Health Labour Market Analysis: CHHATTISGARH
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

* RPO Guwahati Covers Five Other North-Eastern States Also at Present
* RPO Guwahati covers five other North-Eastern States also at present. **RPO Chandigarh covers parts of Punjab and Haryana. ***RPO Delhi covers parts of Haryana. @RPO Kolkata covers Sikkim and Tripura. ANNEXURE-III STATE-WISE LIST OF POST OFFICE PASSPORT SEVA KENDRAS (POPSKs) S.No. Locations State/UT Passport Office 1 Anantpur Andhra Pradesh Vijayawada 2 Bapatla Andhra Pradesh Vijayawada 3 Chittoor Andhra Pradesh Vijayawada 4 Gudivada Andhra Pradesh Vijayawada 5 Guntur Andhra Pradesh Vijayawada 6 Hindupur Andhra Pradesh Vijayawada 7 Kadappa Andhra Pradesh Vijayawada 8 Kodur Andhra Pradesh Vijayawada 9 Kurnool Andhra Pradesh Vijayawada 10 Nandyal Andhra Pradesh Vijayawada 11 Narasaraopet Andhra Pradesh Vijayawada 12 Nellore Andhra Pradesh Vijayawada 13 Ongole Andhra Pradesh Vijayawada 14 Amalapuram Andhra Pradesh Visakhapatnam 15 Eluru Andhra Pradesh Visakhapatnam 16 Kakinada Andhra Pradesh Visakhapatnam 17 Rajamundry Andhra Pradesh Visakhapatnam 18 Srikakulam Andhra Pradesh Visakhapatnam 19 Vizianagaram Andhra Pradesh Visakhapatnam 20 Yelamanchili Andhra Pradesh Visakhapatnam 21 Changlang Arunachal Pradesh Guwahati 22 Khonsa Arunachal Pradesh Guwahati 23 Barpeta Assam Guwahati 24 Dhubri Assam Guwahati 25 Dibrugarh Assam Guwahati 26 Goalpara Assam Guwahati 27 Golaghat Assam Guwahati 28 Jorhat Assam Guwahati 29 Karbi Anglong Assam Guwahati 30 Karimganj Assam Guwahati 31 Kokrajhar Assam Guwahati 32 Mangaldoi Assam Guwahati 33 Nawgong Assam Guwahati 34 North Lakhimpur Assam Guwahati 35 Silchar Assam Guwahati 36 Tezpur Assam Guwahati 37 Tinsukia -
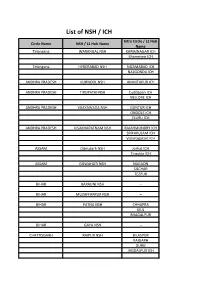
List of NSH / ICH Intra Circle / L2 Hub Circle Name NSH / L1 Hub Name Name Telangana WARANGAL NSH KARIMNAGAR ICH Khammam ICH
List of NSH / ICH Intra Circle / L2 Hub Circle Name NSH / L1 Hub Name Name Telangana WARANGAL NSH KARIMNAGAR ICH Khammam ICH Telangana HYDERABAD NSH NIZAMABAD ICH NALGONDA ICH ANDHRA PRADESH KURNOOL NSH ANANTAPUR ICH ANDHRA PRADESH TIRUPATHI NSH Cuddapah ICH NELLORE ICH ANDHRA PRADESH VIJAYAWADA NSH GUNTUR ICH ONGOLE ICH ELURU ICH ANDHRA PRADESH VISAKHAPATNAM NSH RAJAHMUNDRY ICH SRIKAKULAM ICH Vizianagaram ICH ASSAM Dibrugarh NSH Jorhat ICH Tinsukia ICH ASSAM GUWAHATI NSH NAGAON SILCHAR TEZPUR BIHAR BARAUNI NSH – BIHAR MUZAFFARPUR NSH – BIHAR PATNA NSH CHHAPRA KIUL BHAGALPUR BIHAR GAYA NSH – CHATTISGARH RAIPUR NSH BILASPUR RAIGARH DURG JAGDALPUR ICH DELHI DELHI NSH – GUJRAT AHMEDABAD NSH HIMATNAGAR MEHSANA PALANPUR BHAVNAGAR BHUJ Dhola ICH GUJRAT RAJKOT NSH JAMNAGAR JUNAGADH SURENDRANAGAR GUJRAT SURAT NSH VALSAD GUJRAT VADODARA NSH BHARUCH GODHARA ANAND HARYANA GURGAON NSH FARIDABAD ICH REWARI ICH HARYANA KARNAL NSH – HARYANA ROHTAK NSH HISAR ICH HARYANA AMBALA NSH SOLAN MANDI HIMACHAL PRADESH SHIMLA NSH SOLAN ICH HIMACHAL PRADESH PATHANKOT NSH KANGRA