2 with Chronic Obstructive Pulmonary Disease Severity
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Polygenic Risk Score of SERPINA6/SERPINA1 Associates with Diurnal and Stress-Induced HPA Axis Activity in Children
Edinburgh Research Explorer Polygenic risk score of SERPINA6/SERPINA1 associates with diurnal and stress-induced HPA axis activity in children Citation for published version: Utge, S, Räikkönen, K, Kajantie, E, Lipsanen, J, Andersson, S, Strandberg, T, Reynolds, R, Eriksson, JG & Lahti, J 2018, 'Polygenic risk score of SERPINA6/SERPINA1 associates with diurnal and stress-induced HPA axis activity in children', Psychoneuroendocrinology. https://doi.org/10.1016/j.psyneuen.2018.04.009 Digital Object Identifier (DOI): 10.1016/j.psyneuen.2018.04.009 Link: Link to publication record in Edinburgh Research Explorer Document Version: Publisher's PDF, also known as Version of record Published In: Psychoneuroendocrinology General rights Copyright for the publications made accessible via the Edinburgh Research Explorer is retained by the author(s) and / or other copyright owners and it is a condition of accessing these publications that users recognise and abide by the legal requirements associated with these rights. Take down policy The University of Edinburgh has made every reasonable effort to ensure that Edinburgh Research Explorer content complies with UK legislation. If you believe that the public display of this file breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. Download date: 29. Sep. 2021 Psychoneuroendocrinology 93 (2018) 1–7 Contents lists available at ScienceDirect Psychoneuroendocrinology journal homepage: www.elsevier.com/locate/psyneuen Polygenic risk score of SERPINA6/SERPINA1 associates with diurnal and T stress-induced HPA axis activity in children Siddheshwar Utgea,b, Katri Räikkönena, Eero Kajantiec,d,e, Jari Lipsanena, Sture Anderssond, ⁎ Timo Strandbergf,g, Rebecca M. -

Differential Gene Expression of Serine Protease Inhibitors in Bovine
Hayashi et al. Reproductive Biology and Endocrinology 2011, 9:72 http://www.rbej.com/content/9/1/72 RESEARCH Open Access Differential gene expression of serine protease inhibitors in bovine ovarian follicle: possible involvement in follicular growth and atresia Ken-Go Hayashi, Koichi Ushizawa, Misa Hosoe and Toru Takahashi* Abstract Background: SERPINs (serine protease inhibitors) regulate proteases involving fibrinolysis, coagulation, inflammation, cell mobility, cellular differentiation and apoptosis. This study aimed to investigate differentially expressed genes of members of the SERPIN superfamily between healthy and atretic follicles using a combination of microarray and quantitative real-time PCR (QPCR) analysis. In addition, we further determined mRNA and protein localization of identified SERPINs in estradiol (E2)-active and E2-inactive follicles by in situ hybridization and immunohistochemistry. Methods: We performed microarray analysis of healthy (10.7 +/- 0.7 mm) and atretic (7.8 +/- 0.2 mm) follicles using a custom-made bovine oligonucleotide microarray to screen differentially expressed genes encoding SERPIN superfamily members between groups. The expression profiles of six identified SERPIN genes were further confirmed by QPCR analysis. In addition, mRNA and protein localization of four SERPINs was investigated in E2- active and E2-inactive follicles using in situ hybridization and immunohistochemistry. Results: We have identified 11 SERPIN genes expressed in healthy and atretic follicles by microarray analysis. QPCR analysis confirmed that mRNA expression of four SERPINs (SERPINA5, SERPINB6, SERPINE2 and SERPINF2) was greater in healthy than in atretic follicles, while two SERPINs (SERPINE1 and SERPING1) had greater expression in atretic than in healthy follicles. In situ hybridization showed that SERPINA5, SERPINB6 and SERPINF2 mRNA were localized in GCs of E2-active follicles and weakly expressed in GCs of E2-inactive follicles. -

