Beyond Meatless, the Health Effects of Vegan Diets: Findings from the Adventist Cohorts
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Spiritual Disciplines of Early Adventists Heather Ripley Crews George Fox University, [email protected]
Digital Commons @ George Fox University Doctor of Ministry Theses and Dissertations 2-1-2016 Spiritual Disciplines of Early Adventists Heather Ripley Crews George Fox University, [email protected] This research is a product of the Doctor of Ministry (DMin) program at George Fox University. Find out more about the program. Recommended Citation Crews, Heather Ripley, "Spiritual Disciplines of Early Adventists" (2016). Doctor of Ministry. Paper 139. http://digitalcommons.georgefox.edu/dmin/139 This Dissertation is brought to you for free and open access by the Theses and Dissertations at Digital Commons @ George Fox University. It has been accepted for inclusion in Doctor of Ministry by an authorized administrator of Digital Commons @ George Fox University. For more information, please contact [email protected]. GEORGE FOX UNIVERSITY SPIRITUAL DISCIPLINES OF EARLY ADVENTISTS A DISSERTATION SUBMITTED TO THE FACULTY OF GEORGE FOX EVANGELICAL SEMINARY IN CANDIDACY FOR THE DEGREE OF DOCTOR OF MINISTRY LEADERSHIP AND SPIRITUAL FORMATION BY HEATHER RIPLEY CREWS PORTLAND, OREGON FEBRUARY 2016 Copyright © 2016 by Heather Ripley Crews All rights reserved. ii ABSTRACT The purpose of this dissertation is to explore the Biblical spirituality of the early Adventist Church in order to apply the spiritual principles learned to the contemporary church. Though it is God who changes people, the early Adventists employed specific spiritual practices to place themselves in His presence. Research revealed five main spiritual disciplines that shaped the Advent leaders and by extension the church. The first is Bible study: placing the Holy Scriptures as the foundation for all beliefs. The second is prayer: communication and communion with God. -

The Lifestyle and Prevalence of Vegetarianism in Seventh-Day Adventist Hispanics
Andrews University Digital Commons @ Andrews University Master's Theses Graduate Research 2013 The Lifestyle and Prevalence of Vegetarianism in Seventh-day Adventist Hispanics Maribel Hidalgo Andrews University Follow this and additional works at: https://digitalcommons.andrews.edu/theses Recommended Citation Hidalgo, Maribel, "The Lifestyle and Prevalence of Vegetarianism in Seventh-day Adventist Hispanics" (2013). Master's Theses. 10. https://digitalcommons.andrews.edu/theses/10 This Thesis is brought to you for free and open access by the Graduate Research at Digital Commons @ Andrews University. It has been accepted for inclusion in Master's Theses by an authorized administrator of Digital Commons @ Andrews University. For more information, please contact [email protected]. Thank you for your interest in the Andrews University Digital Library of Dissertations and Theses. Please honor the copyright of this document by not duplicating or distributing additional copies in any form without the author’s express written permission. Thanks for your cooperation. ABSTRACT THE LIFESTYLE AND PREVALENCE OF VEGETARIANISM IN SEVENTH-DAY ADVENTIST HISPANICS by Maribel Hidalgo Chair: Winston J. Craig ABSTRACT OF GRADUATE STUDENT RESEARCH Thesis Andrews University School of Health Professions Title: THE LIFESTYLE AND PREVALENCE OF VEGETARIANISM IN SEVENTH- DAY ADVENTIST HISPANICS Name of the researcher: Maribel Hidalgo Name and degree of chair: Winston J. Craig, Ph.D. Date completed: July 2013 Problem Hispanics are disproportionately affected by chronic diseases and are a growing and significant population. There is minimal research regarding the lifestyle of the Seventh-day Adventists (SDA) among the Hispanic community. The purpose of this cross-sectional descriptive study was to ascertain the lifestyle, health status, eating and physical activity habits of the SDA Hispanics from part of the Midwest. -

