Molecular Methods for the Detection of TEM- and SHV Related Beta Lactamase Genes in Members of the Enterobacteriaceae
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Aero-Blaaupan Precinct: Detailed Development Framework
DRAFT CITY OF EKURHULENI: URBAN DESIGN PRECINCT PLANS AERO-BLAAUPAN PRECINCT DETAILED DEVELOPMENT FRAMEWORK Prepared by: The GAPP Consortium Prepared for: Metropolitan Spatial Planning Division City Planning Department City of Ekurhuleni Submitted: 20 April 2018 Version: 2 GAPP Consortium Aero-Blaaupan Precinct: Detailed Development Framework CONTACT DETAILS CLIENT Metropolitan Spatial Planning Division City Planning Department City of Ekurhuleni tel: +27(0)11-999-4026 email: [email protected] web: www.ekurhuleni.gov.za PROFESSIONAL TEAM GAPP Architects and Urban Designers Contact: Andrew Luke tel: +27 11 482 1648 email: [email protected] web: www.gapp.net Royal Haskoning DHV Contact: Janet Loubser tel: +27 12 3675800 email: [email protected] web: www.rhdhv.co.za Kayamandi Development Services Contact: Russel Aird tel: +27 12 346 4845 email: [email protected] web: www.kayamandi.co.za 20 April 2018 (Final Draft) i GAPP Consortium Aero-Blaaupan Precinct: Detailed Development Framework TABLE OF CONTENTS 4.2.3 Non-Residential Land Use Activities .............................................. 25 4.2.4 Existing Nodes ............................................................................... 25 4.2.5 Nodal development in terms of Proposed Spatial Policy................ 25 CONTACT DETAILS ............................................................................................... I 4.2.6 Consolidated Regional Spatial Strategy......................................... 25 TABLE OF CONTENTS ........................................................................................ -

Or Tambo International
KEMPTON POMONA PARK OFFRA From ATNS head office from Hulley Rd take a left into Andre Greyvenstein Rd. M45 BENONI Carry on straight, past Mastercars & Nissan (R23) ALLEN until it turns into Albatross Rd. On Albatross Road. Keep to the left. AVION PARK Pass Boundary Silk Bazaar on left at robot. SHOPRITE R21 CHECKERS Take slip road M45 R23 Benoni, Allen Grove after overpass, keep left when turning. Turn into slip road (M43 Atlas Rd M45 Benoni). ALBATROSS RD (BRIDGE) M43 ATLAS RD Swing around into Atlas Road and M45 BENONI VOORTREKKER take a right at next robot into Bonaero Drive. M32 M32 RHODESFIELD POMONA LUGVRAG/AIRFREIGHT M43 ATLAS RD BENONI OFFRAMP (M45) On Albatross Road. Keep to the left. VOORTREKKER TURN-OFF Pass Boundary Silk Bazaar on left at robot. Take slip road M45 R23 Benoni, Allen Grove after overpass, keep left when turning. Turn into slip road (M43 Atlas Rd M45 Benoni). Swing around into Atlas Road and take a right at next robot into Bonaero Drive. On R21 highway going north. ISANDO Take M43 Atlas Rd turnoff at first robot turn right HEAD OFFICE STERCARS R21 I SAN into Bonaero Drive. MA N S (011) 961-0100 BONAERO SAFAIR PARK HOLIDAY INN On R21 highway going south. SIM GARDEN L L RD Y Take M43 Atlas Rd turnoff HU HU LE ANDRE GREYVENSTEIN RD at first robot turn right JOHANNESBURG into Bonaero Drive. Via Barbara Rd R24 R2 R21 JHB INTER. AIRPORT BOKSBURG On R21 highway going south. KEMPTON PARK LL Take M43 Atlas Rd turnoff INTERCHANGE A AVIATION TRAINING SBURGM ACADEMY at first robot turn right AIR TRAFFIC BOK into Bonaero Drive. -

