Immune Response Dysfunction in Chronic Lymphocytic Leukemia: Dissecting Molecular Mechanisms and Microenvironmental Conditions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ENSG Gene Encodes Effector TCR Pathway Costimulation Inhibitory/Exhaustion Synapse/Adhesion Chemokines/Receptors
ENSG Gene Encodes Effector TCR pathway Costimulation Inhibitory/exhaustion Synapse/adhesion Chemokines/receptors ENSG00000111537 IFNG IFNg x ENSG00000109471 IL2 IL-2 x ENSG00000232810 TNF TNFa x ENSG00000271503 CCL5 CCL5 x x ENSG00000139187 KLRG1 Klrg1 x ENSG00000117560 FASLG Fas ligand x ENSG00000121858 TNFSF10 TRAIL x ENSG00000134545 KLRC1 Klrc1 / NKG2A x ENSG00000213809 KLRK1 Klrk1 / NKG2D x ENSG00000188389 PDCD1 PD-1 x x ENSG00000117281 CD160 CD160 x x ENSG00000134460 IL2RA IL-2 receptor x subunit alpha ENSG00000110324 IL10RA IL-10 receptor x subunit alpha ENSG00000115604 IL18R1 IL-18 receptor 1 x ENSG00000115607 IL18RAP IL-18 receptor x accessory protein ENSG00000081985 IL12RB2 IL-12 receptor x beta 2 ENSG00000186810 CXCR3 CXCR3 x x ENSG00000005844 ITGAL CD11a x ENSG00000160255 ITGB2 CD18; Integrin x x beta-2 ENSG00000156886 ITGAD CD11d x ENSG00000140678 ITGAX; CD11c x x Integrin alpha-X ENSG00000115232 ITGA4 CD49d; Integrin x x alpha-4 ENSG00000169896 ITGAM CD11b; Integrin x x alpha-M ENSG00000138378 STAT4 Stat4 x ENSG00000115415 STAT1 Stat1 x ENSG00000170581 STAT2 Stat2 x ENSG00000126561 STAT5a Stat5a x ENSG00000162434 JAK1 Jak1 x ENSG00000100453 GZMB Granzyme B x ENSG00000145649 GZMA Granzyme A x ENSG00000180644 PRF1 Perforin 1 x ENSG00000115523 GNLY Granulysin x ENSG00000100450 GZMH Granzyme H x ENSG00000113088 GZMK Granzyme K x ENSG00000057657 PRDM1 Blimp-1 x ENSG00000073861 TBX21 T-bet x ENSG00000115738 ID2 ID2 x ENSG00000176083 ZNF683 Hobit x ENSG00000137265 IRF4 Interferon x regulatory factor 4 ENSG00000140968 IRF8 Interferon -

Intrinsic and Extrinsic Mechanisms for B-Cell Lymphoma Development and Progression Studied by Global Gene Expression Profiling
From the Department of Laboratory Medicine Karolinska Institutet, Stockholm, Sweden INTRINSIC AND EXTRINSIC MECHANISMS FOR B-CELL LYMPHOMA DEVELOPMENT AND PROGRESSION STUDIED BY GLOBAL GENE EXPRESSION PROFILING Gustav Arvidsson Stockholm 2019 All previously published papers were reproduced with permission from the publisher. Published by Karolinska Institutet. Printed by Universitetsservice US-AB © Gustav Arvidsson, 2019 ISBN 978-91-7831-518-5 Intrinsic and extrinsic mechanisms for B-cell lymphoma development and progression studied by global gene expression profiling THESIS FOR DOCTORAL DEGREE (Ph.D.) By Gustav Arvidsson Principal Supervisor: Opponent: Professor Anthony Wright Professor Mikael Sigvardsson Karolinska Institutet Lund University Department of Laboratory Medicine Department of Laboratory Medicine Clinical Research Center Division of Molecular Haematology Co-supervisor: Examination Board: Professor Birgitta Sander Professor Lars-Gunnar Larsson Karolinska Institutet Karolinska Institutet Department of Laboratory Medicine Department of Microbiology, Tumor and Cell Division of Pathology Biology Associate Professor Ingrid Glimelius Uppsala University Department of Immunology, Genetics and Pathology Associate Professor Fredrik Öberg Uppsala University Department of Immunology, Genetics and Pathology For E and E ABSTRACT Mantle cell lymphoma (MCL) is a rare hematopoietic malignancy characterized by frequent relapses and poor survival, partly due to minimal residual disease, whereby a subset of malignant cells, harbored in protective niches, survive treatment. In vitro and ex vivo experiments have shown that MCL cells can be rescued from apoptosis through interactions with non-malignant cells such as stromal cells. The present thesis investigates the effect that extrinsic microenvironmental interactions may exert on MCL cells and discuss the presumptive role of these as well as intrinsic mechanisms in the development and progression of lymphomas. -

Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse
Welcome to More Choice CD Marker Handbook For more information, please visit: Human bdbiosciences.com/eu/go/humancdmarkers Mouse bdbiosciences.com/eu/go/mousecdmarkers Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse CD3 CD3 CD (cluster of differentiation) molecules are cell surface markers T Cell CD4 CD4 useful for the identification and characterization of leukocytes. The CD CD8 CD8 nomenclature was developed and is maintained through the HLDA (Human Leukocyte Differentiation Antigens) workshop started in 1982. CD45R/B220 CD19 CD19 The goal is to provide standardization of monoclonal antibodies to B Cell CD20 CD22 (B cell activation marker) human antigens across laboratories. To characterize or “workshop” the antibodies, multiple laboratories carry out blind analyses of antibodies. These results independently validate antibody specificity. CD11c CD11c Dendritic Cell CD123 CD123 While the CD nomenclature has been developed for use with human antigens, it is applied to corresponding mouse antigens as well as antigens from other species. However, the mouse and other species NK Cell CD56 CD335 (NKp46) antibodies are not tested by HLDA. Human CD markers were reviewed by the HLDA. New CD markers Stem Cell/ CD34 CD34 were established at the HLDA9 meeting held in Barcelona in 2010. For Precursor hematopoetic stem cell only hematopoetic stem cell only additional information and CD markers please visit www.hcdm.org. Macrophage/ CD14 CD11b/ Mac-1 Monocyte CD33 Ly-71 (F4/80) CD66b Granulocyte CD66b Gr-1/Ly6G Ly6C CD41 CD41 CD61 (Integrin b3) CD61 Platelet CD9 CD62 CD62P (activated platelets) CD235a CD235a Erythrocyte Ter-119 CD146 MECA-32 CD106 CD146 Endothelial Cell CD31 CD62E (activated endothelial cells) Epithelial Cell CD236 CD326 (EPCAM1) For Research Use Only. -

Human NK Cells with the 2B4 Receptor Inhibits Self-Killing of the Association of MHC Class I Proteins
The Association of MHC Class I Proteins with the 2B4 Receptor Inhibits Self-Killing of Human NK Cells This information is current as Gili Betser-Cohen, Saar Mizrahi, Moran Elboim, Osnat of September 27, 2021. Alsheich-Bartok and Ofer Mandelboim J Immunol 2010; 184:2761-2768; Prepublished online 17 February 2010; doi: 10.4049/jimmunol.0901572 http://www.jimmunol.org/content/184/6/2761 Downloaded from References This article cites 39 articles, 14 of which you can access for free at: http://www.jimmunol.org/content/184/6/2761.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 27, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2010 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology The Association of MHC Class I Proteins with the 2B4 Receptor Inhibits Self-Killing of Human NK Cells Gili Betser-Cohen, Saar Mizrahi, Moran Elboim, Osnat Alsheich-Bartok, and Ofer Mandelboim The killing activity of NK cells is carried out by several activating NK receptors, which includes NKp46, NKp44, NKp30, NKp80, NKG2D, and 2B4. -

Tools for Cell Therapy and Immunoregulation