HAMIRPUR JAMMUKASHMIR JAMMU NSH – JAMMUKASHMIR SRINAGAR NSH – JHARKHAND JAMSHEDPUR NSH JHARKHAND RANCHI NSH DALTONGANJ HAZARIBAGH ROAD JHARKHAND DHANBAD NSH B. DEOGHAR KARNATAKA BENGALURU NSH BALLARI ICH TUMAKURU ICH KARNATAKA BELAGAVI NSH – KARNATAKA KALABURAGI NSH RAICHUR ICH KARNATAKA HUBBALLI-DHARWAD NSH BAGALKOT ICH KUMTA ICH VIJAYAPURA ICH KARNATAKA MANGALURU NSH – KARNATAKA MYSURU NSH – KARNATAKA ARSIKERE NSH – KERALA KOCHI NSH Kottayam ICH KERALA THRISSUR PALAKKAD ICH KERALA TRIVANDRUM -

Raigarh, Chhattisgarh
District Profile Raigarh, Chhattisgarh Raigarh is a major district in the state of Chhattisgarh in India. The headquarters of the district is located in the city of Raigarh. The total area of the district is 7086 sq. km. Raigarh district is divided into 10 Tehsils/ CD Blocks: Raigarh, Pusaur, Baramkela, Kharsiya, Gharghoda, Tamnar, Lallunga, Dharamjaigarh, Sa- rangarh. DEMOGRAPHY As per Census 2011, the total population of Raigarh is 14,93,984 which accounts for 5.85 percent of the total population of State. The percentage of urban population in Raigarh is 16.49 percent, which is lower than the state average of 23.24 percent. Out of the total population there are 750,278 males and 743,706 females in the district. This gives a sex ratio of 991.24 females per 1000 males. The decadal growth rate of population in Chhattisgarh is 22.59 percent, while Raigarh reports a 18.02 percent decadal increase in the population. The district population density is 211 in 2011. The Scheduled Caste population in the district is 15 percent while Scheduled Tribe comprises one third of the total population. LITERACY The overall literacy rate of Raigarh district is 73.26 percent while the male & female literacy rate is 83.49 and 63.02 percent respectively. At the block level, a considerable variation is noticeable in male-female literacy rate. Dharamjaigarh has the lowest literacy rate 62.43 percent, with 74.09 per- cent men and 50.90 percent women being literate. Raigarh block, subse- quently, has the highest literacy rates– among both males and females. -

Department Related Parliamentary Standing Committee (RS)
Department Related Parliamentary Standing Committee (RS) Committee on HUMAN RESOURCES DEVELOPMENT Rajya Sabha Member : 6 Vacant : 4 S.NO. Member Name State Party 1 Shri Vishambhar Prasad Nishad Uttar Pradesh Samajwadi Party 2 Shri Derek O Brien West Bengal ALL INDIA TRINAMOOL CONGRESS 3 Shri Sasmit Patra Odisha Biju Janata Dal 4 Dr. Vinay P. Sahasrabuddhe Maharashtra Bharatiya Janata Party 5 Shri Gopal Narayan Singh Bihar Bharatiya Janata Party 6 Shri Akhilesh Prasad Singh Bihar Indian National Congress Lok Sabha Member : 21 Vacant (LS) : 0 S.NO. Member Name State Constituency Party 1 Shri Rajendra Agrawal Uttar Pradesh Meerut BJP 2 Dr. Dhal Singh Bisen Madhya Pradesh Balaghat BJP 3 Shri Santokh Singh Chaudhary Punjab Jalandhar INC 4 Shri Lavu Sri Krishna Devarayalu Andhra Pradesh Narasaraopet YSR Cong.Party 5 Shri Sangamlal