Benign Extramedullary Myeloid Proliferations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Skin and Breast Disease in the Differential Diagnosis of Chest Pain
Skin and breast disease in the differential diagnosis of chest pain Author Muir, Jim, Yelland, Michael Published 2010 Journal Title Medical Clinics of North America DOI https://doi.org/10.1016/j.mcna.2010.01.006 Copyright Statement © 2010 Elsevier. This is the author-manuscript version of this paper. Reproduced in accordance with the copyright policy of the publisher. Please refer to the journal's website for access to the definitive, published version. Downloaded from http://hdl.handle.net/10072/33712 Griffith Research Online https://research-repository.griffith.edu.au ARTICLE IN PRESS 1 2 Skin and Breast 3 4 Disease in the 5 6 Differential 7 8 Diagnosis of 9 10 Chest Pain 11 12 a, b ½Q2½ Q3 Jim Muir *, Michael Yelland ½Q4½ Q5 KEYWORDS 13 14 Chest pain Skin diseases Herpes zoster PROOF 15 Breast Neoplasm 16 17 18 Pain is not a symptom commonly associated with skin disease. This is especially so 19 when considering the known skin problems that have a presenting symptom of chest 20 pain that could potentially be confused with chest pain from other causes. 21 22 PAINFUL SKIN CONDITIONS 23 24 Several extremely painful and tender skin conditions present with dramatic clinical 25 signs. Inflammatory disorders such as pyoderma gangrenosum, skin malignancies, 26 both primary and secondary, acute bacterial infections such as erysipelas or cellulitis, 27 and multiple other infections are commonly extremely painful and tender. As these 28 conditions manifest with obvious skin signs such as swelling, erythema, localized 29 tenderness, fever, lymphangitis, and lymphadenopathy, there is little chance of misdi- 30 agnosis of symptoms as caused by anything other than a cutaneous pathology. -

Benign Tumors and Tumor-Like Lesions of the Vulva
Please do not remove this page Benign Tumors and Tumor-like Lesions of the Vulva Heller, Debra https://scholarship.libraries.rutgers.edu/discovery/delivery/01RUT_INST:ResearchRepository/12643402930004646?l#13643525330004646 Heller, D. (2015). Benign Tumors and Tumor-like Lesions of the Vulva. In Clinical Obstetrics & Gynecology (Vol. 58, Issue 3, pp. 526–535). Rutgers University. https://doi.org/10.7282/T3RN3B2N This work is protected by copyright. You are free to use this resource, with proper attribution, for research and educational purposes. Other uses, such as reproduction or publication, may require the permission of the copyright holder. Downloaded On 2021/09/23 14:56:57 -0400 Heller DS Benign Tumors and Tumor-like lesions of the Vulva Debra S. Heller, MD From the Department of Pathology & Laboratory Medicine, Rutgers-New Jersey Medical School, Newark, NJ Address Correspondence to: Debra S. Heller, MD Dept of Pathology-UH/E158 Rutgers-New Jersey Medical School 185 South Orange Ave Newark, NJ, 07103 Tel 973-972-0751 Fax 973-972-5724 [email protected] Funding: None Disclosures: None 1 Heller DS Abstract: A variety of mass lesions may affect the vulva. These may be non-neoplastic, or represent benign or malignant neoplasms. A review of benign mass lesions and neoplasms of the vulva is presented. Key words: Vulvar neoplasms, vulvar diseases, vulva 2 Heller DS Introduction: A variety of mass lesions may affect the vulva. These may be non-neoplastic, or represent benign or malignant neoplasms. Often an excision is required for both diagnosis and therapy. A review of the more commonly encountered non-neoplastic mass lesions and benign neoplasms of the vulva is presented. -