The Serpintine Solution
& Experim l e ca n i t in a l l C C f a Journal of Clinical & Experimental o r d l i a o n l o r g u Lucas et al., J Clin Exp Cardiolog 2017, 8:1 y o J Cardiology ISSN: 2155-9880 DOI: 10.4172/2155-9880.1000e150 Editorial Open Access The Serpintine Solution Alexandra Lucas, MD, FRCP(C)1,2,*, Sriram Ambadapadi, PhD1, Brian Mahon, PhD3, Kasinath Viswanathan, PhD4, Hao Chen, MD, PhD5, Liying Liu, MD6, Erbin Dai, MD6, Ganesh Munuswami-Ramanujam, PhD7, Jacek M. Kwiecien, DVM, MSc, PhD8, Jordan R Yaron, PhD1, Purushottam Shivaji Narute, BVSc & AH, MVSc, PhD1,9, Robert McKenna, PhD10, Shahar Keinan, PhD11, Westley Reeves, MD, PhD12, Mark Brantly, MD, PhD13, Carl Pepine, MD, FACC14 and Grant McFadden, PhD1 1Center for Personalized Diagnostics, Biodesign Institute, Arizona State University, Tempe AZ, USA 2Saint Josephs Hospital, Dignity Health Phoenix, Phoenix, AZ, USA 3NIH/ NIDDK, Bethesda MD, USA 4Zydus Research Centre, Ahmedabad, India 5Department of tumor surgery, The Second Hospital of Lanzhou University, Lanzhou, Gansu, P.R.China 6Beth Israel Deaconess Medical Center, Harvard, Boston, MA, USA 7Interdisciplinary Institute of Indian system of Medicine (IIISM), SRM University, Chennai, Tamil Nadu, India 8MacMaster University, Hamilton, ON, Canada 9Critical Care Medicine Department, Clinical Center, National Institutes of Health, Bethesda MD, USA 10Department of Molecular Genetics and Microbiology, University of Florida, Gainesville, FL, USA 11Cloud Pharmaceuticals, Durham, North Carolina, USA 12Division of Rheumatology, University of Florida, -

Adaptive Evolution and Divergence of SERPINB3: a Young Duplicate in Great Apes
Adaptive Evolution and Divergence of SERPINB3: A Young Duplicate in Great Apes Sı´lvia Gomes1*, Patrı´cia I. Marques1,2, Rune Matthiesen3, Susana Seixas1* 1 Institute of Molecular Pathology and Immunology of the University of Porto (IPATIMUP), Porto, Portugal, 2 Institute of Biomedical Sciences Abel Salazar (ICBAS), University of Porto, Porto, Portugal, 3 National Health Institute Doutor Ricardo Jorge (INSA), Lisboa, Portugal Abstract A series of duplication events led to an expansion of clade B Serine Protease Inhibitors (SERPIN), currently displaying a large repertoire of functions in vertebrates. Accordingly, the recent duplicates SERPINB3 and B4 located in human 18q21.3 SERPIN cluster control the activity of different cysteine and serine proteases, respectively. Here, we aim to assess SERPINB3 and B4 coevolution with their target proteases in order to understand the evolutionary forces shaping the accelerated divergence of these duplicates. Phylogenetic analysis of primate sequences placed the duplication event in a Hominoidae ancestor (,30 Mya) and the emergence of SERPINB3 in Homininae (,9 Mya). We detected evidence of strong positive selection throughout SERPINB4/B3 primate tree and target proteases, cathepsin L2 (CTSL2) and G (CTSG) and chymase (CMA1). Specifically, in the Homininae clade a perfect match was observed between the adaptive evolution of SERPINB3 and cathepsin S (CTSS) and most of sites under positive selection were located at the inhibitor/protease interface. Altogether our results seem to favour a coevolution hypothesis for SERPINB3, CTSS and CTSL2 and for SERPINB4 and CTSG and CMA1.A scenario of an accelerated evolution driven by host-pathogen interactions is also possible since SERPINB3/B4 are potent inhibitors of exogenous proteases, released by infectious agents. -
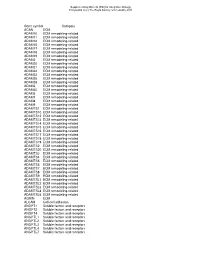