RnDSy-lu-2945 Tools for Cell Therapy and Immunoregulation Target Cell TIM-4 SLAM/CD150 BTNL8 PD-L2/B7-DC B7-H1/PD-L1 (Human) Unknown PD-1 B7-1/CD80 TIM-1 SLAM/CD150 Receptor TIM Family SLAM Family Butyrophilins B7/CD28 Families T Cell Multiple Co-Signaling Molecules Co-stimulatory Co-inhibitory Ig Superfamily Regulate T Cell Activation Target Cell T Cell Target Cell T Cell B7-1/CD80 B7-H1/PD-L1 T cell activation requires two signals: 1) recognition of the antigenic peptide/ B7-1/CD80 B7-2/CD86 CTLA-4 major histocompatibility complex (MHC) by the T cell receptor (TCR) and 2) CD28 antigen-independent co-stimulation induced by interactions between B7-2/CD86 B7-H1/PD-L1 B7-1/CD80 co-signaling molecules expressed on target cells, such as antigen-presenting PD-L2/B7-DC PD-1 ICOS cells (APCs), and their T cell-expressed receptors. Engagement of the TCR in B7-H2/ICOS L 2Ig B7-H3 (Mouse) the absence of this second co-stimulatory signal typically results in T cell B7-H1/PD-L1 B7/CD28 Families 4Ig B7-H3 (Human) anergy or apoptosis. In addition, T cell activation can be negatively regulated Unknown Receptors by co-inhibitory molecules present on APCs. Therefore, integration of the 2Ig B7-H3 Unknown B7-H4 (Mouse) Receptors signals transduced by co-stimulatory and co-inhibitory molecules following TCR B7-H5 4Ig B7-H3 engagement directs the outcome and magnitude of a T cell response Unknown Ligand (Human) B7-H5 including the enhancement or suppression of T cell proliferation, B7-H7 Unknown Receptor differentiation, and/or cytokine secretion. -

2017 American College of Rheumatology/American Association
Arthritis Care & Research Vol. 69, No. 8, August 2017, pp 1111–1124 DOI 10.1002/acr.23274 VC 2017, American College of Rheumatology SPECIAL ARTICLE 2017 American College of Rheumatology/ American Association of Hip and Knee Surgeons Guideline for the Perioperative Management of Antirheumatic Medication in Patients With Rheumatic Diseases Undergoing Elective Total Hip or Total Knee Arthroplasty SUSAN M. GOODMAN,1 BRYAN SPRINGER,2 GORDON GUYATT,3 MATTHEW P. ABDEL,4 VINOD DASA,5 MICHAEL GEORGE,6 ORA GEWURZ-SINGER,7 JON T. GILES,8 BEVERLY JOHNSON,9 STEVE LEE,10 LISA A. MANDL,1 MICHAEL A. MONT,11 PETER SCULCO,1 SCOTT SPORER,12 LOUIS STRYKER,13 MARAT TURGUNBAEV,14 BARRY BRAUSE,1 ANTONIA F. CHEN,15 JEREMY GILILLAND,16 MARK GOODMAN,17 ARLENE HURLEY-ROSENBLATT,18 KYRIAKOS KIROU,1 ELENA LOSINA,19 RONALD MacKENZIE,1 KALEB MICHAUD,20 TED MIKULS,21 LINDA RUSSELL,1 22 14 23 17 ALEXANDER SAH, AMY S. MILLER, JASVINDER A. SINGH, AND ADOLPH YATES Guidelines and recommendations developed and/or endorsed by the American College of Rheumatology (ACR) are intended to provide guidance for particular patterns of practice and not to dictate the care of a particular patient. The ACR considers adherence to the recommendations within this guideline to be volun- tary, with the ultimate determination regarding their application to be made by the physician in light of each patient’s individual circumstances. Guidelines and recommendations are intended to promote benefi- cial or desirable outcomes but cannot guarantee any specific outcome. Guidelines and recommendations developed and endorsed by the ACR are subject to periodic revision as warranted by the evolution of medi- cal knowledge, technology, and practice. -

CD48 Is Critically Involved in Allergic Eosinophilic Airway Inflammation