An Overview of Rural Change in Africa
~ " Rural Futures P ·ogramn1 TRANSFORMING AFRICA A NEW EMERGING RURAL WORLD An Overview of Rural Change in Africa z nd edition , .... ..cc BY NC ND https://creativecommons.org/hcenses/by-nc-nd/4.0/deed.en Juty2016 The Cirad the NEPAD Agency. rights owners. authorize the use of the original work for non-commercial purposes. but does not authorize the creation ofderivat ive works. Cover Photo : Geneviève Cortes Printîng : lmp:Actlmprimerîe. Saint Gelydu Fesc (34 - France) ISBN: 978-2-87614-719-5 An Overview of Rural Change in Africa znd edition A NEW EMERGING RURAL WORLD An Overview of Rural Change in Africa 2nd edition Citation: Pesche D .. Losch B. lmbernon J. (Eds.l. 2016. A New Emerging Rural World. An OverviewofRural Change inAfrica. Atlas for the NEPAD Rural Futures Programme. Second Edition. Revised and Enlarged. Montpellier. Cirad. NEPAD Agency. 76 p. This atlas on rura l change in Africa. for this second edition. revised and enlarged. was prepared at the request oft he NEPAD Agency and un der t he overall coordination and guidance of Ibrahim Assane Mayaki, NEPAD Agency CEO. Estherine Lisinge Fotabong. Programme lmplementation and Coordination Director. lt is part of the partnership between Ci rad and NEPAD and benefited from the financial support of NEPAD. AFD and Cirad. Conceived to inform research and discussions during the Second Africa Rural Development Forum (ARDF) held in Yaoundé. Cameroun. from 8 to 10 September 2016. it contributes to the work of the NEPAD Rural Futures programme. The completion of t he atlas has involved 52 aut hors whose detailed list is provided on page 73. -

36927 18-10 Roadcarrierp P1 Layout 1
Government Gazette Staatskoerant REPUBLIC OF SOUTH AFRICA REPUBLIEK VAN SUID-AFRIKA October Vol. 580 Pretoria, 18 2013 Oktober No. 36927 PART 1 OF 4 N.B. The Government Printing Works will not be held responsible for the quality of “Hard Copies” or “Electronic Files” submitted for publication purposes AIDS HELPLINE: 0800-0123-22 Prevention is the cure 305096—A 36927—1 2 No. 36927 GOVERNMENT GAZETTE, 18 OCTOBER 2013 IMPORTANT NOTICE The Government Printing Works will not be held responsible for faxed documents not received due to errors on the fax machine or faxes received which are unclear or incomplete. Please be advised that an “OK” slip, received from a fax machine, will not be accepted as proof that documents were received by the GPW for printing. If documents are faxed to the GPW it will be the sender’s respon- sibility to phone and confirm that the documents were received in good order. Furthermore the Government Printing Works will also not be held responsible for cancellations and amendments which have not been done on original documents received from clients. CONTENTS INHOUD Page Gazette Bladsy Koerant No. No. No. No. No. No. Transport, Department of Vervoer, Departement van Cross Border Road Transport Agency: Oorgrenspadvervoeragentskap aansoek- Applications for permits:.......................... permitte: .................................................. Menlyn..................................................... 3 36927 Menlyn..................................................... 3 36927 Applications concerning Operating Aansoeke -

Exemption Letter
P.O.BOX73703 LYNNWOOD RIDGE 0040 Tel: 083 459 3091 Fax: 086 695 7247 Email: [email protected] Comprehensive and Professional Solutions for all Heritage Related Matters CK 2006/014630/23 VAT NO.: 4360226270 APAC019/83 2020-02-18 Your Reference: Case ID# 14632 To: Mr. Andrew Salomon Archaeology, Palaeontology and Meteorites Unit South African Heritage Resource Agency P O Box 4637 Cape Town 8000 RE: MOTIVATION FOR EXEMPTION FROM PHASE 1 HERITAGE IMPACT ASSESSMENT – THE DEVELOPMENT OF A FILLING STATION ON ERF 4 VREDEBOS EXTENSION 1, CITY OF EKURHULENI METROPOLITAN MUNICIPALITY, GAUTENG PROVINCE APelser Archaeological Consulting cc (APAC cc) was appointed by Bokamoso Landscape Architects & Environmental Consultants CC to undertake an assessment for the proposed Vredebos Filling Station development and to provide a motivation for the exemption from a Full Phase 1 HIA for the proposed development. Key Spirit Developments (Pty) Ltd proposes the development of a filling station on the property known as Erf 4 Vredebos Extension 1, City of Ekurhuleni Metropolitan Municipality, Gauteng Province. The development and study area measures 0.58 hectares in extent. A physical field study was not conducted for this exemption motivation. Previous heritage assessment work (field-based) conducted by the author in Vredebos, as well as information from earlier desktop research informed the results of this assessment and the recommendations provided. Background to the Project A notification regarding the development was submitted to SAHRA, who acknowledged receipt of this and provided a letter on the 30th of January 2020 in this regard. A Case ID (#14632) was assigned to this project. -

