Injection Technique 2: Administering Drugs Via the Subcutaneous Route
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Administering a Subcutaneous Injection
Inject medication slowly and release skin Will the injection hurt? Children may describe a pinching/stinging or bee-sting sensation during Our Lady’s Children’s Leave needle in place for 5-10 seconds after and just after the injection. It is normal for the Hospital, Crumlin, Dublin injecting medication, if possible injection site to be a little red and tender. It is 12 Remove needle swiftly and smoothly expected that children may be afraid of injections. It is important to be honest and explain the Wipe area gently with cotton wool, do not rub injection in a manner that they can understand. ….where children’s health comes first as this may be sore. Apply a plaster if needed. How to reduce any discomfort: ADVICE FOR • Prepare your child, explain why this is necessary PARENTS/GUARDIANS/CHILDREN and how you will give the injection Step 4. Dispose of the Needle/Syringe • Use distraction and play to amuse your child Administering a • Encourage them to practice on their teddy or doll. For infants, give them a soother/comforter if Subcutaneous Injection Dispose of needle and syringe immediately into they use one a sharps bin • Ensure clothing over the injection site is not tight My child has a bleeding disorder: seek medical advice before giving injections to your child. Auto-injector: Some children use an automatic injection device, often called a ‘rocket’. Specific Instructions: ……………………………………………………………………… ………………………………………………………………………. Developed by: Naomi Bartley, Clinical Placement Coordinator. CONTACT DETAILS Example of an Auto-Injector st Date issued: July 2014, October 2012 : 1 edn. Ward / Dept. Name: _________________ Date of review: July 2017 Telephone: ___________________ Follow the manufacture’s instructions for ©2014, Our Lady’s Children’s Hospital Crumlin, Dublin 12. -

Fascia Iliaca Block in the Emergency Department for Hip Fracture
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Serveur académique lausannois Pasquier et al. BMC Geriatrics (2019) 19:180 https://doi.org/10.1186/s12877-019-1193-0 RESEARCH ARTICLE Open Access Fascia iliaca block in the emergency department for hip fracture: a randomized, controlled, double-blind trial Mathieu Pasquier1, Patrick Taffé2, Olivier Hugli1, Olivier Borens3, Kyle Robert Kirkham4 and Eric Albrecht5* Abstract Background: Hip fracture causes moderate to severe pain and while fascia iliaca block has been reported to provide analgesic benefit, most previous trials were unblinded, with subsequent high risks of performance, selection and detection biases. In this randomized, control double-blind trial, we tested the hypothesis that a fascia iliaca block provides effective analgesia for patients suffering from hip fracture. Methods: Thirty ASA I-III hip fracture patients over 70 years old, who received prehospital morphine, were randomized to receive either a fascia iliaca block using 30 ml of bupivacaine 0.5% with epinephrine 1:200,000 or a sham injection with normal saline. The fascia iliaca block was administered by emergency medicine physicians trained to perform an anatomic landmark-based technique. The primary outcome was the comparison between groups of the longitudinal pain score profiles at rest over the first 45 min following the procedure (numeric rating scale, 0–10). Secondary outcomes included the longitudinal pain score profiles on movement and the comparison over 4 h, 8 h, 12 h, and 24 h after the procedure, along with cumulative intravenous morphine consumption at 24 h. Results: At baseline, the fascia iliaca group had a lower mean pain score than the sham injection group, both at rest (difference = − 0.9, 95%CI [− 2.4, 0.5]) and on movement (difference = − 0.9, 95%CI [− 2.7; 0.9]). -
Technical Considerations for Pen, Jet, and Related Injectors Intended for Use with Drugs and Biological Products
Guidance for Industry and FDA Staff: Technical Considerations for Pen, Jet, and Related Injectors Intended for Use with Drugs and Biological Products Additional copies are available from: Office of Combination Products Office of Special Medical Programs Office of the Commissioner Food and Drug Administration 10903 New Hampshire Avenue, WO-32 Hub 5129 Silver Spring, MD 20993 (Tel) 301-796-8930 (Fax) 301-796-8619 http://www.fda.gov/CombinationProducts/default.htm This document finalizes the draft guidance issued in April 2009. For questions regarding this document, contact the Office of Combination Products at [email protected] or Patricia Y. Love, MD at 301-796-8933 or [email protected] U.S. Department of Health and Human Services Food and Drug Administration Center for Devices and Radiological Health, Center for Drug Evaluation Research, Center for Biologics Evaluation and Research, and Office of Combination Products in the Office of the Commissioner June 2013 Contains Nonbinding Recommendations Table of Contents INTRODUCTION.....................................................................................................................3 BACKGROUND .......................................................................................................................4 SECTION I: SCIENTIFIC AND TECHNICAL CONSIDERATIONS.............................5 A. INJECTOR DESCRIPTION .............................................................................................5 B. DESIGN FEATURES.........................................................................................................9 -