The God Who Hears Prayer Inside Illinoisillinois Members Focus News on the Web in This Issue / Telling the Stories of What God Is Doing in the Lives of His People
JUNE/JULY 2020 THE GOD WHO HEARS PRAYER ILLINOIS MEMBERS ILLINOIS FOCUS INSIDE NEWS ON THE WEB IN THIS ISSUE / TELLING THE STORIES OF WHAT GOD IS DOING IN THE LIVES OF HIS PEOPLE FEATURES Visit lakeunionherald.org for 14 Illinois — Camp Akita more on these and other stories By Mary Claire Smith Wisconsin’s Adventist Community Service volunteers made much needed 16 tie- and elastic-strapped masks for facilities and individuals. They were Download the Herald to your Indiana — Timber Ridge Camp asked to make masks for a 300-bed facility By Charlie Thompson in Pennsylvania which had experienced 38 mobile device! Just launch your PERSPECTIVES deaths due to the virus. camera and point it at the QR code. President's Perspective 4 18 (Older model devices may require Lest We Forget 8 downloading a third party app.) Conversations with God 9 Michigan — Camp Au Sable On Tuesday, May 5, the Michigan So, how’s your world? I remember Conference Executive Committee voted Conexiones 11 By Bailey Gallant my grandparents telling me about the to close the Adventist Book Centers One Voice 42 in Lansing, Berrien Springs and Cicero old days in North Dakota. One day I 20 (Indiana). They are exploring options to was walking through the Watford city EVANGELISM continue supplying printed material in cemetery where my great-grandfather Wisconsin — Camp Wakonda more efficient ways. Sharing Our Hope 10 Melchior was buried. I noticed that By Kristin Zeismer Telling God’s Stories 12 Follow us at lakeunionherald so many of the tombstones were Partnership With God 41 As part of its Everyone Counts, dated 1918, the year of the Spanish flu 22 Everyone Matters theme for the year, pandemic. -

Health Consequences of Vegetarian Diets
© Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR SALE OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION CHAPTER 2 © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT HealthFOR SALE Consequences OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION of Vegetarian Diets © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR SALE OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR SALE OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION Populations consuming vegetarian and semi-vegetarian diets have lower rates of several chronic diseases that typically plague Western countries, including heart disease, hypertension, diabetes, and certain cancers. This is true of vegetarians living in Western countries and of populations consuming© Jones plant-based & Bartlett diets in developingLearning, countries. LLC Migration studies indicate© these Jones differences & Bartlett Learning, LLC are dueNOT to environmental FOR SALE factors. OR TheDISTRIBUTION incidence of heart disease and many cancersNOT increases FOR when SALE OR DISTRIBUTION people from countries where plant-based diets are consumed relocate to countries with diets pre- dominantly based on animal products. Similarly, when people in developing countries become more affluent and begin to add more animal products to their diet, rates of chronic disease increase.1,2 © Jones & BartlettMuch of theLearning, available information LLC about health effects ©of Jonesvegetarian & diets Bartlett comes fromLearning, two LLC NOT FOR largeSALE prospective OR DISTRIBUTION epidemiologic studies. The Adventist HealthNOT Study FOR (AHS)-1 SALE is ORa cohort DISTRIBUTION of 34,192 California Seventh-day Adventists (SDAs) that began in 1974–1976. The European Pro- spective Investigation into Cancer and Nutrition-Oxford (EPIC-Oxford) in the United Kingdom has 65,429 participants and oversampled for vegetarians. -