Kadedin Gupta Uttar Pradesh Pratapgarh BJP 6 Shri S. Jagathrakshakan Tamil Nadu Arakkonam DMK 7 Shri Sadashiv Kisan Lokhande Maharashtra Shirdi SS Dr. Jaisiddeshwar Shivacharya 8 Maharashtra Solapur BJP Mahaswamiji 9 Shri Asit Kumar Mal West Bengal Bolpur AITC 10 Ms. Chandrani Murmu Odisha Keonjhar BJD 11 Shri Balak Nath Rajasthan Alwar BJP 12 Dr. T. R. Paarivendhar Tamil Nadu Perambalur DMK 13 Shri Chandeshwar Prasad Bihar Jahanabad JD(U) 14 Shri T.N. Prathapan Kerala Thrissur INC 15 Shri Ratansinh Magansinh Rathod Gujarat Panchmahal BJP 16 Shri Jagannath Sarkar West Bengal Ranaghat BJP 17 Dr. Arvind Kumar Sharma Haryana Rohtak BJP 18 Shri Vishnu Dutt Sharma Madhya Pradesh Khajuraho BJP Bhiwani- 19 Shri Dharambir Singh Haryana BJP Mahendragarh 20 Shri S. Venkatesan Tamil Nadu Madurai CPI(M) 21 Shri Ashok Kumar Yadav Bihar Madhubani BJP Department Related Parliamentary Standing Committee (RS) Committee on INDUSTRY Rajya Sabha Member : 9 Vacant : 1 S.NO. -
Common Service Center List
CSC Profile Details Report as on 15-07-2015 SNo CSC ID District Name Block Name Village/CSC name Pincode Location VLE Name Address Line 1 Address Line 2 Address Line 3 E-mail Id Contact No 1 CG010100101 Durg Balod Karahibhadar 491227 Karahibhadar LALIT KUMAR SAHU vill post Karahibhadar block dist balod chhattisgarh [email protected] 8827309989 VILL & POST : NIPANI ,TAH : 2 CG010100102 Durg Balod Nipani 491227 Nipani MURLIDHAR C/O RAHUL COMUNICATION BALOD DISTRICT BALOD [email protected] 9424137413 3 CG010100103 Durg Balod Baghmara 491226 Baghmara KESHAL KUMAR SAHU Baghmara BLOCK-BALOD DURG C.G. [email protected] 9406116499 VILL & POST : JAGANNATHPUR ,TAH : 4 CG010100105 Durg Balod JAGANNATHPUR 491226 JAGANNATHPUR HEMANT KUMAR THAKUR JAGANNATHPUR C/O NIKHIL COMPUTER BALOD [email protected] 9479051538 5 CG010100106 Durg Balod Jhalmala 491226 Jhalmala SMT PRITI DESHMUKH VILL & POST : JHALMALA TAH : BALOD DIST:BALOD [email protected] 9406208255 6 CG010100107 Durg Balod LATABOD LATABOD DEKESHWAR PRASAD SAHU LATABOD [email protected] 9301172853 7 CG010100108 Durg Balod Piparchhedi 491226 PIPERCHEDI REKHA SAO Piparchhedi Block: Balod District:Balod [email protected] 9907125793 VILL & POST : JAGANNATHPUR JAGANNATHPUR.CSC@AISEC 8 CG010100109 Durg Balod SANKARAJ 491226 SANKARAJ HEMANT KUMAR THAKUR C/O NIKHIL COMPUTER ,TAH : BALOD DIST: BALOD TCSC.COM 9893483408 9 CG010100110 Durg Balod Bhediya Nawagaon 491226 Bhediya Nawagaon HULSI SAHU VILL & POST : BHEDIYA NAWAGAON BLOCK : BALOD DIST:BALOD [email protected] 9179037807 10 CG010100111 -

Dharamjaigarh Block, Raigarh DISTRICT, CHHATTISGARH