Refi Ning Procedures for the Administration of Substances
WORKINGPARTY REPORT Rening procedures for theadministration of substances Report of the BVAAWF =FRAME=RSPCA=UFAW JointWorking Group on Renement Members of theJoint Working Groupon Renement: D.B.Morton (Chairman), M.Jennings (Secretary),A. Buckwell, R.Ewbank, C.Godfrey, B.Holgate, I. Inglis, R.James, C.Page,I. Sharman, R.Verschoyle, L.Westall &A.B.Wilson Contents Preface 2 3.6 Intraperitoneal 19 1Introduction and aimsof thereport 2 3.7 Intratracheal 20 3.8 Intravaginal 20 2Generalprinc iplesof `good practice’ 3 2.1 Planningand preparation 3 3.9 Intravenous and intra-arterial 21 2.1.1 Experimental aims 3 3.10 Oral routes 25 2.1.2 Theroute 3 3.10.1 Inclusionin an animal’s food orwater 25 2.1.3 Thesubstance 3 3.10.2 Dosingdirectly into 2.1.4 Theanimal 5 the pharynx 27 2.1.5 Thetechnique 7 3.10.3 Oral gavage 28 2.1.6 Staff and training 7 3.11 Osmotic minipumps 30 2.2 Technical preparation 3.12 Respiratory routes 31 andaftercare 8 3.12.1 Wholebody exposure 31 2.3 Generalre® nem entfor 3.12.2 Noseonly =Snout only all routes 9 exposure 32 3Re®nem entfor individual routes 3.12.3 Mask exposure 33 and procedures 13 3.13 Subcutaneous 34 3.1 Intra-articular 13 3.14 TopicalÐderm al 35 3.2 Intracerebral (intracerebro- 3.15 TopicalÐoc ular 36 ventricular) 14 3.16 Footpad 37 3.3 Intradermal 16 3.17 Uncommonroutes 38 3.4 Intramuscular 16 4Special considerations for wildanimals 38 3.5 Intranasal 18 References 39 Correspo ndenceandre q uestsfo rreprintst o:ProfessorD.B.Morton,DepartmentofBiomedicalSciences & BiomedicalEthic s, TheMed icalScho ol,UniversityofBirm ingham,Ed gbaston,Birm inghamB152TT, UK Accepted 14July 2000 # LaboratoryAnimals Ltd. -