Local MP Worships at Tottenham
Local MP worships at Tottenham n 23 June, Tottenham Church held a special recognition service in which they paid tribute to members of the Ochurch and the community. Among the dignitaries present were representatives from the local fire and police services and a number of community leaders. David Lammy, local MP, paid tribute to the church and charged everyone to continue the good work being done. He commented on the warmth of the church and recognised its value as a good place for young people to learn right from wrong. He mentioned five things necessary to build any successful family or church: education, employment, parenting, aspiration and community. He presented awards and posed for photos with those who received them. In his sermon, Pastor Perry encouraged the church to say ‘thank you’ to all the unseen heroes that are a part of our lives, but also pointed out that, although we may not always be thanked here on Earth, there is a reward for us in Heaven. All of this, combined with parading Pathfinders and good music, made the day a great success. COMMUNICATION TEAM 2 editorial 3 Fancy being published? ‘Murray, Murray, Murray . .’. Centre court This macro picture of a spotted long - throbbed. Wimbledon has echoed loudly for horn beetle was taken by decades, but never like this. The crowd factor Whitnell Anderson. Andy was serving for the match of his life Julian Hibbert Editor Please keep M– for Olympic gold and this country’s honour! sending in your photos Powerful first serves, deft backhand top for Megapixels of creation . -
Adventist Health and Healing Adventist Journey
06 20 INSPIRATION & INFORMATION FOR NORTH AMERICA INCLUDED Share the story of Adventist Health and Healing Adventist Journey AdventHealth is sharing the legacy and stories of the Seventh-day Adventist Contents 04 Feature 11 NAD Newsbriefs Loving People—Beyond Church with our 80,000 team members the Dentist’s Chair through a series of inspirational videos and other resources. 08 NAD Update 13 Perspective Breath of Life Revival Leads to On the Same Team More Than 15,000 Baptisms My Journey As I reflect on my journey, I recognize that God doesn’t promise that it’s going to be an easy path or an enjoyable path. Sometimes there are struggles and trials and hardships. But Join us in the journey. looking back, I realize that each one of those has strengthened Watch the videos and learn more at: my faith, strengthened my resolve, to trust in Him more and AdventHealth.com/adventisthealthcare more every day. Visit vimeo.com/nadadventist/ajrandygriffin for more of Griffin’s story. GETTING TO KNOW MEMBER SERIES ADVENTISTS | TEAM MEMBER SERIE TEA M GETTING TO KNOW ADVENTISTS | TEAM MEMBER SERIES S GETTING TO KNOW ADVENTISTS | Adventist Education RANDY GRIFFIN, Adventist Health Care Worldwide INTRODUCTION Getting to Know Adventists The Seventh-day Adventist Church operates the largest Protestant education system in the world, with more than 8,000 schools in more than 100 countries. With the belief that education is more than just intellectual growth, Adventist education Cicero, Indiana, GETTING TO KNOW ADVENTISTS | TEAM MEMBER SERIES INTRODUCTION also focuses on physical, social, and spiritual Driven by the desire to bring restoration to a broken development. -
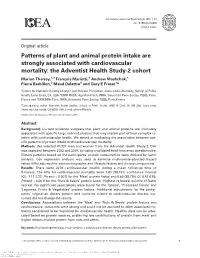
Patterns of Plant and Animal Protein Intake Are Strongly Associated With
International Journal of Epidemiology, 2018, 1–10 doi: 10.1093/ije/dyy030 Original article Original article Patterns of plant and animal protein intake are strongly associated with cardiovascular mortality: the Adventist Health Study-2 cohort Marion Tharrey,1,2 Franc¸ois Mariotti,2 Andrew Mashchak,1 Pierre Barbillon,3 Maud Delattre3 and Gary E Fraser1* 1Center for Nutrition, Healthy Lifestyle and Disease Prevention, Loma Linda University, School of Public Health, Loma Linda, CA, USA, 2UMR PNCA, AgroParisTech, INRA, Universite´ Paris-Saclay, 75005, Paris, France and 3UMR MIA-Paris, INRA, Universite´ Paris-Saclay, 75005, Paris, France *Corresponding author. Adventist Health Studies, School of Public Health, 24951 N Circle Dr, NH 2033, Loma Linda University, Loma Linda, CA 92350, USA. E-mail: [email protected] Editorial decision 29 January 2018; Accepted 6 February 2018 Abstract Background: Current evidence suggests that plant and animal proteins are intimately associated with specific large nutrient clusters that may explain part of their complex re- lation with cardiovascular health. We aimed at evaluating the association between spe- cific patterns of protein intake with cardiovascular mortality. Methods: We selected 81 337 men and women from the Adventist Health Study-2. Diet was assessed between 2002 and 2007, by using a validated food frequency questionnaire. Dietary patterns based on the participants’ protein consumption were derived by factor analysis. Cox regression analysis was used to estimate multivariate-adjusted hazard ratios (HRs) adjusted for sociodemographic and lifestyle factors and dietary components. Results: There were 2276 cardiovascular deaths during a mean follow-up time of 9.4 years. The HRs for cardiovascular mortality were 1.61 [98.75% confidence interval (CI), 1.12 2.32; P-trend < 0.001] for the ‘Meat’ protein factor and 0.60 (98.75% CI, 0.42 0.86; P-trend < 0.001) for the ‘Nuts & Seeds’ protein factor (highest vs lowest quintile of factor scores). -