कᴂद्रीय भूमि जल बो셍ड जल संसाधन, नदी विकास और गंगा संरक्षण विभाग, जल शक्ति मंत्रालय भारत सरकार Central Ground Water Board Department of Water Resources, River Development and Ganga Rejuvenation, Ministry of Jal Shakti Government of India AQUIFER MAPPING AND MANAGEMENT OF GROUND WATER RESOURCES Dharamjaigarh block, Raigarh DISTRICT, CHHATTISGARH उत्तर मध्य छत्तीसग褼 क्षेत्र, रायपुर North Central Chhattisgarh Region, Raipur वछ जल - वछ भारत के ीय भूिम जल बोड mRrj e/; NRrhlx<+ {ks= f}rh; ry] ,y-ds- dkWaiksZjsV ,oa ykWftfLVd ikdZ] /kerjh jksM] MwejrjkÃZ] jk;iqj ¼NÙkhlx<+½&492015 Qksu&0771&2974405] QSDl&2974405 bZesy&[email protected] भारत सरकार Government of India जल शि मंालय Ministry of Jal Shakti जल संसाधन, नदी िवकास और गंगा संरण िवभाग Department of Water Resources, River Development & Ganga Rejuvenation के ीय भूिम जल बोड CENTRAL GROUND WATER BOARD Aquifer Mapping and Management Plan in Dharamjaigarh block, Raigarh District, Chhattisgarh By Sh. A K Biswal (Scientist-D) North Central Chhattisgarh Region Raipur 2020 Government of India Ministry of Jal Shakti Department of Water Resources, River Development & Ganga Rejuvenation CENTRAL GROUND WATER BOARD Aquifer Mapping and Management Plan in Dharamjaigarh block, Raigarh District, Chhattisgarh By Sh. A K Biswal (Scientist-D) Type of Study Officer engaged Data compilation, Data Gap Analysis & Sri S.Acharya, Scientist-D, (AAP-2015-16) Data Generation Data Interpretation, Integration, Aquifer Sri A. K. Biswal, Scientist-D Mapping, Management Plan & Report writing North Central Chhattisgarh Region Raipur 2020 BLOCK AT A GLANCE DHARAMJAIGARH BLOCK, RAIGARH DISTRICT, CHHATTISGARH 1. -

About Chhattisgarh
About Chhattisgarh Map Chhatisgarh state and districts (Stand 2007) At the time of separation from Madhya Pradesh, Chhattisgarh originally had 16 districts. Two new districts: Bijapur and Narayanpur were carved out on May 11, 2007[1] and nine new districts on Jan 1, 2012. The new districts have been created by carving out the existing districts to facilitate more targeted, focused and closer administration. These districts have been named Sukma, Kondagaon, Balod, Bemetara, Baloda Bazar, Gariaband, Mungeli, Surajpur and Balrampur[2] Contents [hide] 1 Background 2 Administrative history 3 Districts of Chhattisgarh 4 References 5 External links Background[edit] A district of an Indian state is an administrative geographical unit, headed by a district magistrate or a deputy commissioner, an officer belonging to the Indian Administrative Service. The district magistrate or the deputy commissioner is assisted by a number of officials belonging to different wings of the administrative services of the state. A superintendent of Police, an officer belonging to Indian Police Service is entrusted with the responsibility of maintaining law and order and related issues. Administrative history Before Indian independence, present-day Chhattisgarh state was divided between the Central Provinces and Berar, a province of British India, and a number of princely states in the north, south, and east, which were part of the Eastern States Agency. The British province encompassed the central portion of the state, and was made up of three districts, Raipur, Bilaspur, and Durg, which made up the Chhattisgarh Division of the Central Provinces. Durg District was created in 1906 out of the eastern portion of Raipur District. -