Gene Symbol Category ACAN ECM ADAM10 ECM Remodeling-Related ADAM11 ECM Remodeling-Related ADAM12 ECM Remodeling-Related ADAM15 E
Supplementary Material (ESI) for Integrative Biology This journal is (c) The Royal Society of Chemistry 2010 Gene symbol Category ACAN ECM ADAM10 ECM remodeling-related ADAM11 ECM remodeling-related ADAM12 ECM remodeling-related ADAM15 ECM remodeling-related ADAM17 ECM remodeling-related ADAM18 ECM remodeling-related ADAM19 ECM remodeling-related ADAM2 ECM remodeling-related ADAM20 ECM remodeling-related ADAM21 ECM remodeling-related ADAM22 ECM remodeling-related ADAM23 ECM remodeling-related ADAM28 ECM remodeling-related ADAM29 ECM remodeling-related ADAM3 ECM remodeling-related ADAM30 ECM remodeling-related ADAM5 ECM remodeling-related ADAM7 ECM remodeling-related ADAM8 ECM remodeling-related ADAM9 ECM remodeling-related ADAMTS1 ECM remodeling-related ADAMTS10 ECM remodeling-related ADAMTS12 ECM remodeling-related ADAMTS13 ECM remodeling-related ADAMTS14 ECM remodeling-related ADAMTS15 ECM remodeling-related ADAMTS16 ECM remodeling-related ADAMTS17 ECM remodeling-related ADAMTS18 ECM remodeling-related ADAMTS19 ECM remodeling-related ADAMTS2 ECM remodeling-related ADAMTS20 ECM remodeling-related ADAMTS3 ECM remodeling-related ADAMTS4 ECM remodeling-related ADAMTS5 ECM remodeling-related ADAMTS6 ECM remodeling-related ADAMTS7 ECM remodeling-related ADAMTS8 ECM remodeling-related ADAMTS9 ECM remodeling-related ADAMTSL1 ECM remodeling-related ADAMTSL2 ECM remodeling-related ADAMTSL3 ECM remodeling-related ADAMTSL4 ECM remodeling-related ADAMTSL5 ECM remodeling-related AGRIN ECM ALCAM Cell-cell adhesion ANGPT1 Soluble factors and receptors -

The Plasmin–Antiplasmin System: Structural and Functional Aspects
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Bern Open Repository and Information System (BORIS) Cell. Mol. Life Sci. (2011) 68:785–801 DOI 10.1007/s00018-010-0566-5 Cellular and Molecular Life Sciences REVIEW The plasmin–antiplasmin system: structural and functional aspects Johann Schaller • Simon S. Gerber Received: 13 April 2010 / Revised: 3 September 2010 / Accepted: 12 October 2010 / Published online: 7 December 2010 Ó Springer Basel AG 2010 Abstract The plasmin–antiplasmin system plays a key Plasminogen activator inhibitors Á a2-Macroglobulin Á role in blood coagulation and fibrinolysis. Plasmin and Multidomain serine proteases a2-antiplasmin are primarily responsible for a controlled and regulated dissolution of the fibrin polymers into solu- Abbreviations ble fragments. However, besides plasmin(ogen) and A2PI a2-Antiplasmin, a2-Plasmin inhibitor a2-antiplasmin the system contains a series of specific CHO Carbohydrate activators and inhibitors. The main physiological activators EGF-like Epidermal growth factor-like of plasminogen are tissue-type plasminogen activator, FN1 Fibronectin type I which is mainly involved in the dissolution of the fibrin K Kringle polymers by plasmin, and urokinase-type plasminogen LBS Lysine binding site activator, which is primarily responsible for the generation LMW Low molecular weight of plasmin activity in the intercellular space. Both activa- a2M a2-Macroglobulin tors are multidomain serine proteases. Besides the main NTP N-terminal peptide of Pgn physiological inhibitor a2-antiplasmin, the plasmin–anti- PAI-1, -2 Plasminogen activator inhibitor 1, 2 plasmin system is also regulated by the general protease Pgn Plasminogen inhibitor a2-macroglobulin, a member of the protease Plm Plasmin inhibitor I39 family. -

Serpins—From Trap to Treatment