CD48 Is Critically Involved in Allergic Eosinophilic Airway Inflammation Ariel Munitz,1 Ido Bachelet,1 Fred D. Finkelman,2 Marc E. Rothenberg,3 and Francesca Levi-Schaffer1,4 1Department of Pharmacology, School of Pharmacy, Faculty of Medicine, Hebrew University of Jerusalem, Jerusalem, Israel; 2Department of Medicine, University of Cincinnati College of Medicine, Cincinnati, Ohio; 3Division of Allergy and Immunology, Department of Pediatrics, Cincinnati Children’s Hospital Medical Center, University of Cincinnati College of Medicine, Cincinnati, Ohio; and 4David R. Bloom Center for Pharmacology, Hebrew University of Jerusalem, Jerusalem, Israel Rationale: Despite ongoing research, the molecular mechanisms con- trolling asthma are still elusive. CD48 is a glycosylphosphatidylinositol- AT A GLANCE COMMENTARY anchored protein involved in lymphocyte adhesion, activation, and costimulation. Although CD48 is widely expressed on hematopoi- Scientific Knowledge on the Subject etic cells and commonly studied in the context of natural killer and CD48 is an activation molecule able to facilitate various cytotoxic T cell functions, its role in helper T cell type 2 settings cellular activities. Its role in asthma is unknown. has not been examined. Objectives: To evaluate the expression and function of CD48, CD2, and 2B4 in a murine model of allergic eosinophilic airway inflammation. What This Study Adds to the Field Methods: Allergic eosinophilic airway inflammation was induced by CD48 is upregulated in experimental asthma. Anti-CD48– ovalbumin (OVA)–alum sensitization and intranasal inoculation of based therapies may be useful for asthma and perhaps OVA or, alternatively, by repeated intranasal inoculation of Aspergil- various allergic diseases. lus fumigatus antigen in wild-type, STAT (signal transducer and acti- vator of transcription)-6–deficient, and IL-4/IL-13–deficient BALB/c mice. -

Receptor-Arrestin Interactions: the GPCR Perspective
biomolecules Review Receptor-Arrestin Interactions: The GPCR Perspective Mohammad Seyedabadi 1,2 , Mehdi Gharghabi 3, Eugenia V. Gurevich 4 and Vsevolod V. Gurevich 4,* 1 Department of Toxicology & Pharmacology, Faculty of Pharmacy, Mazandaran University of Medical Sciences, Sari 48471-93698, Iran; [email protected] 2 Pharmaceutical Sciences Research Center, Faculty of Pharmacy, Mazandaran University of Medical Sciences, Sari 48167-75952, Iran 3 Department of Cancer Biology and Genetics, The Ohio State University Wexner Medical Center, Columbus, OH 43210, USA; [email protected] 4 Department of Pharmacology, Vanderbilt University, Nashville, TN 37232, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-615-322-7070; Fax: +1-615-343-6532 Abstract: Arrestins are a small family of four proteins in most vertebrates that bind hundreds of different G protein-coupled receptors (GPCRs). Arrestin binding to a GPCR has at least three functions: precluding further receptor coupling to G proteins, facilitating receptor internalization, and initiating distinct arrestin-mediated signaling. The molecular mechanism of arrestin–GPCR interactions has been extensively studied and discussed from the “arrestin perspective”, focusing on the roles of arrestin elements in receptor binding. Here, we discuss this phenomenon from the “receptor perspective”, focusing on the receptor elements involved in arrestin binding and empha- sizing existing gaps in our knowledge that need to be filled. It is vitally important to understand the role of receptor elements in arrestin activation and how the interaction of each of these elements with arrestin contributes to the latter’s transition to the high-affinity binding state. A more precise knowledge of the molecular mechanisms of arrestin activation is needed to enable the construction of arrestin mutants with desired functional characteristics. -