S.No Districts Covid Care Centre Hospital Category Total
S.No Districts Covid Care Centre Hospital Category Total Beds 1 Balod ITI Batera, Dondilohara Covid Care Center 100 2 Balod ITI Dhanora, Gurur Covid Care Center 100 3 Balod ITI Khallari, Gunderdehi Covid Care Center 60 4 Balod Sports Club Lal Maidan Dallirajhara Dondi Covid Care Center 100 5 Balod Livelyhood College Balod Covid Care Center 300 6 Balod PWD Colony Balod Covid Care Center 56 7 BALODA BAJAR DAV Khamhariya Baloda Bazar Covid Care Center 70 8 BALODA BAJAR ITI Simga Balodabazar Covid Care Center 112 9 BALODA BAJAR Livelyhood College Sankari Baloda Bazar Covid Care Center 161 10 BALODA BAJAR Pre Metric ST Hostal Kasdol Covid Care Center 50 11 Balrampur Polytecnic College Ramanunjganj Covid Care Center 250 12 Bastar Boys Hostal Bakawand Bastar Covid Care Center 200 13 Bastar Post Matric College Bastar Covid Care Center 250 14 Bemetara Lively hood college Bemetara Covid Care Center 130 15 Bemetara Agriculture College Covid Care Center 255 16 Bemetara Govt PG College Covid Care Center 100 17 Bemetara SRS Covid Care Center 25 18 Bijapur ITI Bairamgarh Bijapur Covid Care Center 100 19 Bijapur ITI rudraram Covid Care Center 100 20 Bilaspur Central Hospital railway Covid Care Center 75 21 Bilaspur Chitrakoot hostel bilaspur Covid Care Center 200 22 Bilaspur Community Hospital CH Bharni Covid Care Center 50 23 Bilaspur Mental Hospital Sendri Bilaspur Covid Care Center 10 24 Bilaspur NTPC seepat Covid Care Center 10 25 Bilaspur Prayas Hostel Bilaspur Covid Care Center 400 26 Dantewada Covid Care Center Eklavya Parisar Jawanga Covid Care -
Copy of CCC with Address and Phn No.Xlsx
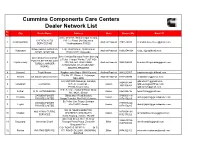
Cummins Components Care Centers Dealer Network List Sr. City Dealer Name Address State Contact No Email ID No. D.No. 27-2-9/1, Sitaramnagar Colony, CHENDU AUTO 100 feet Road, Old Gajuwaka, 1 Visakhapatnam Andhra Pradesh 7893576688 [email protected] SERVICES KB Visakhapatnam 530026 SREE VENKATESWARA 1-96, GUDAVALLI, GUDAVALLI 2 Vijaywada Andhra Pradesh 08662544124 [email protected] DIESEL SYSTEMS PANCHAITY,Vijaywada Sree Venkata Ramana Power Steering SRI VENKATA RAMANA & Turbo Charger Works; PLOT NO:- POWER STEERING AND 3 Rajahmundry 359, WATER TANK ROAD, Andhra Pradesh 9966366555 [email protected] TURBO CHARGER AUTONAGAR, RAJAHMUNDRY, WORKS ANDHRA PRADESH 4 Kurnool Trupti Motors Raghavendra Nager NH44 Kurnool Andhra Pradesh 9440232567 [email protected] Plot No.171, Phase II, Autonagar, 5 Nellore Sri Sarvani Diesel Service Andhra Pradesh 9849139999 [email protected] NELLORE G.D.MOTORS,Sarusojai, Garoliya, [email protected] 9864031944 6 Guwahati G.D Motors N.H.