Upper and Lower Limb Blocks in Children
Upper and lower limb blocks in children Adrian Bosenberg Correspondence Email: [email protected] INTRODUCTION insulated needles are the next best option Regional anaesthesia is commonly used as an although successful blocks can be achieved with 6 rinciples of clinical anaesthesia adjunct to general anaesthesia and plays a key non-insulated needles. P role in the multimodal approach to perioperative Nerve stimulator 1,2 pain management in children. Peripheral nerve Many peripheral nerve stimulators are available. SUMMARY blockade has increased with the development of Familiarise yourself with a particular device and age-appropriate equipment, safer, long-acting This article outlines regional stick with it. Read the manufacturer’s instructions anaesthetic techniques and local anaesthetic agents, increasing experience and understand how the nerve stimulator works methods used to identify and and low complication rates. before you use it.7 block individual nerves to provide analgesia for surgical The safety of peripheral nerve blocks in children The following basic principles should be followed procedures of the upper has been established in large-scale prospective to locate a peripheral nerve or plexus accurately: and lower limbs. Expertly studies, although caudal epidural remains the performed, peripheral nerve most popular and frequently used block in • Muscle relaxants must be withheld until after blocks can provide long lasting 3-5 completion of the block. anaesthesia and analgesia infants and small children. The experience of for surgery or after injury to the operator, pathology, the site and extent of • Attach the Negative electrode to the Needle the upper or lower limbs in surgery, the child’s body habitus and the presence and the Positive electrode to the Patient using children. -
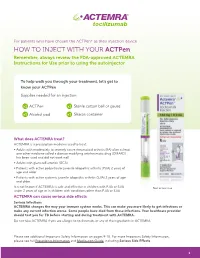
HOW to INJECT with YOUR Actpen Remember, Always Review the FDA-Approved ACTEMRA Instructions for Use Prior to Using the Autoinjector
For patients who have chosen the ACTPen® as their injection device HOW TO INJECT WITH YOUR ACTPen Remember, always review the FDA-approved ACTEMRA Instructions for Use prior to using the autoinjector To help walk you through your treatment, let’s get to know your ACTPen Supplies needed for an injection: x1 ACTPen x1 Sterile cotton ball or gauze x1 Alcohol pad x1 Sharps container What does ACTEMRA treat? ACTEMRA is a prescription medicine used to treat: • Adults with moderately to severely active rheumatoid arthritis (RA) after at least one other medicine called a disease modifying antirheumatic drug (DMARD) has been used and did not work well • Adults with giant cell arteritis (GCA) • Patients with active polyarticular juvenile idiopathic arthritis (PJIA) 2 years of age and older • Patients with active systemic juvenile idiopathic arthritis (SJIA) 2 years of age and older It is not known if ACTEMRA is safe and effective in children with PJIA or SJIA Not actual size. under 2 years of age or in children with conditions other than PJIA or SJIA. ACTEMRA can cause serious side effects Serious Infections ACTEMRA changes the way your immune system works. This can make you more likely to get infections or make any current infection worse. Some people have died from these infections. Your healthcare provider should test you for TB before starting and during treatment with ACTEMRA. Do not take ACTEMRA if you are allergic to tocilizumab, or any of the ingredients in ACTEMRA. Please see additional Important Safety Information on pages 9-10. For more Important Safety Information, please see full Prescribing Information and Medication Guide, including Serious Side Effects. -

Injectable Supramolecular Polymer–Nanoparticle Hydrogels Enhance Human Mesenchymal Stem Cell Delivery
Received: 13 July 2019 Revised: 25 September 2019 Accepted: 1 October 2019 DOI: 10.1002/btm2.10147 RESEARCH REPORT Injectable supramolecular polymer–nanoparticle hydrogels enhance human mesenchymal stem cell delivery Abigail K. Grosskopf1 | Gillie A. Roth2 | Anton A. A. Smith3 | Emily C. Gale4 | Hector Lopez Hernandez3 | Eric A. Appel3 1Department of Chemical Engineering, Stanford University, Stanford, California Abstract 2Department of Bioengineering, Stanford Stem cell therapies have emerged as promising treatments for injuries and diseases in University, Stanford, California regenerative medicine. Yet, delivering stem cells therapeutically can be complicated 3Department of Materials Science & Engineering, Stanford University, Stanford, by invasive administration techniques, heterogeneity in the injection media, and/or California poor cell retention at the injection site. Despite these issues, traditional administra- 4 Department of Biochemistry, Stanford tion protocols using bolus injections in a saline solution or surgical implants of cell- University, Stanford, California laden hydrogels have highlighted the promise of cell administration as a treatment Correspondence strategy. To address these limitations, we have designed an injectable polymer– Eric A. Appel, Department of Materials Science & Engineering, Stanford University, nanoparticle (PNP) hydrogel platform exploiting multivalent, noncovalent interactions Stanford, CA 94305. between modified biopolymers and biodegradable nanoparticles for encapsulation Email: [email protected] -

