Maternal Use of Acid Reducers Before and During Pregnancy: Trends And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Appendix a Common Abbreviations Used in Medication
UNIVERSITY OF AMSTERDAM MASTERS THESIS Impact of Medication Grouping on Fall Risk Prediction in Elders: A Retrospective Analysis of MIMIC-III Critical Care Database Student: SRP Mentor: Noman Dormosh Dr. Martijn C. Schut Student No. 11412682 – SRP Tutor: Prof. dr. Ameen Abu-Hanna SRP Address: Amsterdam University Medical Center - Location AMC Department Medical Informatics Meibergdreef 9, 1105 AZ Amsterdam Practice teaching period: November 2018 - June 2019 A thesis submitted in fulfillment of the requirements for the degree of Master of Medical Informatics iii Abstract Background: Falls are the leading cause of injury in elderly patients. Risk factors for falls in- cluding among others history of falls, old age, and female gender. Research studies have also linked certain medications with an increased risk of fall in what is called fall-risk-increasing drugs (FRIDs), such as psychotropics and cardiovascular drugs. However, there is a lack of consistency in the definitions of FRIDs between the studies and many studies did not use any systematic classification for medications. Objective: The aim of this study was to investigate the effect of grouping medications at different levels of granularity of a medication classification system on the performance of fall risk prediction models. Methods: This is a retrospective analysis of the MIMIC-III cohort database. We created seven prediction models including demographic, comorbidity and medication variables. Medica- tions were grouped using the anatomical therapeutic chemical classification system (ATC) starting from the most specific scope of medications and moving up to the more generic groups: one model used individual medications (ATC level 5), four models used medication grouping at levels one, two, three and four of the ATC and one model did not include med- ications. -

Clinical Indications for Proton Pump Inhibitors and Tapering Information When Indicated
Clinical Indications for Proton Pump Inhibitors and Tapering Information When Indicated MacKenzie Crist, Pharm.D. Candidate 2017 Nabila Ahmed -Sarwar, Pharm.D, BCPS, CDE October 2016 Appropriate indications for PPIs Treatment Recommendations for GERD ● Initial eight-week course of therapy Try to lower dose, as needed therapy, or Short-Term Treatment Long-Term Treatment intermittent therapy ● ○ ● GERD ● Refractory GERD Refractory GERD—No response to PPI therapy after two to ● Gastric and duodenal ● Erosive esophagitis three months (needs GI consult and endoscopy) ulcers ● Barrett’s esophagus Add a bedtime H2 blocker if nocturnal symptoms ● H. pylori co-therapy ● History of NSAID induced Double the dose ○ bleeding ulcers Concerns with Chronic PPI Therapy ○ ● Chronic anticoagulation ● Clostridium difficile infections after a GI bleed ● Hypomagnesaemia ● NSAID or dual anti-platelet ● Increased fracture risk agent use* ● Acute interstitial nephritis (rare, idiopathic) ● Chronic kidney disease (weak observational data may be *presence of multiple risk factors: Age>65 years, high dose NSAID associated with dose and duration) therapy, PUD, concurrent corticosteroids or anticoagulants When PPIs Should Be Tapered and Not Abruptly Discontinued ● Patients who do not have any appropriate indications for continuing a PPI, but have been on a PPI for > six months, and asymptomatic at least 3 months ● Counsel patient on initial worsening of symptoms during tapering phase PPI Tapering Algorithm Step 1: Tapering Schedule Step 2: Management of Recurrence H2 Antagonist and antacids may be added while tapering for breakthrough symptoms Katz PO, Gerson LB, Vela MF. Guidelines for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterology. 2013; 108:308-328. Bundeff AW, Zaiken K. -

PHARMACEUTICAL APPENDIX to the TARIFF SCHEDULE 2 Table 1
Harmonized Tariff Schedule of the United States (2020) Revision 19 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2020) Revision 19 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names INN which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service CAS registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. -