MINI REVIEW published: 12 February 2019 doi: 10.3389/fmed.2019.00025 SERPINs—From Trap to Treatment Wariya Sanrattana, Coen Maas and Steven de Maat* Department of Clinical Chemistry and Haematology, University Medical Center Utrecht, Utrecht University, Utrecht, Netherlands Excessive enzyme activity often has pathological consequences. This for example is the case in thrombosis and hereditary angioedema, where serine proteases of the coagulation system and kallikrein-kinin system are excessively active. Serine proteases are controlled by SERPINs (serine protease inhibitors). We here describe the basic biochemical mechanisms behind SERPIN activity and identify key determinants that influence their function. We explore the clinical phenotypes of several SERPIN deficiencies and review studies where SERPINs are being used beyond replacement therapy. Excitingly, rare human SERPIN mutations have led us and others to believe that it is possible to refine SERPINs toward desired behavior for the treatment of enzyme-driven pathology. Keywords: SERPIN (serine proteinase inhibitor), protein engineering, bradykinin (BK), hemostasis, therapy Edited by: Marvin T. Nieman, Case Western Reserve University, United States INTRODUCTION Reviewed by: Serine proteases are the “workhorses” of the human body. This enzyme family is conserved Daniel A. Lawrence, throughout evolution. There are 1,121 putative proteases in the human body, and about 180 of University of Michigan, United States Thomas Renne, these are serine proteases (1, 2). They are involved in diverse physiological processes, ranging from University Medical Center blood coagulation, fibrinolysis, and inflammation to immunity (Figure 1A). The activity of serine Hamburg-Eppendorf, Germany proteases is amongst others regulated by a dedicated class of inhibitory proteins called SERPINs Paulo Antonio De Souza Mourão, (serine protease inhibitors). -

Anti-Mullerian-Hormone-Dependent Regulation of the Brain Serine-Protease Inhibitor Neuroserpin
Research Article 3357 Anti-Mullerian-hormone-dependent regulation of the brain serine-protease inhibitor neuroserpin Nathalie Lebeurrier 1,2,3,*, Séverine Launay 1,2,3,*, Richard Macrez 1,2,3, Eric Maubert 1,2,3, Hélène Legros 4, Arnaud Leclerc 5,6, Soazik P. Jamin 5,6, Jean-Yves Picard 5,6, Stéphane Marret 4, Vincent Laudenbach 4, Philipp Berger 7,‡, Peter Sonderegger 7, Carine Ali 1,2,3, Nathalie di Clemente 5,6, Denis Vivien 1,2,3,§ 1INSERM, INSERM U919, Serine Proteases and Pathophysiology of the neurovascular Unit (SP2U), Cyceron, 2CNRS, UMR CNRS 6232 Ci-NAPs ʻCenter for imaging Neurosciences and Applications to PathologieSʼ, Cyceron, 3University of Caen Basse-Normandie, Caen Cedex, F-14074 France 4INSERM-Avenir, Institute for Biomedical Research, IFRMP23, University of Rouen & Department of Neonatal Pediatrics and Intensive Care, Rouen University Hospital, Rouen, F-76183, France 5INSERM, U782, 6University of Paris-Sud, UMR-S0782, Clamart, F-92140 7Department of Biochemistry, University of Zurich, Zurich, CH-8057, Switzerland *These authors contributed equally to this work ‡Present address: ETH Zurich, Institute of Cell Biology, Zurich, CH-8093, Switzerland §Author for correspondence (e-mail: [email protected]) Accepted 30 June 2008 Journal of Cell Science 121, 000-000 Published by The Company of Biologists 2008 doi:10.1242/jcs.031872 Summary The balance between tissue-type plasminogen activator (tPA) neuroserpin in the brain of AMHR-II-deficient mice. and one of its inhibitors, neuroserpin, has crucial roles in the Interestingly, as previously demonstrated for neuroserpin, central nervous system, including the control of neuronal AMH protects neurons against N-methyl-D-aspartate (NMDA)- migration, neuronal plasticity and neuronal death. -

Alternative Signaling Pathways Triggered by Different Mechanisms of Serpin Endocytosis
