NW Washington, DC 20005 2019 Summit What 8:45 AM Beverly Snow Ballroom (2nd Floor) Works to Advance Eaton Hotel Economic Mobility 1201 K Street NW Washington, DC 20005 Lunch - The Story 12:00 PM Beverly Snow Ballroom (2nd Floor) of Economic Eaton Hotel Mobility in America 1201 K Street NW Washington, DC 20005 Thursday, October 3 Concurrent 2:15 PM Various - See Summit Agenda Workshops State Education 6:30 PM Ghibellina Agency & 1610 14th St NW Workforce Washington, DC 20009 Reception and Dinner Breakfast & 8:00 AM Salon (2nd Floor) State Standard of Eaton Hotel Excellence Launch 1201 K Street NW Event Washington, DC 20005 Friday, State Education 9:45 AM Crystal Room (1st Floor) October 4 Agency Fellowship Eaton Hotel Convening 1201 K Street NW Washington, DC 20005 Adjourn 3:30 PM Travel to airport Please see transportation details below 2 Results for America Summit 2019 & State Education Fellowship Convening Agenda October 2-4, 2019 Eaton Hotel, 1201 K Street, NW, Washington, DC 20005 Wednesday, October 2, 2019 5:30 - 7:30 pm Welcome Reception Eaton Hotel Rooftop - Wild Days Note: There will not be a formal Fellows dinner this evening. -
2016-17 NORTH TEXAS MEN's GOLF Men's Golf
2016-17 NORTH TEXAS MEN'S GOLF FACT AND RECORDS BOOK men's golf North Texas Athletics Department 1301 S. Bonnie Brae Denton, TX 76207 Office: (940) 565-2662 Shipping Address - Use this for overnight - FED EX / UPS 1251 South Bonnie Brae Shipping Dock Denton, TX 76207 Mailing Address - US Postal Service ONLY 1155 Union Circle #311397 Denton, TX 76203 www.meangreensports.com Credits: the North Texas Media Relations Department Photography: Rick Yeatts Mean Green Mission Statement * To Promote and monitor the educational achievement and personal growth of student-athletes, emphasizing that their education- al growth and development is the primary purpose of intercollegiate athletics * To conduct an athletics program that protects and enhances the physical and educational welfare of student-athletes * To provide fair and equitable opportunity for all student-athletes and staff participating in intercollegiate sport activities, regard- less of gender or ethnicity * To promote the principles of good sportsmanship and honesty in compliance with the University of North Texas, state, NCAA and conference regulations * To conduct a competitive athletics program that promotes faculty, staff, student and community affiliation with the University of North Texas * To serve the community through public service and outreach activities which positively reflect on the University of North Texas and promote good will in the community. TABLE OF CONTENTS Men’s Golf Quick Facts 2 PROFILES University Information Head Coach .................................................. -

The Ethics Corner First We Get You Through Law School
Year 2000: We'reHere.NowWhat? The ethics Corner First We Get You Through Law School. .. Then We Get You Through The Bar Exam! Gilbert Law Summaries Legalines Over 4 Million Copies Sold BAR/BRI Bar Review Relied On By Over 500,000 Lawyers ©rJJ!Jbr1 GROUP Our Only Mission Is Test Preparation Call Toll Free 1-888-3BARBRI or visit our web site at http.//www.barbri.com Juris Vol. 33, No. 1 • Winter 1999 You are young, my son, and as the years Staff go by, time will change and even reverse Editor-in-Chief many of your present opinions. Nick Rodriguez-Cayro Refrain therefore awhile from setting yourself Executive Editor up as a judge of the highest matters. Maureen Jordan Plato Managing Editor Matthew Clark • Senior Editor In thisISsue Gianni Floro Production Editor Maureen McQuillan Editorial: A Word from the Weary Assistant Executive Editors by Nick Rodriguez-Cayro ............ ... ................................................. .... ......... pg. 2 Annary Aytch Julie Gentry Repressed Memory and False Memory Syndrome: Nancy Koerbel Current Scien tific and Legal Perspectives Christi Neroni by Douglas Harhai ........... .................... ......... .. .............................................. pg. 3 Assistant Senior Editors Leslie Britton The Internet and the First Amendment: Douglas Harhai Bridgett Langer Regulations and Standards by Eliana Carrelli .................... .............................................. ................... ... pg. 10 Assistant Managing Editors Leah Lewandowski Patrick Dougherty The ABCs of Avoiding Malpractice -