Proton Pump Inhibitors
MEDICATION POLICY: Proton Pump Inhibitors Generic Name: Proton Pump Inhibitors Preferred: Esomeprazole (generic), Lansoprazole (generic), Omeprazole (generic), Therapeutic Class or Brand Name: Proton Pantoprazole (generic), and Rabeprazole Pump Inhibitors (generic) Applicable Drugs (if Therapeutic Class): Non-preferred: Aciphex® (rabeprazole), Esomeprazole (generic), Lansoprazole Dexilant® (dexlansoprazole), Nexium® (generic), Omeprazole (generic), Pantoprazole (esomeprazole), Not Medically Necessary: (generic), and Rabeprazole (generic). Omeprazole/Sodium Bicarbonate (generic), Aciphex® (rabeprazole), Dexilant® Zegerid® (omeprazole/sodium bicarbonate). (dexlansoprazole), Nexium® (esomeprazole), Prevacid® (lansoprazole), Prilosec® Date of Origin: 2/1/2013 (omeprazole), and Protonix® (pantoprazole). Date Last Reviewed / Revised: 12/23/2020 Omeprazole/Sodium Bicarbonate (generic), Zegerid® (omeprazole/sodium bicarbonate). Policy also applies to any other Proton Pump Inhibitors not listed. GPI Code: 4927002000, 4927002510, 4927004000, 4927006000, 4927007010, 4927007610, 4999600260 PRIOR AUTHORIZATION CRITERIA (May be considered medically necessary when criteria I and II are met) I. Documented diagnosis of one of the following A through G: A. Gastroesophageal reflux disease (GERD). B. Erosive esophagitis. C. Gastric ulcers. D. Risk reduction of NSAID-associated gastric ulcer. E. Duodenal ulcers. F. Eradication of H. pylori. G. Hypersecretory conditions II. Non-preferred PPIs require documented trials and failures of all generic PPIs. EXCLUSION -

Proton Pump Inhibitors Therapeutic Class Review (TCR) September 1, 2017 the Literature Review Is Current Through February 17, 2020
Proton Pump Inhibitors Therapeutic Class Review (TCR) September 1, 2017 The literature review is current through February 17, 2020. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage or retrieval system without the express written consent of Magellan Rx Management. All requests for permission should be mailed to: Magellan Rx Management Attention: Legal Department 6950 Columbia Gateway Drive Columbia, Maryland 21046 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended to be educational in nature and is intended to be used for informational purposes only. Send comments and suggestions to [email protected]. September 2017 Proprietary Information. Restricted Access – Do not disseminate or copy without approval. © 2004-2020 Magellan Rx Management. All rights reserved. -

DEXILANT DEXILANT Safely and Effectively
HIGHLIGHTS OF PRESCRIBING INFORMATION • Cutaneous and Systemic Lupus Erythematosus: Mostly cutaneous; These highlights do not include all the information needed to use new onset or exacerbation of existing disease; discontinue DEXILANT DEXILANT safely and effectively. See full prescribing information for and refer to specialist for evaluation. (5.5) DEXILANT. • Cyanocobalamin (Vitamin B12) Deficiency: Daily long-term use (e.g., DEXILANT (dexlansoprazole) delayed-release capsules, for oral use longer than 3 years) may lead to malabsorption or a deficiency of Initial U.S. Approval: 1995 (lansoprazole) cyanocobalamin. (5.6) • Hypomagnesemia: Reported rarely with prolonged treatment with ---------------------------RECENT MAJOR CHANGES----------------------------- PPIs. (5.7) Warnings and Precautions, Acute Tubulointerstitial Nephritis (5.2) 11/2020 • Interactions with Investigations for Neuroendocrine Tumors: Risk of Heart Valve Thickening in Pediatric Patients Increases in intragastric pH may result in hypergastrinemia and Less than Two Years of Age (5.11) 9/2020 enterochromaffin-like cell hyperplasia and increased chromogranin A levels which may interfere with diagnostic investigations for neuroendocrine tumors. (5.8, 7) ---------------------------INDICATIONS AND USAGE----------------------------- • Interaction with Methotrexate: Concomitant use with PPIs may DEXILANT is a proton pump inhibitor (PPI) indicated in patients 12 years elevate and/or prolong serum concentrations of methotrexate of age and older for: and/or its metabolite, possibly leading to toxicity. With high-dose • Healing of all grades of erosive esophagitis (EE). (1.1) methotrexate administration, consider a temporary withdrawal • Maintenance of healed EE and relief of heartburn. (1.2) of DEXILANT. (5.9, 7) • Treatment of symptomatic non-erosive gastroesophageal reflux • Fundic Gland Polyps: Risk increases with long-term use, especially disease (GERD). -