Pharmacokinetic Study of Nicotine and Its Metabolite Cotinine to Clarify Possible Association Between Smoking and Voiding Dysfunction in Rats Using UPLC/ESI-MS
Drug Metab. Pharmacokinet. 26 (4): 416422 (2011). Copyright © 2011 by the Japanese Society for the Study of Xenobiotics (JSSX) Regular Article Pharmacokinetic Study of Nicotine and Its Metabolite Cotinine to Clarify Possible Association between Smoking and Voiding Dysfunction in Rats Using UPLC/ESI-MS Satomi ONOUE*,NoriyukiYAMAMOTO,YoshikiSETO and Shizuo YAMADA Department of Pharmacokinetics and Pharmacodynamics and Global Center of Excellence (COE) Program, School of Pharmaceutical Sciences, University of Shizuoka, Shizuoka, Japan Full text of this paper is available at http://www.jstage.jst.go.jp/browse/dmpk Summary: The present study was undertaken to clarify the possible association between nicotine intake/ cigarette smoking and detrusor instability. For pharmacokinetic characterization of nicotine and cotinine (a major and pharmacologically less active metabolite of nicotine), a rapid ultra-performance liquid chromatography/electrospray ionization-mass spectrometry (UPLC/ESI-MS) method was developed that requires only a small amount of sample and simple pretreatment. The UPLC/ESI-MS method was validated with a focus on specificity, sensitivity (limit of detection, 2.5 ng/mL; limit of quantification, 5 ng/mL), linearity (r > 0.998), accuracy (97.2102.8%), precision (relative standard deviation <8%) and robustness in accordance with ICH guidelines (Q2B Validation of Analytical Procedures: Methodology). The developed method was successfully applied to determine nicotine and cotinine levels in rat biological samples such as plasma, urine and several tissues. After subcutaneous administration of nicotine ditartrate (2 mg/kg of body weight) in rats, the absorbed nicotine was rapidly and extensively metabolized into cotinine. However, nicotine was found to be predominant in cortex and bladder, where nicotinic acetylcholine receptors were expressed for neuronal control of voiding function. -

Injection Guide Overview and Goals of This Guide ����������������������������������� 1
Injection Guide Overview and goals of this guide . 1 Overview of injections. 3 Why did my doctor choose an injectable medication? ��������������� 3 Differences between injectable medication and oral medication . 3 Types of injections. 4 Parts of a syringe ��������������������������������������������������� 4 Steps for injecting medication ��������������������������������������� 5 Storage ������������������������������������������������������������� 5 Preparation ��������������������������������������������������������� 6 Wash your hands ����������������������������������������������� 6 Prepare your medication for injection ��������������������������� 7 Prepare the injection site ��������������������������������������� 8 Injection ����������������������������������������������������������� 9 Intramuscular injection ����������������������������������������� 9 Subcutaneous injection ����������������������������������������10 Disposal. .11 Monitoring of the injection site ����������������������������� 12 References . .13 Injection-site records ������������������������������������������������14 Overview and goals of this guide This guide is a quick reference on how to use medications that are given by injection. It gives step-by-step instructions for preparing and injecting the medication. It also covers safety precautions. The instructions in this guide apply whether you are giving the injection to someone you care for or you are giving the injection to yourself. This guide is not meant to replace instructions from your doctor nor the information -

Ultrasound-Guided Regional Anesthesia and Clinical Skills Workshop
Ultrasound-Guided Regional Anesthesia and Clinical Skills Workshop 2 Table of Contents I. Upper extremity neuroanatomy…………………….…………………………….. page 3 II. Upper extremity regional techniques…………………………………………..... page 5 III. Lower extremity neuroanatomy…………...…………………………….…...... page 13 IV. Lower extremity regional techniques……………………..…………………... page 16 V. Truncal neuroanatomy and regional techniques..……..……………..….....… page 26 VI. Suggested reading…………………………………………..………..…………. page 29 3 4 I. Upper Extremity Neuroanatomy Figure 1. Brachial plexus Roots: Anterior (ventral) rami of C5 - T1 (variable contributions from C4 and T1) Trunks: Form at the lateral border of the middle scalene muscle • Superior trunk: formed from C5 and C6 • Middle trunk: formed from C7 • Inferior trunk: formed from C8 and T1 Divisions: All trunks separate into an anterior and posterior division at the lateral border of the 1st rib (above & behind the middle 3rd of the clavicle) • Anterior divisions: supply the ventral (flexor) portion of the extremity • Posterior divisions: supply the dorsal (extensor) portion of the extremity Cords: Form at the apex of the axilla and named according to their relationship to the second part of the axillary artery (posterior to the pectoralis minor). • Lateral cord: formed from anterior divisions of the superior and middle trunks • Posterior cord: formed from the posterior divisions of all three trunks • Medial cord: formed from the anterior division of the inferior trunk Terminal Branches: Form at the lateral border of the pectoralis minor • Lateral cord has two major terminal branches 1. Musculocutaneous nerve (supplies biceps and terminates as lateral antebrachial cutaneous nerve of the forearm) 2. Median nerve (lateral root) • Posterior Cord has two major terminal branches 1. Axillary nerve (supplies deltoid and cutaneous skin innervation over lateral shoulder) 2. -