Review Record Sheet
Zitholele Consulting Reg. No. 2000/000392/07 PO Box 6002 Halfway House 1685 South Africa Thandanani Park, Matuka Close Halfway Gardens, Midrand Tel + (27) 11 207 2060 Fax + (27) 86 674 6121 E-mail : [email protected] REPORT ON WASTE MANAGEMENT LICENSE APPLICATION FOR THE ZIMCO ALUMINIUM COMPANY (ZIMALCO), A DIVISION OF THE ZIMCO GROUP (PTY) LTD, BENONI, GAUTENG PROVINCE FINAL SCOPING REPORT & PLAN OF STUDY FOR EIA DEA Ref. No: 12/9/11/L1290/3 Report No : 12984-46-Rep-004-FSR-Rev0 Submitted to: Zimco Aluminium Company, a Division of the Zimco Group (Pty) Ltd P.O. Box 5044 Benoni South 1502 DISTRIBUTION: 2 Copies - Zimco Aluminium Company, a Division of the Zimco Group (Pty) Ltd 1 Copy - Zitholele Consulting (Pty) Ltd – Library 1 Copy - Ekurhuleni Metropolitan Municipality November 2013 12984 Directors : S Pillay (Managing Director); N Rajasakran (Director); Dr RGM Heath (Director) November 2013 i 12984 EXECUTIVE SUMMARY Introduction The existing Zimco Aluminium Company (Zimalco), a Division of the Zimco Group (Pty) Ltd, is a secondary aluminium smelter situated in the Benoni Industrial Sites, Benoni, in the Gauteng Province. The study site is situated in the jurisdiction of the Ekurhuleni Metropolitan Municipality. The operation recycles aluminium scrap and primary metal to produce aluminium foundry ingot, powder and master alloys which are then sold. The facility also processes aluminium dross to extract the metallic aluminium. The site is approximately 43 000m2 in extent. The processing of aluminium dross occurs in an area of approximately 10 000m2 in size. Activities undertaken on site are listed in Government Notice 718 of 2009 (List of Waste Management Activities that have, or are likely to have a detrimental effect on the environment) and therefore environmental authorisation in the form of a Waste Management License is required in terms of the National Environmental Management: Waste Act (Act 59 of 2008) [NEMWA]. -

Urban Design Precinct Plans Aero-Blaaupan Urban Design Precinct Plan
CITY OF EKURHULENI: URBAN DESIGN PRECINCT PLANS AERO-BLAAUPAN URBAN DESIGN PRECINCT PLAN Prepared by: The GAPP Consortium Prepared for: Metropolitan Spatial Planning Division City Planning Department City of Ekurhuleni Version: Final Submission GAPP Consortium Aero-Blaaupan Urban Design Precinct Plan CONTACT DETAILS CLIENT Metropolitan Spatial Planning Division City Planning Department City of Ekurhuleni tel: +27(0)11-999-4026 email: [email protected] web: www.ekurhuleni.gov.za PROFESSIONAL TEAM GAPP Architects and Urban Designers Contact: Andrew Luke tel: +27 11 482 1648 email: [email protected] web: www.gapp.net Royal HaskoningDHV Contact: Janet Loubser tel: +27 11 798 6000 email: [email protected] web: www.rhdhv.co.za Kayamandi Development Services Contact: Russell Aird tel: +27 12 346 4845 email: [email protected] web: www.kayamandi.co.za June 2018 – Vr 2 2 GAPP Consortium Aero-Blaaupan Urban Design Precinct Plan TABLE OF CONTENTS 2.4.2 National and Provincial Policies, Development Plans and Projects 50 2.4.3 Principles and Development Strategy ................................. 50 CONTACT DETAILS .................................................................................. 2 2.4.4 Airport East Development Strategy ..................................... 52 TABLE OF CONTENTS ............................................................................. 3 2.4.5 CoE Policies, Development Plans and Projects .................. 56 2.4.6 MSDF Urban Structuring Elements .................................... -