Five Steps to Health in America
A Health Policy Agenda for the Next President & Congress of the United States A Proposal From The Adventist Health Policy Association To Promote Sound Health Policy In 2016 And Beyond Five Steps to Health in America A Health Policy Agenda For The Next President & Congress Of The United States A Proposal from the Adventist Health Policy Association To Promote Sound Health Policy In 2016 and Beyond October 2015 www.adventisthealthpolicy.org PREFACE The Seventh-day Adventist commitment to fostering human health began more than 150 years ago at a time when much of what passed for medical care was in fact detrimental. Patent medicines, often containing toxic or addictive substances, were widely offered as cures for nearly all ailments. Many medical interventions at the time – such as bloodletting, heroin for the common cold, and radium for arthritis and diabetes – caused far more harm than good. By contrast, Adventists began to teach the value of a healthy lifestyle and a preference for natural remedies including fresh air, regular exercise and pure water. Within a few years, Adventists expanded their health ministry by establishing innovative health care institutions. The first of these opened in 1866 in Battle Creek, Michigan, where people not only received treatment for diseases but were also taught how to prevent them. Since these early beginnings, Adventists have continued to build hundreds of hospitals, nursing homes, clinics, and health-sciences schools around the world. The Adventist work toward human health is founded on the belief that every person is a beloved child of the Creator, and deserving of compassionate, whole-person care with thoughtful attention to all dimensions of a person’s life. -

Collaborative Leadership Roles in the Implementation of Adventist Health Lifestyle: a Case Study of the Chinese Union Mission
Andrews University Digital Commons @ Andrews University Dissertations Graduate Research 2014 Collaborative Leadership Roles in the Implementation of Adventist Health Lifestyle: A Case Study of the Chinese Union Mission James Wu Andrews University, [email protected] Follow this and additional works at: https://digitalcommons.andrews.edu/dissertations Part of the Medicine and Health Sciences Commons, and the Religion Commons Recommended Citation Wu, James, "Collaborative Leadership Roles in the Implementation of Adventist Health Lifestyle: A Case Study of the Chinese Union Mission" (2014). Dissertations. 1566. https://digitalcommons.andrews.edu/dissertations/1566 This Dissertation is brought to you for free and open access by the Graduate Research at Digital Commons @ Andrews University. It has been accepted for inclusion in Dissertations by an authorized administrator of Digital Commons @ Andrews University. For more information, please contact [email protected]. Thank you for your interest in the Andrews University Digital Library of Dissertations and Theses. Please honor the copyright of this document by not duplicating or distributing additional copies in any form without the author’s express written permission. Thanks for your cooperation. ABSTRACT COLLABORATIVE LEADERSHIP ROLES IN THE IMPLEMENTATION OF ADVENTIST HEALTH LIFESTYLE: A CASE STUDY OF THE CHINESE UNION MISSION by James Wu Chair: Erich Baumgartner ABSTRACT OF GRADUATE STUDENT RESEARCH Dissertation Andrews University School of Education Title: COLLABORATIVE LEADERSHIP ROLES IN THE IMPLEMENTATION OF ADVENTIST HEALTH LIFESTYLE: A CASE STUDY OF THE CHINESE UNION MISSION Name of researcher: James Wu Name and degree of faculty chair: Erich Baumgartner, Ph.D. Date completed: July 2014 Problem Little is known about the roles of the institutional leader’s role in the collaborative implementation of the Adventist health lifestyle programs of the Chinese Union Mission of the Seventh-day Adventist Church in Hong Kong and Taiwan. -