ALTERNATIVE SIGNALING PATHWAYS TRIGGERED BY DIFFERENT MECHANISMS OF SERPIN ENDOCYTOSIS INAUGURALDISSERTATION zur Erlangung der Würde Doktors der Philosophie Vorgelegt der Philosophisch-Naturwissenschaftlichen Fakultät Der Universität Basel von Xiaobiao Li aus Nanning, China Friedrich Miescher Institute, Basel, 2006 Genehmigt von der Philosophisch-Naturwissenschaftlichen Fakultät auf Antrag der Herren Prof. Dr. Denis Monard, PD Dr. Jan Hofsteenge und Frau Dr. Ariane de Agostini. Basel, den 18 March 2006. Prof. Dr. Hans-Jakob Wirz 2 Acknowledgments: It is a pleasure for me to express my gratitude to those who contributed to this work. In the first place, I would like to thank Prof. Dr. Denis Monard, who gave me the opportunity to work in his laboratory and the freedom to develop my projects. His support was essential for completion of my projects and my scientific development. I would also like to thank the members of my PhD thesis committee, PD Dr. Jan Hofsteenge and Dr. Ariane de Agostini, for their comments and help during the course of the thesis. I am grateful to my colleagues at FMI, especially in the lab, for their helpful discussions, suggestions, technical assistance, and their kindly company over all these years. In particular, I would like to thank Ulrich Hengst and Mirna Kvajo for helping me to get started, Catherine Vaillant for some valuable suggestions, Anne-Catherine Feutz and Sabrina Taieb for their continuous encouragement. I am especially grateful to all my friends for their friendship, which was a great support to me, especially at the time when I experienced difficulty during these years. The most special thank goes to my family, who has always encouraged me in pursuing my professional interest, supported me with their love. -

Targeting Plasminogen Activator Inhibitor-1 Inhibits Angiogenesis and Tumor Growth in a Human Cancer Xenograft Model
Author Manuscript Published OnlineFirst on September 26, 2013; DOI: 10.1158/1535-7163.MCT-13-0500 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Targeting plasminogen activator inhibitor-1 inhibits angiogenesis and tumor growth in a human cancer xenograft model Evan Gomes-Giacoia1, Makito Miyake1, Steve Goodison1,2, Charles J. Rosser1,2 Authors’ Affiliations: 1Cancer Research Institute, MD Anderson Cancer Center, Orlando, Florida, USA 2Nonagen Bioscience Corp, Orlando, Florida, USA Running title: Targeting PAI-1 inhibits tumor growth Key words: angiogenesis, apoptosis, cancer, plasminogen activator inhibitor -1, therapy, tiplaxtinin Abbreviation list: PAI-1, plasminogen activator inhibitor-1; uPA, urokinase-type plasminogen activator; Scr, scrambled; IHC, Immunohistochemistry, MVD, Microvessel density; PI, Proliferative index; AI, Apoptotic index; tPA, tissue-type plasminogen activator Grant support: This work was funded by the James and Esther King Biomedical Team Science Project 1KT-01 (C.J. Rosser). Disclosure of potential conflicts of interest: S Goodison and CJ Rosser are officers in Nonagen Bioscience Corporation (NBC). Correspondence author: Charles J. Rosser, MD, MBA, FACS Cancer Research Institute MD Anderson Cancer Center 6900 Lake Nona Blvd Orlando, FL USA 32827 Telephone: +1 (407) 266 7401 Fax: +1 (407) 266 7402 Email: [email protected] Word count: 5,189 Total number of Tables and Figures: 5 Total number of Supplemental Figures: 5 1 Downloaded from mct.aacrjournals.org on October 2, 2021. © 2013 American Association for Cancer Research. Author Manuscript Published OnlineFirst on September 26, 2013; DOI: 10.1158/1535-7163.MCT-13-0500 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. -

Serpins in Hemostasis As Therapeutic Targets for Bleeding Or Thrombotic Disorders