Actonville Wattville Rail Reserve Precinct Plan Draft Jun 2019
DRAFT ACTONVILLE WATTVILLE RAIL RESERVE URBAN DESIGN PRECINCT PLAN Metropolitan Spatial Planning Division City Planning Department City of Ekurhuleni GAPP Consortium Ekurhuleni Urban Design Precinct Plans CONTACT DETAILS CLIENT Metropolitan Spatial Planning Division City Planning Department City of Ekurhuleni tel: +27(0)11-999-4026 email: [email protected] web: www.ekurhuleni.gov.za PROFESSIONAL TEAM GAPP Architects and Urban Designers tel: +27 11 482 1648 email: [email protected] web: www.gapp.net Royal HaskoningDHV tel: email: web: Kayamandi Development Services tel: +27 12 346 4845 email: [email protected] web: www.kayamandi.co.za Submitted: 10 June 2019 2 GAPP Consortium Ekurhuleni Urban Design Precinct Plans TABLE OF CONTENTS 3 REGIONAL OVERVIEW .................................................................... 27 3.1 INTRODUCTION ........................................................................ 27 3.2 HISTORIC OVERVIEW OF ACTONVILLE ................................. 27 CONTACT DETAILS .................................................................................. 2 3.3 REGIONAL CONTEXT AND STATUS QUO ............................... 28 3.3.1 Institutional Boundaries ....................................................... 28 TABLE OF CONTENTS ............................................................................. 3 3.3.2 Locality and Accessibility ..................................................... 28 LIST OF DIAGRAMS ................................................................................. -

Imprensa Oficial 1992 HB2024.A418 Governo Do Estado Do Amazonas, 1992
Title Author BibliographicEntry YearPublished CallNumber Romanceiro da Batalha da Borracha. Benchimol, Samuel. Manaus: Imprensa Oficial 1992 HB2024.A418 Governo do Estado do Amazonas, 1992. Un Tal José Salomé. Azuela, Arturo. México: Editora Leega, 1982 PQ7298.1.Z77 1982. La Prudencia en la Mujer/El Molina, Tirso de. [Fray Gabriel Téllez] Madrid: Espasa-Calpe, 1964 PQ6434.P7 Condenado por Desconfiado. 6a ed. 1964. The Communist Manifesto. Marx, Karl and Frederick Engels. New York, London, 1964 HX276.M3 Toronto, and Sydney: Pocket Books, 1964. Tijuanenses. Campbell, Federico. México: Joaquín Mortiz, 1989 PQ7298.13.A392 1989. Ministers of God, Ministers of the Cabestrero, Teófilo. Maryknoll, New York: 1984 BX1442.2.C32 People: Testimonies of Faith from Orbis, 1984. Nicaragua. Translated by Robert R. Barr. Historia del Noveau Théâtre. Serreau, Geneviève. México: SigloXXI, 1967. 1967 PQ556.S4H Translated by Manuel de la Escalera. Breve Historia de la Revolución Silva Herzog, Jesús. México: Fondo de Cultura 1960 F1234.S586 Mexicana: La Etapa Constitucionalista Económica, 1960. y la Lucha de Facciones. Chapters of Brazil's Colonial History, Abreu, João Capistrano de. Oxford and New York: 1997 F2524.A2413 1500-1800. Translated by Arthur Oxford University Press, Brakel. 1997. Field Guide to the Plants of Inter Fitzmaurice, Sylvia. San Juan: Editorial 1990 QK230.F57 American University of Puerto Rico, Académica, 1990. San Germán Campus. Toward Renewed Economic Growth Balassa, Bela et al. México, Rio de Janeiro, and 1986 HC125.B48 in Latin America: Summary, Overview, Washington, D.C.: Institute and Recommendations. for International Economics, 1986. Steadfastness of the Saints: A Journal Berrigan, Daniel. Maryknoll, New York: 1986 BX4705.B3845 of Peace and War in Central and Orbis, 1986. -