Read Book Diet, Life Expectancy, and Chronic Disease : Studies Of
DIET, LIFE EXPECTANCY, AND CHRONIC DISEASE : STUDIES OF SEVENTH-DAY ADVENTISTS AND OTHER VEGETARIANS PDF, EPUB, EBOOK Gary E. Fraser | 392 pages | 01 Jul 2003 | Oxford University Press Inc | 9780195113242 | English | New York, United States Diet, Life Expectancy, and Chronic Disease : Studies of Seventh-Day Adventists and Other Vegetarians PDF Book Are vegans and vegetarians nuts? Respondents responded yes or no to a single question on whether they consumed alcohol beverages at the time of data collection. IJE vol. Highland Community News. This finding is consistent with previous research findings e. These include the laws of health. Download all slides. A study conducted by Masters and Knestel is of particular relevance in an attempt to understand the inverse relationship observed between intrinsic religiosity and hypertension in the present study. For systolic blood pressure, the mean for those with self-reported high blood pressure diagnosis was Many of their beliefs on vegetarian nutrition don't align with Gary's and the science; basic biochemistry and physiology around carbohydrates simply being glucose once ingested and raising blood glucose. LPenting marked it as to-read Feb 05, Fraser , Hardcover. This book analyzes the results of such studies, focusing on heart disease and cancer. Author information Copyright and License information Disclaimer. It was found that intrinsic religiosity may offer salutary effects on hypertension in our sample. Richards Edward Heppenstall Herbert E. Spiritual Meaning Spiritual meaning was measured using the spiritual meaning scale Mascaro et al. Written by. I would have included some discussion of the disadvantages of studying Adventists an atypical group with low disease risk. -

What Is Preventive Health & Lifestyle Medicine?
NAMCP Lifestyle Medicine Institute ”Lifestyle Medicine (LM) is the use of lifestyle interventions in the treatment and management of disease. Such interventions include diet (nutrition), exercise, stress management, smoking cessation, and a variety of other non-drug modalities. “ American College of Lifestyle Medicine • Addresses causes instead of symptoms • Deals with prevention--primary, secondary, and tertiary (but not simply traditional Preventive Medicine) • Inline with the Leading Health Indicators---Healthy People 2010: Physical Activity Mental Health Overweight and Obesity Injury and Violence Tobacco Use Environmental Quality Substance Abuse Immunization Responsible Sexual Behavior Access to Health Care Large Scale Epidemiological Findings Blue Zones Adventist Health Study China Study Harvard Nurses Health Study Blue Zones (Dan Buettner) •Where people commonly live active lives past the age of 100 years • Five Known Blue Zone locations: •Sardinia, Italy •Okinawa, Japan •Nicoya Peninsula, Costa Rica •Icaria, Greece •Loma Linda, CA Characteristics: The people inhabiting Blue Zones share common lifestyle characteristics that contribute to their longevity. Among the lifestyle characteristics shared among the Okinawa, Sardinia, and Loma Linda Blue Zones are the following: 1. Family (family is put ahead of other concerns) 2. No Smoking 3. Plant-based diet (the majority of food consumed is derived from plants) 4. Physical activity (constant moderate) 5. Social engagement (people of all ages are socially active and integrated into their communities) 6. Legumes are commonly consumed. Adventist Health Studies Adventist Health Study 1 (AHS-1)--(1974–1988) Adventist Mortality Study •Involved approximately 34,000 Californian Adventists over •The first major study of Adventists 25 years of age begun in 1960 •Purpose was to find out which components of the •Consisting of 22,940 California Adventist lifestyle give protection against disease. -

Adventist Religion & Health Study Follow-Up (PDF)
Three years ago you were one of over 10,000 people who filled out the first questionnaire in the Adventist Religion & Health Study, a substudy of the Adventist Health Study-2. We greatly appreciate your participation. Now we ask that you fill out the questionnaire once again. BAR This will give us important information about how Please return your completed questionnaire CODE changes in your life may have affected your in the envelope health. provided to: AREA LOMA LINDA U NIVERSITY Adventist Health Studies in partnership with OAKWOOD Evans Hall, Room 203 COLLEGE and the Seventh-day Loma Linda University Adventist Churches of North America Loma Linda CA 92350 PLEASE DO NOT WRITE IN THIS AREA SERIAL # 6232301 Please read all the instructions carefully. Each of the questions on the following pages has a number of bubbles like this next to them. 1. Please fill in one bubble for each question unless otherwise directed. Take care that the mark fills the circle and does not stray near other Shade bubbles like this bubbles. Not like this ✓ ✗ 2. Erase cleanly any answer you wish to change. A. Your Religious and Social Environment Which of the following categories best describes your religious belief now and, if you are married, describes your spouse’s religious belief now. For SDA No office Other formal Not use Inactive Active Catholic Jewish Other Don't only Protestant religion know married 1. Your belief now 1 2. Your spouse's belief now 2 Under 26 to 51 to 101 to 201 to 401 to 601 to Over 25 50 100 200 400 600 1000 1000 3.