A Single Case Report of Granular Cell Tumor of the Tongue Successfully Treated Through 445 Nm Diode Laser
healthcare Case Report A Single Case Report of Granular Cell Tumor of the Tongue Successfully Treated through 445 nm Diode Laser Maria Vittoria Viani 1,*, Luigi Corcione 1, Chiara Di Blasio 2, Ronell Bologna-Molina 3 , Paolo Vescovi 1 and Marco Meleti 1 1 Department of Medicine and Surgery, University of Parma, 43126 Parma, Italy; [email protected] (L.C.); [email protected] (P.V.); [email protected] (M.M.) 2 Private practice, Centro Medico Di Blasio, 43121 Parma; Italy; [email protected] 3 Faculty of Dentistry, University of the Republic, 14600 Montevideo, Uruguay; [email protected] * Correspondence: [email protected] Received: 10 June 2020; Accepted: 11 August 2020; Published: 13 August 2020 Abstract: Oral granular cell tumor (GCT) is a relatively rare, benign lesion that can easily be misdiagnosed. Particularly, the presence of pseudoepitheliomatous hyperplasia might, in some cases, lead to the hypothesis of squamous cell carcinoma. Surgical excision is the treatment of choice. Recurrence has been reported in up to 15% of cases treated with conventional surgery. Here, we reported a case of GCT of the tongue in a young female patient, which was successfully treated through 445 nm diode laser excision. Laser surgery might reduce bleeding and postoperative pain and may be associated with more rapid healing. Particularly, the vaporization effect on remnant tissues could eliminate GCT cells on the surgical bed, thus hypothetically leading to a lower rate of recurrence. In the present case, complete healing occurred in 1 week, and no recurrence was observed after 6 months. Laser surgery also allows the possibility to obtain second intention healing. -

Soft Tissue Cytopathology: a Practical Approach Liron Pantanowitz, MD
4/1/2020 Soft Tissue Cytopathology: A Practical Approach Liron Pantanowitz, MD Department of Pathology University of Pittsburgh Medical Center [email protected] What does the clinician want to know? • Is the lesion of mesenchymal origin or not? • Is it begin or malignant? • If it is malignant: – Is it a small round cell tumor & if so what type? – Is this soft tissue neoplasm of low or high‐grade? Practical diagnostic categories used in soft tissue cytopathology 1 4/1/2020 Practical approach to interpret FNA of soft tissue lesions involves: 1. Predominant cell type present 2. Background pattern recognition Cell Type Stroma • Lipomatous • Myxoid • Spindle cells • Other • Giant cells • Round cells • Epithelioid • Pleomorphic Lipomatous Spindle cell Small round cell Fibrolipoma Leiomyosarcoma Ewing sarcoma Myxoid Epithelioid Pleomorphic Myxoid sarcoma Clear cell sarcoma Pleomorphic sarcoma 2 4/1/2020 CASE #1 • 45yr Man • Thigh mass (fatty) • CNB with TP (DQ stain) DQ Mag 20x ALT –Floret cells 3 4/1/2020 Adipocytic Lesions • Lipoma ‐ most common soft tissue neoplasm • Liposarcoma ‐ most common adult soft tissue sarcoma • Benign features: – Large, univacuolated adipocytes of uniform size – Small, bland nuclei without atypia • Malignant features: – Lipoblasts, pleomorphic giant cells or round cells – Vascular myxoid stroma • Pitfalls: Lipophages & pseudo‐lipoblasts • Fat easily destroyed (oil globules) & lost with preparation Lipoma & Variants . Angiolipoma (prominent vessels) . Myolipoma (smooth muscle) . Angiomyolipoma (vessels + smooth muscle) . Myelolipoma (hematopoietic elements) . Chondroid lipoma (chondromyxoid matrix) . Spindle cell lipoma (CD34+ spindle cells) . Pleomorphic lipoma . Intramuscular lipoma Lipoma 4 4/1/2020 Angiolipoma Myelolipoma Lipoblasts • Typically multivacuolated • Can be monovacuolated • Hyperchromatic nuclei • Irregular (scalloped) nuclei • Nucleoli not typically seen 5 4/1/2020 WD liposarcoma Layfield et al. -

Adenomatoid Tumor of the Skin: Differential Diagnosis of an Umbilical Erythematous Plaque
Title: Adenomatoid tumor of the skin: differential diagnosis of an umbilical erythematous plaque Keywords: Adenomatoid tumor, skin, umbilicus Short title: Adenomatoid tumor of the skin Authors: Ingrid Ferreira1, Olivier De Lathouwer2, Hugues Fierens3, Anne Theunis1, Josette André1, Nicolas de Saint Aubain3 1Dermatopathology laboratory, Department of Dermatology, Saint-Pierre University Hospital, Université Libre de Bruxelles, Brussels, Belgium. 2Department of Plastic surgery, Centre Hospitalier Interrégional Edith Cavell, Waterloo, Belgium. 3Department of Dermatology, Saint-Jean Hospital, Brussels, Belgium. 4Department of Pathology, Jules Bordet Institute, Université Libre de Bruxelles, Brussels, Belgium. Acknowledgements: None Corresponding author: Ingrid Ferreira This article has been accepted for publication and undergone full peer review but has not been through the copyediting, typesetting, pagination and proofreading process which may lead to differences between this version and the Version of Record. Please cite this article as doi: 10.1111/cup.13872 This article is protected by copyright. All rights reserved. Abstract Adenomatoid tumors are benign tumors of mesothelial origin that are usually encountered in the genital tract. Although they have been observed in other organs, the skin appears to be a very rare location with only one case reported in the literature to our knowledge. We report a second case of an adenomatoid tumor, arising in the umbilicus of a 44-year-old woman. The patient presented with an 8 months old erythematous and firm plaque under the umbilicus. A skin biopsy showed numerous microcystic spaces dissecting a fibrous stroma and being lined by flattened to cuboidal cells with focal intraluminal papillary formation. This poorly known diagnosis constitutes a diagnostic pitfall for dermatopathologists and dermatologists, and could be misdiagnosed as other benign or malignant entities. -