Proton Pump Inhibitors
Cigna National Formulary Coverage Policy Step Therapy Proton Pump Inhibitors Table of Contents Product Identifier(s) National Formulary Medical Necessity ................ 1 14530 Conditions Not Covered....................................... 2 Background .......................................................... 2 References .......................................................... 3 Revision History ................................................... 4 INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide utilization review services to clients and do not make coverage determinations. References to standard benefit plan language and coverage determinations do not apply to those clients. Coverage Policies are intended to provide guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please note, the terms of a customer’s particular benefit plan document [Group Service Agreement, Evidence of Coverage, Certificate of Coverage, Summary Plan Description (SPD) or similar plan document] may differ significantly from the standard benefit plans upon which these Coverage Policies are based. For example, a customer’s benefit plan document may contain a specific exclusion related to a topic addressed in a Coverage Policy. In the event of a conflict, a customer’s benefit plan document always supersedes the information in the Coverage Policies. In the absence of a controlling federal or state coverage mandate, benefits are ultimately determined by the terms of the applicable benefit plan document. Coverage determinations in each specific instance require consideration of 1) the terms of the applicable benefit plan document in effect on the date of service; 2) any applicable laws/regulations; 3) any relevant collateral source materials including Coverage Policies and; 4) the specific facts of the particular situation. -

New and Future Drug Development for Gastroesophageal Reflux Disease
J Neurogastroenterol Motil, Vol. 20 No. 1 January, 2014 pISSN: 2093-0879 eISSN: 2093-0887 http://dx.doi.org/10.5056/jnm.2014.20.1.6 JNM Journal of Neurogastroenterology and Motility Review New and Future Drug Development for Gastroesophageal Reflux Disease Carla Maradey-Romero and Ronnie Fass* The Esophageal and Swallowing Center, Division of Gastroenterology and Hepatology, MetroHealth Medical Center, Case Western Reserve University, Cleveland, Ohio, USA Medical therapy remains the most popular treatment for gastroesophageal reflux disease (GERD). Whilst interest in drug devel- opment for GERD has declined over the last few years primarily due to the conversion of most proton pump inhibitor (PPI)’s to generic and over the counter compounds, there are still numerous areas of unmet needs in GERD. Drug development has been focused on potent histamine type 2 receptor antagonist’s, extended release PPI’s, PPI combination, potassium-competitive acid blockers, transient lower esophageal sphincter relaxation reducers, prokinetics, mucosal protectants and esophageal pain modulators. It is likely that the aforementioned compounds will be niched for specific areas of unmet need in GERD, rather than compete with the presently available anti-reflux therapies. (J Neurogastroenterol Motil 2014;20:6-16) Key Words Erosive esophagitis; Gastroesophageal reflux; Heartburn; Proton pump inhibitors Most patients with GERD fall into 1 of 3 categories: non- erosive reflux disease (NERD), erosive esophagitis (EE), and Introduction Barrett’s esophagus (BE). The 2 main phenotypes of GERD, Gastroesophageal reflux disease (GERD) is a common con- NERD and EE, appear to have different pathophysiological and dition that develops when reflux of stomach contents cause trou- clinical characteristics. -

2 12/ 35 74Al
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date 22 March 2012 (22.03.2012) 2 12/ 35 74 Al (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 9/16 (2006.01) A61K 9/51 (2006.01) kind of national protection available): AE, AG, AL, AM, A61K 9/14 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, (21) International Application Number: DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, PCT/EP201 1/065959 HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, (22) International Filing Date: KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, 14 September 201 1 (14.09.201 1) ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PE, PG, PH, PL, PT, QA, RO, RS, RU, (25) Filing Language: English RW, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, (26) Publication Language: English TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: 61/382,653 14 September 2010 (14.09.2010) US (84) Designated States (unless otherwise indicated, for every kind of regional protection available): ARIPO (BW, GH, (71) Applicant (for all designated States except US): GM, KE, LR, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, NANOLOGICA AB [SE/SE]; P.O Box 8182, S-104 20 ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, Stockholm (SE). -
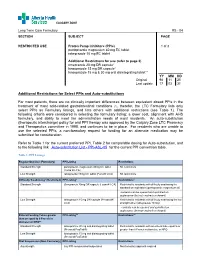
Additional Restrictions for Select Ppis and Auto-Substitutions for Most
CALGARY ZONE Long Term Care Formulary RS - 04 SECTION SUBJECT PAGE RESTRICTED USE Proton Pump Inhibitors (PPIs) 1 of 3 pantoprazole magnesium 40 mg EC tablet rabeprazole 10 mg EC tablet Additional Restrictions for use (refer to page 3) omeprazole 20 mg DR capsule* lansoprazole 15 mg DR capsule* lansoprazole 15 mg & 30 mg oral disintegrating tablet** _____________ YY MM DD Original 98 11 25 Last update 17 03 31 Additional Restrictions for Select PPIs and Auto-substitutions For most patients, there are no clinically important differences between equivalent dosed PPIs in the treatment of most acid-related gastrointestinal conditions (1), therefor, the LTC Formulary lists only select PPIs as Formulary listings, and lists others with additional restrictions (see Table 1). The following criteria were considered in selecting the formulary listing: a lower cost, alignment with AHS formulary, and ability to meet the administration needs of most residents. An auto-substitution (therapeutic interchange) policy for oral PPI therapy was approved by the Calgary Zone LTC Pharmacy and Therapeutics committee in 1998, and continues to be in place. For residents who are unable to use the selected PPIs, a non-formulary request for funding for an alternate medication may be submitted for consideration. Refer to Table 1 for the current preferred PPI, Table 2 for comparable dosing for Auto-substitution, and to the following link Auto-substitution List - PPI-ASL-05 for the current PPI conversion table. Table 1: PPI Listings Regular Oral Use (Formulary) PPI Listing -