-37,,Guwahati - Assam [email protected]; 9435104854 781034,Assam,India, [email protected] N.S. Avenue, Haikandi Road, Shop 7 Silchar R. D. AUTOMOBILES Assam 9954099796 [email protected] No. 942/1, Silchar GARUDA POWER Gillapukhuri Road,Bordoloi 9706009311/ 8 Tinsukia Assam [email protected] PRIVATE LIMITED Nagar,Tinsukia, Pin-786125,Assam 9178456285 Ex.Police Line.Tezpur,Sonitpur GARUDA POWER 7399000242/ 9 Tejpur ,Pin-784001,Assam Assam [email protected] PRIVATE LIMITED 9178456285 NH 39, NEAR HOME PIPE, M/S ARNAV TURBO 8876054191/ 10 Khatkati KHATKHATI, KHATKAHTI, Assam [email protected] SERVICES 6002179202 Karbi Anglong, Assam, 782480 American Diesel, N.H. 31, Near 9934630786/ 11 Begusarai American Diesel Roongta Petrol Pump, Zero Mile Bihar [email protected] 8507500000 Begusarai Pin;- C/O- ROHTAS DIESELS OLD 12 Rohtas ROHTAS SERVICE G.T. -
Click Here to See List of Proposed Study Center
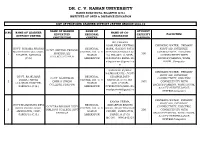
DR. C. V. RAMAN UNIVERSITY KARGI ROAD KOTA, BILASPUR (C.G.) INSTITUTE OF OPEN & DISTANCE EDUCATION LIST OF PROPOSED LEARNER SUPPORT CENTRE SESSION 2018-19 NAME OF HIGHER NAME OF STUDENT S.NO NAME OF LEARNER NAME OF CO- EDUCATUIN REGIONAL CAPECITY FACILITIES . SUPPORT CENTRE ORDINATOR INSTITUTION CENTRE (APPROX) MD.PARWEZ ALAM,NEAR CENTRAL DRINKING WATER, PRIMARY GOVT. SHYAMA PRASAD REGIONAL BANK, GAURAV PATH FIRST AID, INTERNET, GOVT. SHYAMA PRASAD MUKHARJEE COLLEGE, CENTRE, DR. C. V. SITAPUR,SARGUJA,(C. CONNECTIVITY, ELECTRIC 1 MUKHARJEE 300 SITAPUR, SARGUJA RAMAN G.) PIN-497111,MOB- CONNECTIVITY WITH COLLEGE,SITAPUR (C.G.) AMBIKAPUR 9424261584 EMAIL ID- BACKUP,PARKING, WASH [email protected] ROOM.,Computer m SANDEEP KUMAR DRINKING WATER, PRIMARY RAJWADE,VILL-,POST- FIRST AID, INTERNET, GOVT. RAJKUMAR REGIONAL UDAIPUR,DIST- GOVT. RAJKUMAR CONNECTIVITY, ELECTRIC DHIRAJ SINGH CENTRE, DR. C. V. SARGUJA,(C.G.),PIN- 2 DHIRAJ SINGH 1000 CONNECTIVITY WITH COLLEGE,UDAIPUR, RAMAN 497117,MOB- COLLEGE,UDAIPUR BACKUP,PARKING, WASH ROOM, SARGUJA (C.G.) AMBIKAPUR 07909870934,MAIL ID- & CCTV SURVEILLANCE [email protected] SYSTEM,Computer m DRINKING WATER, PRIMARY KAMNA VERMA, FIRST AID, INTERNET, GOVT.RAJMOHANI DEVI REGIONAL KEDARPUR BHATHI GOVT.RAJMOHANI DEVI CONNECTIVITY, ELECTRIC GIRLS PG COLLEGE, CENTRE, DR. C. V. ROAD, NEAR TRICHON 3 GIRLS PG COLLEGE DIST- 200 CONNECTIVITY WITH AMBIKAPUR, DIST- RAMAN CHOWK, AMBIKAPUR, SARGUJA BACKUP,PARKING, WASH ROOM, SARGUJA (C.G.) AMBIKAPUR SARGUJA (C.G.) & CCTV SURVEILLANCE MO.NO. - 9981642327 SYSTEM,Computer VARSHA DRINKING WATER, PRIMARY KASHYAP,Takiya road, FIRST AID, INTERNET, REGIONAL kenabandh ambikapur, RAJEEV GANDHI GOVT. CONNECTIVITY, ELECTRIC RAJEEV GANDHI GOVT. CENTRE, DR. C. V. Distt. Surguja 4 COLLEGE AMBIKAPUR 600 CONNECTIVITY WITH COLLEGE,AMBIKAPUR RAMAN (C.G.),Cell: +91 (C.G.) BACKUP,PARKING, WASH ROOM, AMBIKAPUR 9424255074 & CCTV SURVEILLANCE Email : SYSTEM,Computer [email protected] Rinu Jain Manjusha Academy Namna Kala , Ring DRINKING WATER, PRIMARY Road Ambikapur , FIRST AID, INTERNET, REGIONAL K.R. -

Brief Industrial Profile of Raigarh District