The Health-Related Quality of Life of Sarcoma Patients and Survivors In
Cancers 2020, 12 S1 of S7 Supplementary Materials The Health-Related Quality of Life of Sarcoma Patients and Survivors in Germany—Cross-Sectional Results of A Nationwide Observational Study (PROSa) Martin Eichler, Leopold Hentschel, Stephan Richter, Peter Hohenberger, Bernd Kasper, Dimosthenis Andreou, Daniel Pink, Jens Jakob, Susanne Singer, Robert Grützmann, Stephen Fung, Eva Wardelmann, Karin Arndt, Vitali Heidt, Christine Hofbauer, Marius Fried, Verena I. Gaidzik, Karl Verpoort, Marit Ahrens, Jürgen Weitz, Klaus-Dieter Schaser, Martin Bornhäuser, Jochen Schmitt, Markus K. Schuler and the PROSa study group Includes Entities We included sarcomas according to the following WHO classification. - Fletcher CDM, World Health Organization, International Agency for Research on Cancer, editors. WHO classification of tumours of soft tissue and bone. 4th ed. Lyon: IARC Press; 2013. 468 p. (World Health Organization classification of tumours). - Kurman RJ, International Agency for Research on Cancer, World Health Organization, editors. WHO classification of tumours of female reproductive organs. 4th ed. Lyon: International Agency for Research on Cancer; 2014. 307 p. (World Health Organization classification of tumours). - Humphrey PA, Moch H, Cubilla AL, Ulbright TM, Reuter VE. The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs—Part B: Prostate and Bladder Tumours. Eur Urol. 2016 Jul;70(1):106–19. - World Health Organization, Swerdlow SH, International Agency for Research on Cancer, editors. WHO classification of tumours of haematopoietic and lymphoid tissues: [... reflects the views of a working group that convened for an Editorial and Consensus Conference at the International Agency for Research on Cancer (IARC), Lyon, October 25 - 27, 2007]. 4. ed. -
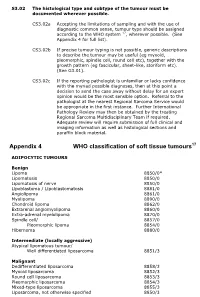
Appendix 4 WHO Classification of Soft Tissue Tumours17
S3.02 The histological type and subtype of the tumour must be documented wherever possible. CS3.02a Accepting the limitations of sampling and with the use of diagnostic common sense, tumour type should be assigned according to the WHO system 17, wherever possible. (See Appendix 4 for full list). CS3.02b If precise tumour typing is not possible, generic descriptions to describe the tumour may be useful (eg myxoid, pleomorphic, spindle cell, round cell etc), together with the growth pattern (eg fascicular, sheet-like, storiform etc). (See G3.01). CS3.02c If the reporting pathologist is unfamiliar or lacks confidence with the myriad possible diagnoses, then at this point a decision to send the case away without delay for an expert opinion would be the most sensible option. Referral to the pathologist at the nearest Regional Sarcoma Service would be appropriate in the first instance. Further International Pathology Review may then be obtained by the treating Regional Sarcoma Multidisciplinary Team if required. Adequate review will require submission of full clinical and imaging information as well as histological sections and paraffin block material. Appendix 4 WHO classification of soft tissue tumours17 ADIPOCYTIC TUMOURS Benign Lipoma 8850/0* Lipomatosis 8850/0 Lipomatosis of nerve 8850/0 Lipoblastoma / Lipoblastomatosis 8881/0 Angiolipoma 8861/0 Myolipoma 8890/0 Chondroid lipoma 8862/0 Extrarenal angiomyolipoma 8860/0 Extra-adrenal myelolipoma 8870/0 Spindle cell/ 8857/0 Pleomorphic lipoma 8854/0 Hibernoma 8880/0 Intermediate (locally -