West Virginia Power Game Notes
WEST VIRGINIA POWER GAME NOTES South Atlantic League - Class-A affiliate of the Seattle Mariners since 2019 - 601 Morris St. Suite 201- Charleston, WV 25301 - 304-344-2287 - www.wvpower.com - Media Contact: David Kahn WEST VIRGINIA POWER (25-26, 62-59) at DELMARVA SHOREBIRDS (32-18, 80-39) Game: 122 (Road: 63 [30-32]) | August 14, 2019 | Arthur W. Perdue Stadium | Salisbury, Md. Radio: The Jock 1300 and 1340 AM - wvpower.com Airtime: 6:45 P.M. THE PITCHING MATCH-UP: RHP Devin Sweet (7-4, 2.89 ERA) vs. RHP Gray Fenter (6-2, 1.88 ERA) Sweet: Has won his last four decisions dating back to July 6 at Lexington Fenter: Boasts a 1.50 ERA in two games (one start) vs. WV; Has tossed 6 IP with 11 K and 0 BB POWER FALLS IN BACK-AND-FORTH AFFAIR 10-9: Julio Rodriguez smacked his first career grand slam and CURRENT ROAD TRIP tallied a career-high six RBI, but West Virginia dropped the middle match of their series with the Delmarva Shorebirds, Record: 4-2 Season Highs 10-9, Tuesday evening at Arthur W. Perdue Stadium. The Power got on the board first in the opening frame, as Ryan Batting Statistics Batting Statistics: Ramiz and Matt Sanders started the ballgame with back-to-back singles before Austin Shenton brought in a run on AVG: .228 (46-for-202) AVG: .362 (25-for-69) a groundout later in the stanza to make it 1-0. Delmarva answered immediately in the home half, taking advantage AB: 202 AB: 248 of a shaky Ryne Inman, who only lasted two-thirds of an inning and gave up three runs on one hit and five walks. -

Of Medical Experts
Tribunal Estadual do Rio de Janeiro Ministério Público e Defensoria Pùblica do Estado do Rio de Janeiro, Petitioners-Plaintiffs, v. Matter of Ação Civil Pública #0087229-92.2020.8.19.0001 Estado do Rio de Janeiro, Município do Rio de Janeiro e Associação Filantrópica Nova Esperança (Pronto Socorro Geral Hamilton Agostinho), Respondents-Defendants. OPINION OF MEDICAL EXPERTS GREGG GONSALVES, PH.D., JASON ANDREWS, M.D., TED COHEN, M.D., M.P.H., D.P.H., JULIO CRODA, M.D., ALBERT KO, M.D., JOSÉ ROBERTO LAPA E SILVA, M.D., PH.D., MARY PETRONE, KATHARINE WALTER, PH.D., MSC. 1. We, Gregg Gonsalves, Jason Andrews, Ted Cohen, Julio Croda, Albert Ko, José Roberto Lapa e Silva, Mary Petrone and Katharine Walter, hereby declare under penalty of perjury, that the following is true and correct to the best of our knowledge: RELEVANT BACKGROUND AND QUALIFICATIONS Gregg Gonsalves, Ph.D., Assistant Professor in Epidemiology of Microbial Diseases; Associate Professor of Law and Research Scholar in Law Yale School of Medicine, Yale Law School 2. I am an Assistant Professor in Epidemiology of Microbial Diseases at the Yale School of Medicine and an Associate Professor of Law and Research Scholar in Law at Yale Law School. I co-direct the Yale Law School/Yale School of Public Health Global Health Justice Partnership. I was the Co-Director of the Yale Law School/Yale School of Public Health/Yale Medical School Collaboration on Research Integrity and Transparency and the Co-Faculty Director of Global Health Studies at Yale College until May 2020. Among others, I also have held appointments at Harvard Medical School, the Institut Pasteur, and the University of Cape Town. -
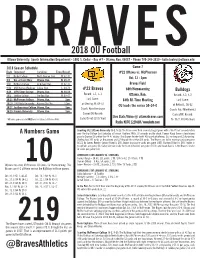
Overall Defensive Stats File:///C:/Daktronics/Dakstats Football/Sdefense 1.Html
BRAVES2018 OU Football Ottawa University® Sports Information Department - 1001 S. Cedar - Box #7 - Ottawa, Kan. 66067 - Phone 785-248-2610 - [email protected] 2018 Season Schedule Game 7 Date Opponent Location Time/Result #22 Ottawa vs. McPherson 9/1 Bethel College North Newton, Kan. W, 42-12 Oct. 13 - 1pm 9/8 Uni. of Saint Mary Ottawa, Kan. W, 29-27 9/15 Bethany College Lindsborg, Kan. W, 42-35 Braves Field 9/22 #14 Kansas Wesleyan Salina, Kan. L, 24-70 #22 Braves 88th Homecoming 9/29 #RV Tabor College Ottawa, Kan. W, 34-14 Bulldogs Record: 5-1, 5-1 10/6 Sterling College Sterling, Kan. W, 48-47 Ottawa, Kan. Record: 3-2, 3-2 10/13 McPherson College Ottawa, Kan. 1pm Last Game: 84th All-Time Meeting Last Game: 10/20 #RV Avila University Kansas City, Mo. 12pm at Sterling, W, 48-47 OU leads the series 59-24-0 at Bethel L, 56-42 10/27 Southwestern College Ottawa, Kan. 1pm Coach: Kent Kessinger Coach: Paul Mierkiewicz 10/10 Friends University Ottawa, Kan. 1pm Career/OU Record: Career/MC Record: Live Stats/Video @ ottawabraves.com *All home games are in BOLD and are played at Braves Field Same/93-65 (15th Year) 76-93/7-30 (4th Year) Radio: KOFO 1220 AM / www.kofo.com Scouting #22 Ottawa University (5-1, 5-1): The Braves won their second straight game with a 48-47 last second victory A Numbers Game over Sterling College last Saturday at Smisor Stadium. With 1.8 seconds on the clock, Connor Kaegi threw a touchdown pass to Darrion Dillard for the 48-47 victory.