lR;eso t;rs Government of India Ministry of MSME Brief Industrial Profile of Raigarh District Carried out by MSME -Development Institute, Raipur (Ministry of MSME, Govt. of India,) Phone :- 0771- 2427719 /2422312 Fax: 0771 - 2422312 e-mail: [email protected] Web- www.msmediraipur.gov.in Contents S. No. Topic 1. General Characteristics of the District 1.1 Location & Geographical Area 1.2 Topography 1.3 Availability of Minerals. 1.4 Forest 1.5 Administrative set up 2. District at a glance 2.1 Existing Status of Industrial Area in the District Durg 3. Industrial Scenario Of Durg 3.1 Industry at a Glance 3.2 Year Wise Trend Of Units Registered 3.3 Details Of Existing Micro & Small Enterprises & Artisan Units In The District 3.4 Large Scale Industries / Public Sector undertakings 3.5 Major Exportable Item 3.6 Growth Trend 3.7 Vendorisation / Ancillarisation of the Industry 3.8 Medium Scale Enterprises 3.8.1 List of the units in Durg & near by Area 3.8.2 Major Exportable Item 3.9 Service Enterprises 3.9.1 Potentials areas for service industry 3.10 Potential for new MSMEs 4. Existing Clusters of Micro & Small Enterprise 4.1 Detail of Major Clusters 4.1.1 Manufacturing Sector 4.1.2 Service Sector 4.2 Details of Identified Cluster 5. General issues raised by industry association during the course of meeting 6. Steps to set up MSMEs Brief Industrial Profile of Raigarh District 1. General Characteristics of the District Raigarh district is one of the oldest and important districts of Chhattisgarh State. -

Chhattisgarh 24X7 Connected Chhattisgarh
CHHATTISGARH 24X7 CONNECTED CHHATTISGARH Uttar Pradesh Bihar Jharkhand Madhya Pradesh CHHATTISGARH Maharashtra Odisha Telangana Andhra Pradesh The State of Chhattisgarh has seen rapid progress in road infrastructure development since 2014. A total of Rs. 9,070.02 Cr has been awarded for road works spanning 1,690.92 km in the State in the past four years. The length of National Highways in Chhattisgarh has reached 3,508.4 km in 2018. Construction and upgrading of National Highways and bridges is paving the way for socio-economic progress at a new pace, that is reaching each and every corner of the State, connecting backward areas and creating new opportunities for the people. “When a network of good roads is created, the economy of the country also picks up pace. Roads are veins and arteries of the nation, which help to transform the pace of development and ensure that prosperity reaches the farthest corners of our nation.” NARENDRA MODI Prime Minister “In the past four years, we have expanded the length of Indian National Highways network to 1,26,350 km. The highway sector in the country has seen a 20% growth between 2014 and 2018. Tourist destinations have come closer. Border, tribal and backward areas are being connected seamlessly. Multimodal integration through road, rail and port connectivity is creating socio economic growth and new opportunities for the people. In the coming years, we have planned projects with investments worth over Rs 6 lakh crore, to further expand the world’s second largest road network.” NITIN GADKARI Union