Subcutaneous Hemangiosarcoma: the First Report in Maltese Dog
pISSN 1598-298X / eISSN 2384-0749 J Vet Clin 36(3) : 169-171 (2019) http://dx.doi.org/10.17555/jvc.2019.06.36.3.169 Subcutaneous Hemangiosarcoma: The First Report in Maltese Dog Ha-Jung Kim, Eun-Taek Hong and Guk-Hyun Suh1 Department of Veterinary Internal Medicine, College of Veterinary Medicine, Chonnam National University, Gwangju 500-757, Korea (Received: March 13, 2019 / Accepted: May 09, 2019) Abstract : Subcutanous hemangiosarcoma is rare malignant condition in dogs. An eleven-year-old neutered male Maltese was presented with multicentric cutaneous hemorrhagic nodules followed by lethargy. The patient showed regenerative anemia and thrombocytopenia with skyrocketing D-dimer, indicating that he had disseminated intravascular coagulation (DIC) on progress. Fine needle aspiration, histopathology, X-ray, and computed tomographic scanning ultimately diagnosed this patient as subcutaneous hemangiosarcoma with disseminated metastasis to the body. Unfortunately, the dog died due to side effects of anti-thrombotic therapy for DIC. This case report described a rare subcutaneous hemangiosarcoma in a Maltese dog. Key words : dog, skin neoplasms, hemangiosarcoma, disseminated intravascular coagulation, histopathology. Introduction had a 2 month history of multicentric cutaneous hemor- rhagic nodules initiated from his dorsum (Fig 1A and C). Hemangiosarcoma (a.k.a. malignant hemangioendotheli- There were no specific findings from skin examination such oma or angisarcoma) is an outbreak of tumor from endothe- as scraping or taping, and no bacteria or fungi were cultured lial cells which occurs more frequently in dogs than any from the lesions. On physical examination, he had a pale other species, accounting for 0.3% to 2.0% of all tumors in mucous membrane with bilateral ocular hemorrhage (Fig dogs with a high fatality rate (1,7). -
Atypical Fibroids
Hereditary leiomyomatosis and renal cell cancer: Cutaneous lesions & atypical fibroids The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation Bortoletto, Pietro, Jennifer L. Lindsey, Liping Yuan, Bradley J. Quade, Antonio R. Gargiulo, Cynthia C. Morton, Elizabeth A. Stewart, and Raymond M. Anchan. 2017. “Hereditary leiomyomatosis and renal cell cancer: Cutaneous lesions & atypical fibroids.” Case Reports in Women's Health 15 (1): 31-34. doi:10.1016/ j.crwh.2017.06.004. http://dx.doi.org/10.1016/j.crwh.2017.06.004. Published Version doi:10.1016/j.crwh.2017.06.004 Citable link http://nrs.harvard.edu/urn-3:HUL.InstRepos:35982080 Terms of Use This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http:// nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA Case Reports in Women's Health 15 (2017) 31–34 Contents lists available at ScienceDirect Case Reports in Women's Health journal homepage: www.elsevier.com/locate/crwh Hereditary leiomyomatosis and renal cell cancer: Cutaneous MARK lesions & atypical fibroids Pietro Bortolettoa,b,c,1, Jennifer L. Lindseya,b,1, Liping Yuand, Bradley J. Quadec,d, Antonio R. Gargiuloa,b,c, Cynthia C. Mortonb,c,d,e,f, Elizabeth A. Stewartg, ⁎ Raymond M. Anchana,b,c, a Division of Reproductive Endocrinology and Infertility, Boston, MA, USA b Department of Obstetrics, Gynecology and Reproductive Biology, -