B Cell Subsets in Autoimmune Disease B Cell Subsetsb Cell in Autoimmune Disease
Thesis for doctoral degree (Ph.D.) 2018 Thesis for doctoral degree (Ph.D.) 2018 (Ph.D.) degree doctoral Thesis for B cell subsets in autoimmune disease B cell subsets in autoimmune disease B cell in autoimmune subsets Katrin Habir Katrin Habir From DEPARTMENT OF MEDICINE Karolinska Institutet, Stockholm, Sweden B CELL SUBSETS IN AUTOIMMUNE DISEASE Katrin Habir Stockholm 2018 All previously published papers were reproduced with permission from the publisher. Published by Karolinska Institutet. Printed by Printed by Eprint AB 2018 © Katrin Habir, 2018 ISBN 978-91-7676-900-3 B CELL SUBSETS IN AUTOIMMUNE DISEASE THESIS FOR DOCTORAL DEGREE (Ph.D.) AKADEMISK AVHANDLING som för avläggande av medicine doktorsexamen vid Karolinska Institutet offentligen försvaras i CMM Lecture Hall, L8:00, Center for Molecular Medicine (CMM), Karolinska Universitetssjukhuset, Solna. Friday February 2nd 2018 at 09.00 by Katrin Habir Principal Supervisor: Opponent: Dr. Stephen Malin Associate Professor Bengt Johansson Lindbom Karolinska Institutet Lunds Universitet Department of Medicine Department of Experimental Medical Science Division of Cardiovascular Medicine Division of Adaptive Immunity Co-supervisors: Examination Board: Professor Gunilla Karlsson Hedestam Professor Birgitta Heyman Karolinska Institutet Uppsala Universitet Department of Microbiology, Tumor and Cell Department of Medical Biochemistry and Biology Microbiology Division of Microbiology-Immunology Professor Dan Grandér Karolinska Institutet Associate Professor Lisa Westerberg Department of Oncology-Pathology Karolinska Institutet Department of Microbiology, Tumor and Cell Biology Associate Professor Angela Silveira Karolinska Institutet Department of Medicine Division of Cardiovascular Medicine “We still do not know one thousandth of one percent of what nature has revealed to us.” Albert Einstein THIS THESIS IS DEDICATED TO MY BELOVED ONES ABSTRACT B lymphocytes are a type of white blood cells, belonging to the adaptive arm of the immune system and involved in creating immunological memory. -

Advanced Age Increases Immunosuppression in the Brain and Decreases Immunotherapeutic Efficacy in Subjects with Glioblastoma
Author Manuscript Published OnlineFirst on June 16, 2020; DOI: 10.1158/1078-0432.CCR-19-3874 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. RESEARCH ARTICLE Advanced Age Increases Immunosuppression in the Brain and Decreases Immunotherapeutic Efficacy in Subjects with Glioblastoma Authors: Erik Ladomersky1, Lijie Zhai1, Kristen L. Lauing1, April Bell1, Jiahui Xu2, Masha Kocherginsky2, Bin Zhang3,4, Jennifer D. Wu5, Joseph R. Podojil4, Leonidas C. Platanias3,6, Aaron Y. Mochizuki7, Robert M. Prins8, Priya Kumthekar9, Jeffrey J. Raizer9, Karan Dixit9, Rimas V. Lukas9, Craig Horbinski1,10, Min Wei11, Changyou Zhou11, Graham Pawelec12, Judith Campisi13,14, Ursula Grohmann15, George C. Prendergast16, David H. Munn17, Derek A. Wainwright1,5,7,8 Affiliations: 1Department of Neurological Surgery, 2Department of Preventive Medicine-Biostatistics, 3Department of Medicine-Hematology/Oncology, 4Department of Microbiology- Immunology, 5Department of Urology, 6Department of Biochemistry and Molecular Genetics, 9Department of Neurology, 10Department of Pathology, Northwestern University Feinberg School of Medicine, Chicago, USA. 7Department of Neurology and Neurological Sciences, Stanford University, Stanford, USA. 8Department of Neurosurgery, David Geffen School of Medicine, University of California, Los Angeles, USA. 11BeiGene, Zhong-Guan-Cun Life Science Park, Changping District, Beijing, China. 