YOUTH PERSPECTIVES on THEIR EMPOWERMENT in SUB-SAHARAN AFRICA: the CASE of KENYA a Dissertation Submitted to Kent State Univers
YOUTH PERSPECTIVES ON THEIR EMPOWERMENT IN SUB-SAHARAN AFRICA: THE CASE OF KENYA A dissertation submitted to Kent State University in partial fulfillment of the requirements for the degree of Doctor of Philosophy by Christine Mwongeli Mutuku August 2011 Dissertation written by Christine Mwongeli Mutuku BA., University of Nairobi, 1997 MA., Saginaw Valley State University, 2000 Ph.D., Kent State University, 2011 Approved by Steven R. Brown, Ph.D., Co-Chair, Doctoral Dissertation Committee Julie Mazzei, Ph.D., Co-Chair, Doctoral Dissertation Committee Andrew Barnes, Ph.D., Members, Doctoral Dissertation Committee Kenneth Cushner, Ph.D., Accepted by Steven W. Hook, Ph.D., Chair, Department of Political Science John R. D. Stalvey, Ph.D., Dean, College of Arts and Sciences ii TABLE OF CONTENTS Page LIST OF TABLES ................................................................................................................ vi ACKNOWLEDGEMENTS .................................................................................................. viii CHAPTERS 1. INTRODUCTION .......................................................................................................... 1 Youth in Africa ............................................................................................................... 2 Context: Kenya ............................................................................................................... 8 Problem Statement ........................................................................................................ -
Tswalu Information Guide
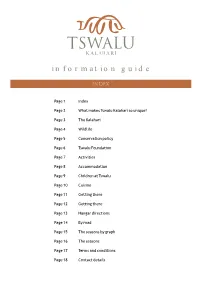
information guide Page 1 Index Page 2 What makes Tswalu Kalahari so unique? Page 3 The Kalahari Page 4 Wildlife Page 5 Conservation policy Page 6 Tswalu Foundation Page 7 Activities Page 8 Accommodation Page 9 Children at Tswalu Page 10 Cuisine Page 11 Getting there Page 12 Getting there Page 13 Hangar directions Page 14 By road Page 15 The seasons by graph Page 16 The seasons Page 17 Terms and conditions Page 18 Contact details Sense of Space Tswalu Kalahari, owned by the Oppenheimer family, is South Africa's largest private game reserve, covering an area of over 100,000 hectares (1,000 sq km or almost a quarter of a million acres). For comparison, this is twice the size of Pilanesberg National Park and bigger than the entire Madikwe reserve. This vast and magical landscape takes conservation as its first priority; indeed Nicky Oppenheimer's vision is to “restore the Kalahari to itself”. Flexibility No other game reserve offers such flexibility. Your dedicated complement of field guides and staff allows you to choose how you would like to spend your day – from breakfast in bed and an indulgent spa treatment in the comfort of your own deck overlooking the Kalahari, to a leisurely game drive, and a delicious private gourmet picnic which reflects the essence of Africa. Malaria-free Safari Tswalu is MALARIA-FREE and guests do not have to worry about taking anti-malaria tablets. It is therefore ideal for families, and at Tswalu we welcome children and actively encourage them to participate fully in the safari experience. -

Rutgers Business School 1 Washington Park, Room 946 Newark, NJ 07102 [email protected] Mobile (201) 454-4377 Fax (973) 353-1283
Miklos A. Vasarhelyi Rutgers Business School 1 Washington Park, Room 946 Newark, NJ 07102 [email protected] Mobile (201) 454-4377 Fax (973) 353-1283 CURRENT POSITION Rutgers University: KPMG Distinguished Professor of Accounting Information Systems Rutgers Business School - Newark & New Brunswick Director, Rutgers Accounting Research Center & Continuous Auditing & Reporting Lab EDUCATION University of California, Los Angeles, Graduate School of Management, Ph.D. Major: Accounting Information Systems - Minor: Finance & Computer Methods. Dissertation Title: Man Machine Planning Systems: A Behavioral Examination of Interactive Decision Making, 1973. Massachusetts Institute of Technology, Alfred P. Sloan School of Management M.S. in Management, Emphasis: Finance, 1969. Catholic University of Rio de Janeiro, Brazil, B.S. Electrical Engineering, 1966. State University of Guanabara, Brazil, B.S., Economics, 1966. PROFESSIONAL EXPERIENCE ACADEMIC Rutgers University, Graduate School of Management, Professor of Accounting Information Systems (1999-2001), Area Chair (1989, 1992), Director of the RARC (Rutgers Accounting Research Center) (1990-Present), Director of CAR Lab (2003-Present) University of Southern Europe - Monaco, Visiting Professor (2001-2002) University of Hawaii, Visiting Professor, Summer Sessions (1994, 1995) Theseus Institute, Sophia Antipolis, France, Visiting Professor (Fall 1993); Professor Vacataire (1993-Present) Columbia University, Graduate School of Business, Associate Professor of Accounting (1978-1987); Director of the Accounting Research Center (1983- 1987) University of Southern California, Department of Accounting, School of Business Administration, Assistant Professor of Accounting (1974-1978) Catholic University of Rio de Janeiro, Associate Professor (1972-1974). Creator and Coordinator of the MBA Program (1972-1974), Director of Rio Datacenter - 150 employees, at the time the largest data processing center in South America (1972-1974) PROFESSIONAL AT&T Bell Laboratories, the Consumer Laboratories, Murray Hill, NJ.