DEXILANT (Dexlansoprazole) Delayed-Release Capsules for Oral Use
HIGHLIGHTS OF PRESCRIBING INFORMATION • Clostridium difficile associated diarrhea: PPI therapy may be These highlights do not include all the information needed to use associated with increased risk of Clostridium difficile DEXILANT safely and effectively. See full prescribing information for associated diarrhea. (5.4) DEXILANT. • Bone Fracture: Long-term and multiple daily dose PPI therapy may be associated with an increased risk for osteoporosis- DEXILANT (dexlansoprazole) delayed-release capsules for oral use. related fractures of the hip, wrist or spine. (5.5) Initial U.S. Approval: 1995 (lansoprazole) • Hypomagnesemia: Hypomagnesemia has been reported rarely with prolonged treatment with PPIs. (5.6) -------------------------------INDICATIONS AND USAGE------------------------ ------------------------------ ADVERSE REACTIONS ------------------------------ DEXILANT is a proton pump inhibitor (PPI) indicated for: Most commonly reported adverse reactions (≥2%): diarrhea, • Healing of all grades of erosive esophagitis (EE). (1.1) abdominal pain, nausea, upper respiratory tract infection, • Maintaining healing of EE and relief of heartburn. (1.2) vomiting, and flatulence. (6.1) • Treating heartburn associated with symptomatic non-erosive gastroesophageal reflux disease (GERD). (1.3) To report SUSPECTED ADVERSE REACTIONS, contact Takeda Pharmaceuticals America, Inc. at 1-877-TAKEDA-7 (1 ----------------------- DOSAGE AND ADMINISTRATION ---------------------- 877-825-3327) or FDA at 1-800-FDA-1088 or • Healing of EE: 60 mg once daily for up to 8 weeks. (2.1) www.fda.gov/medwatch. • Maintenance of healed EE: 30 mg once daily for up to 6 months. (2.1) • Symptomatic non-erosive GERD: 30 mg once daily for 4 weeks. (2.1) ------------------------------- DRUG INTERACTIONS ------------------------------ • Hepatic impairment: Consider 30 mg maximum daily dose for patients • Atazanavir and Nelfinavir: Do not co-administer with with moderate hepatic impairment (Child-Pugh Class B). -

DEXILANT (Dexlansoprazole) Label
HIGHLIGHTS OF PRESCRIBING INFORMATION DEXILANT SoluTab These highlights do not include all the information needed to use • Take at least 30 minutes before a meal. DEXILANT safely and effectively. See full prescribing information • Do not break or cut. for DEXILANT. • Place the tablet on the tongue, allow to disintegrate and swallow without water. Do not chew microgranules. DEXILANT (dexlansoprazole) delayed-release capsules, for oral • May also be swallowed whole with water. use • Avoid use of alcohol when taking DEXILANT SoluTab (7) DEXILANT SoluTab (dexlansoprazole) delayed-release orally • See full prescribing information for alternative administration disintegrating tablets, for oral use options. Initial U.S. Approval: 1995 (lansoprazole) ---------------------------RECENT MAJOR CHANGES-------------------------- --------------------- DOSAGE FORMS AND STRENGTHS -------------------- Indications and Usage (1) 01/2016 • Delayed-release capsules: 30 mg and 60 mg. (3) Dosage and Administration, Recommended Dose (2.1) 01/2016 • Delayed-release orally disintegrating tablets: 30 mg. (3) Dose Adjustment in Adults with Hepatic Impairment for Healing of EE (2.2) 01/2016 ------------------------------- CONTRAINDICATIONS ------------------------------ Dosage and Administration, Important Administration • Patients with known hypersensitivity to any component of the Information (2.3) 01/2016 formulation. (4) Contraindications (4) 01/2016 • Patients receiving rilpivirine-containing products. (4, 7) Warnings and Precautions, Interaction with Diagnostic