12Department of Immunology, University of Tübingen, Tübingen, Germany. 13Buck Institute for Research on Aging, Novato, CA, USA. 14Lawrence Berkeley National Laboratory, Berkeley, CA, USA. 15Department of Experimental Medicine, University of Perugia, Perugia, Italy. 16Lankenau Institute for Medical Research, Wynnewood, PA, USA. 17Georgia Cancer Center, Augusta, GA, USA. Running Title: Aging and brain immunosuppression of GBM immunity Keywords: Senescence, neuroimmunology, immunotherapy, brain tumor, IDO COI: Min Wei and Changyou Zhou possess financial interests and are paid employees of BeiGene, Ltd. -

Supplementary Table 1: Adhesion Genes Data Set
Supplementary Table 1: Adhesion genes data set PROBE Entrez Gene ID Celera Gene ID Gene_Symbol Gene_Name 160832 1 hCG201364.3 A1BG alpha-1-B glycoprotein 223658 1 hCG201364.3 A1BG alpha-1-B glycoprotein 212988 102 hCG40040.3 ADAM10 ADAM metallopeptidase domain 10 133411 4185 hCG28232.2 ADAM11 ADAM metallopeptidase domain 11 110695 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 195222 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 165344 8751 hCG20021.3 ADAM15 ADAM metallopeptidase domain 15 (metargidin) 189065 6868 null ADAM17 ADAM metallopeptidase domain 17 (tumor necrosis factor, alpha, converting enzyme) 108119 8728 hCG15398.4 ADAM19 ADAM metallopeptidase domain 19 (meltrin beta) 117763 8748 hCG20675.3 ADAM20 ADAM metallopeptidase domain 20 126448 8747 hCG1785634.2 ADAM21 ADAM metallopeptidase domain 21 208981 8747 hCG1785634.2|hCG2042897 ADAM21 ADAM metallopeptidase domain 21 180903 53616 hCG17212.4 ADAM22 ADAM metallopeptidase domain 22 177272 8745 hCG1811623.1 ADAM23 ADAM metallopeptidase domain 23 102384 10863 hCG1818505.1 ADAM28 ADAM metallopeptidase domain 28 119968 11086 hCG1786734.2 ADAM29 ADAM metallopeptidase domain 29 205542 11085 hCG1997196.1 ADAM30 ADAM metallopeptidase domain 30 148417 80332 hCG39255.4 ADAM33 ADAM metallopeptidase domain 33 140492 8756 hCG1789002.2 ADAM7 ADAM metallopeptidase domain 7 122603 101 hCG1816947.1 ADAM8 ADAM metallopeptidase domain 8 183965 8754 hCG1996391 ADAM9 ADAM metallopeptidase domain 9 (meltrin gamma) 129974 27299 hCG15447.3 ADAMDEC1 ADAM-like, -
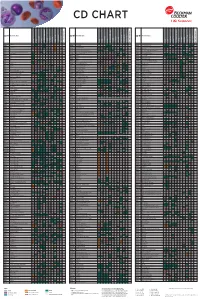
Flow Reagents Single Color Antibodies CD Chart
CD CHART CD N° Alternative Name CD N° Alternative Name CD N° Alternative Name Beckman Coulter Clone Beckman Coulter Clone Beckman Coulter Clone T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells CD1a T6, R4, HTA1 Act p n n p n n S l CD99 MIC2 gene product, E2 p p p CD223 LAG-3 (Lymphocyte activation gene 3) Act n Act p n CD1b R1 Act p n n p n n S CD99R restricted CD99 p p CD224 GGT (γ-glutamyl transferase) p p p p p p CD1c R7, M241 Act S n n p n n S l CD100 SEMA4D (semaphorin 4D) p Low p p p n n CD225 Leu13, interferon induced transmembrane protein 1 (IFITM1). p p p p p CD1d R3 Act S n n Low n n S Intest CD101 V7, P126 Act n p n p n n p CD226 DNAM-1, PTA-1 Act n Act Act Act n p n CD1e R2 n n n n S CD102 ICAM-2 (intercellular adhesion molecule-2) p p n p Folli p CD227 MUC1, mucin 1, episialin, PUM, PEM, EMA, DF3, H23 Act p CD2 T11; Tp50; sheep red blood cell (SRBC) receptor; LFA-2 p S n p n n l CD103 HML-1 (human mucosal lymphocytes antigen 1), integrin aE chain S n n n n n n n l CD228 Melanotransferrin (MT), p97 p p CD3 T3, CD3 complex p n n n n n n n n n l CD104 integrin b4 chain; TSP-1180 n n n n n n n p p CD229 Ly9, T-lymphocyte surface antigen p p n p n