Radiation-Associated Synovial Sarcoma
Radiation-Associated Synovial Sarcoma: Clinicopathologic and Molecular Analysis of Two Cases Jean-François Egger, M.D., Jean-Michel Coindre, M.D., Jean Benhattar, Ph.D., Philippe Coucke, M.D., Louis Guillou, M.D. University Institute of Pathology (J-FE, JB, LG) and Department of Radiooncology, University Hospital (PC), Lausanne, Switzerland; Bergonié Institute and University of Bordeaux II (J-MC), Bordeaux, France region, or viscera (1, 2). SS bears the t(X;18) (SYT- Development of a soft-tissue sarcoma is an infre- SSX) reciprocal translocation that seems to be spe- quent but well-known long-term complication of cific for this tumor type and can be routinely de- radiotherapy. Malignant fibrous histiocytomas, ex- tected in paraffin-embedded tissue using the traskeletal osteosarcomas, fibrosarcomas, malig- reverse transcriptase–polymerase chain reaction nant peripheral nerve sheath tumors, and angiosar- (RT-PCR; 3–6). Radiation-associated sarcomas are comas are most frequently encountered. Radiation- an infrequent but well-known long-term complica- associated synovial sarcomas are exceptional. We tion of radiotherapy (7–16). They occur in about report the clinicopathologic, immunohistochemi- 1/1000 patients who have undergone radiation cal, and molecular features of two radiation- therapy (7–11). Radiation-associated sarcomas are associated synovial sarcomas. One tumor developed defined as sarcomas arising in a previously irradi- in a 42-year-old female 17 years after external irra- ated field after a latency period of Ն2 years (12). diation was given for breast carcinoma; the other They usually show a more aggressive clinical course occurred in a 34-year-old female who was irradiated associated with shortened patient survival as com- at the age of 7 years for a nonneoplastic condition of pared with sporadic sarcomas (9–12, 14). -

Dermatofibrosarcoma Protuberans of the Parotid Gland -A Case Report
The Korean Journal of Pathology 2004; 38: 276-9 Dermatofibrosarcoma Protuberans of the Parotid Gland -A Case Report - Ok-Jun Lee∙David Y. Pi∙ Dermatofibrosarcoma protuberans (DFSP) typically presents during the early or mid-adult life, Daniel H. Jo∙Kyung-Ja Cho and the most common site of origin is the skin on the trunk and proximal extremities. DFSP of Sang Yoon Kim1∙Jae Y. Ro the parotid gland is extremely rare and only one case has been reported in the literature. We present here a case of a 30-year-old woman with DFSP occurring in the parotid gland, and we Departments of Pathology and discuss the differential diagnosis. The patient is alive and doing well one year after her operation. 1Otolaryngology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea Received : January 27, 2004 Accepted : July 5, 2004 Corresponding Author Jae Y. Ro, M.D. Department of Pathology, University of Ulsan College of Medicine, Asan Medical Center, 388-1 Pungnap-dong, Songpa-gu, Seoul 138-736, Korea Tel: 02-3010-4550 Fax: 02-472-7898 E-mail: [email protected] Key Words : Dermatofibrosarcoma Protuberans-Parotid Gland Epithelial tumors make up the majority of salivary gland neo- CASE REPORT plasms, while mesenchymal tumors of this organ are uncommon. Dermatofibrosarcoma protuberans (DFSP) of the salivary gland A 30-year-old woman came to the Otolaryngology Clinic at is exremely rare and only one case has been reported in the parotid the Asan Medical Center with a 2-year history of a slowly enlarg- gland.1 ing mass inferior to the left angle of the mandible. -

Epssg NRSTS 2005
EpSSG NRSTS 2005 a protocol for Localized Non-Rhabdomyosarcoma Soft Tissue Sarcomas VERSION 1.1 SEPTEMBER 2009 EpSSG NRSTS 2005 protocol Version 1.1 Contents 1. Administrative organisation p. 3 1.1 Protocol sponsor p. 3 1.2 Protocol coordination p. 3 1.3 EpSSG and NRSTS 2005 structure p. 4 2. Abbreviations p.10 3. Summary p.11 3.1. Objectives p.12 3.2. Patients eligibility p.12 3.3. Patients stratification p.13 3.4. Pathology and Biology p.13 3.5. Statistical consideration p.13 3.6. Organisation of the study p.14 3.7. Datamanagement and analysis p.14 3.8. Ethical consideration p.14 4. Background p.16 4.1. References p.20 5. Study structure p.22 6. Patient eligibility p.22 7. Pre-treatment investigation p.23 7.1. Histological diagnosis p.23 7.2. Clinical assessment p.23 7.3. Laboratory investigations p.23 7.4. Radiological investigations p.24 7.5. Tumour measurements p.25 7.6. Lung lesions p.25 8. Staging system p.26 8.1. References p.26 9. Surgical guidelines p.27 9.1. Definitions p.27 9.2. Biopsy p.28 9.3. Primary resection p.29 9.4. Primary re-operation p.30 9.5. Secondary re-operation p.30 9.6. Reconstructive surgery and local control p.31 9.7. Lymph nodes p.31 9.8. Specific sites p.32 9.9. Surgery for relapse p.34 9.10. Marker clips p.34 9.11. Histology p.34 9.12. References p.34 10.