MINI REVIEW published: 07 January 2021 doi: 10.3389/fcvm.2020.622778 Serpins in Hemostasis as Therapeutic Targets for Bleeding or Thrombotic Disorders Elsa P. Bianchini 1*, Claire Auditeau 1, Mahita Razanakolona 1, Marc Vasse 1,2 and Delphine Borgel 1,3 1 HITh, UMR_S1176, Institut National de la Santé et de la Recherche Médicale, Université Paris-Saclay, Le Kremlin-Bicêtre, France, 2 Service de Biologie Clinique, Hôpital Foch, Suresnes, France, 3 Laboratoire d’Hématologie Biologique, Hôpital Necker, APHP, Paris, France Edited by: Bleeding and thrombotic disorders result from imbalances in coagulation or fibrinolysis, Marie-Christine Bouton, respectively. Inhibitors from the serine protease inhibitor (serpin) family have a key role Institut National de la Santé et de la in regulating these physiological events, and thus stand out as potential therapeutic Recherche Médicale (INSERM), France targets for modulating fibrin clot formation or dismantling. Here, we review the diversity Reviewed by: of serpin-targeting strategies in the area of hemostasis, and detail the suggested use of Xin Huang, modified serpins and serpin inhibitors (ranging from small-molecule drugs to antibodies) University of Illinois at Chicago, United States to treat or prevent bleeding or thrombosis. Martine Jandrot-Perrus, Keywords: serpin (serine proteinase inhibitor), antithrombin (AT), protein Z-dependent protease inhibitor (ZPI), Institut National de la Santé et de la plasminogen activator inhibitor 1 (PAI-1), therapy, protease nexin I (PN-1) Recherche Médicale (INSERM), France *Correspondence: INTRODUCTION Elsa P. Bianchini elsa.bianchini@ universite-paris-saclay.fr Coagulation (the formation of a solid fibrin clot at the site of vessel injury, to stop bleeding) and fibrinolysis (the disaggregation of a clot, to prevent the obstruction of blood flow) are Specialty section: interconnected pathways that both help to maintain the hemostatic balance. -

View Preprint
A peer-reviewed version of this preprint was published in PeerJ on 16 June 2015. View the peer-reviewed version (peerj.com/articles/1026), which is the preferred citable publication unless you specifically need to cite this preprint. Kumar A. 2015. Bayesian phylogeny analysis of vertebrate serpins illustrates evolutionary conservation of the intron and indels based six groups classification system from lampreys for ∼500 MY. PeerJ 3:e1026 https://doi.org/10.7717/peerj.1026 Bayesian phylogeny analysis of vertebrate serpins illustrates evolutionary conservation of the intron and indels based six groups classification system from lampreys for ~500 MY Abhishek Kumar The serpin superfamily is characterized by proteins that fold into a conserved tertiary structure and exploits a sophisticated and irreversible suicide-mechanism of inhibition. Vertebrate serpins can be conveniently classified into six groups (V1-V6), based on three independent biological features - genomic organization, diagnostic amino acid sites and rare indels. However, this classification system was based on the limited number of mammalian genomes available. In this study, several non-mammalian genomes are used to validate this classification system, using the powerful Bayesian phylogenetic method. PrePrints This method supports the intron and indel based vertebrate classification and proves that serpins have been maintained from lampreys to humans for about 500 MY. Lampreys have less than 10 serpins, which expanded into 36 serpins in humans. The two expanding groups V1 and V2 have SERPINB1/SERPINB6 and SERPINA8/SERPIND1 as the ancestral serpins, respectively. Large clusters of serpins are formed by local duplications of these serpins in tetrapod genomes. Interestingly, the ancestral HCII/SERPIND1 locus (nested within PIK4CA) possesses group V4 serpin (A2APL1, homolog of α2-AP/SERPINF2 ) of lampreys; hence, pointing to the fact that group V4 might have originated from group V2.