EUA) of REGEN-COVTM (Casirivimab and Imdevimab
FACT SHEET FOR HEALTH CARE PROVIDERS EMERGENCY USE AUTHORIZATION (EUA) OF REGEN-COVTM (casirivimab and imdevimab) AUTHORIZED USE TREATMENT The U.S. Food and Drug Administration (FDA) has issued an Emergency Use Authorization (EUA) to permit the emergency use of the unapproved product, REGEN-COV (casirivimab and imdevimab) co-formulated product and REGEN-COV (casirivimab and imdevimab) supplied as individual vials to be administered together, for the treatment of mild to moderate coronavirus disease 2019 (COVID-19) in adult and pediatric patients (12 years of age and older weighing at least 40 kg) with positive results of direct SARS-CoV-2 viral testing, and who are at high risk for progression to severe COVID-19, including hospitalization or death. Limitations of Authorized Use • REGEN-COV (casirivimab and imdevimab) is not authorized for use in patients: - who are hospitalized due to COVID-19, OR - who require oxygen therapy due to COVID-19, OR - who require an increase in baseline oxygen flow rate due to COVID-19 in those on chronic oxygen therapy due to underlying non-COVID-19 related comorbidity. • Monoclonal antibodies, such as REGEN-COV, may be associated with worse clinical outcomes when administered to hospitalized patients with COVID-19 requiring high flow oxygen or mechanical ventilation. POST-EXPOSURE PROPHYLAXIS The U.S. Food and Drug Administration (FDA) has issued an Emergency Use Authorization (EUA) to permit the emergency use of the unapproved product, REGEN-COV (casirivimab and imdevimab) co-formulated product and REGEN-COV -

Development of in Situ Self-Assembly Nanoparticles to Encapsulate Lopinavir and Ritonavir for Long-Acting Subcutaneous Injection
pharmaceutics Article Development of In Situ Self-Assembly Nanoparticles to Encapsulate Lopinavir and Ritonavir for Long-Acting Subcutaneous Injection Irin Tanaudommongkon, Asama Tanaudommongkon and Xiaowei Dong * Department of Pharmaceutical Sciences, University of North Texas Health Science Center, Fort Worth, TX 76107, USA; [email protected] (I.T.); [email protected] (A.T.) * Correspondence: [email protected]; Tel.: +1-817-735-2785 Abstract: Most antiretroviral medications for human immunodeficiency virus treatment and preven- tion require high levels of patient adherence, such that medications need to be administered daily without missing doses. Here, a long-acting subcutaneous injection of lopinavir (LPV) in combination with ritonavir (RTV) using in situ self-assembly nanoparticles (ISNPs) was developed to potentially overcome adherence barriers. The ISNP approach can improve the pharmacokinetic profiles of the drugs. The ISNPs were characterized in terms of particle size, drug entrapment efficiency, drug loading, in vitro release study, and in vivo pharmacokinetic study. LPV/RTV ISNPs were 167.8 nm in size, with a polydispersity index of less than 0.35. The entrapment efficiency was over 98% for both LPV and RTV, with drug loadings of 25% LPV and 6.3% RTV. A slow release rate of LPV was observed at about 20% on day 5, followed by a sustained release beyond 14 days. RTV released faster than LPV in the first 5 days and slower than LPV thereafter. LPV trough concentration remained above 160 ng/mL and RTV trough concentration was above 50 ng/mL after 6 days with one subcutaneous injection. Overall, the ISNP-based LPV/RTV injection showed sustained release profiles in both Citation: Tanaudommongkon, I.; Tanaudommongkon, A.; Dong, X.