Rural Continuum in the Michigan National Guard
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Defense & Homeland Security Industry Profile
Defense & Homeland Security Industry Profile Macomb County, Michigan www.MacombBusiness.com | Macomb County Michigan | 1 600 500 400 300 200 Macomb County Toronto 100 Detroit New York Chicago Cleveland Distance is in miles Macomb County – A World Leader The Macomb Strategic Advantage in Defense and Homeland Security w Nearly 600 companies performing defense contract business Defense and Homeland Security companies find a strategic w Macomb County companies transacted over $26 billion in advantage in Macomb County, Michigan that exists nowhere defense business between 2000 and 2010 else in North America - our exceptional engineering, R&D and w Represents 63 percent of the defense business in Michigan advanced manufacturing capabilities. w Over 10,000 defense contracts awarded to Macomb County companies between 2000-2010 This strategic advantage is a direct result of over 100 years of meeting the exacting standards of the automotive, aerospace w Home to a full quarter of the world’s advanced manufacturing and defense industries. Over the decades, literally thousands work force of manufacturers have established this infrastructure while w More than 30,000 workers engaged in engineering, research perfecting their advanced manufacturing methods and processes. and development w Our region is ranked first in the nation for industrial R&D Today, defense and homeland security companies located in spending Macomb County are capitalizing on the highly skilled workforce, infrastructure and vast supplier network that only exist here, w Over 350 labs and research facilities in the state are devoted allowing them to operate more efficiently and provide quality to industrial and manufacturing products and services. technologies As a result, Macomb County companies are better able to w Nearly 400,000 diversify and gain access to new markets. -

Michigan Air Guard Historical Association April 2019
Michigan Air Guard Historical Association Website: www.selfridgeairmuseum.org Email: [email protected] April 2019 Table of Contents Page Taps, Honor Roll, Lost & Found 2 Letters Home 3 127th Wing Happenings 4-7 110th Attack Wing Happenings 8-10 Col. Donald G. Miller, CCMSgt William Cieciek, BG Leon D. Worden, SMSgt Macon Davis, & MSgt Cyrus Napper – In Memoriam 11-12 VA Assists with Burial of Unclaimed Veterans 13 This Day in History: Michigan Air National Guard 14-15 First Female Brigadier General in MI ANG 16-17 Museum Happenings 18-25 Reader Information Survey 26 Kroger Community Rewards Program 27 Amazon Smile 28 MAGHA Membership Application 29 Memorial Wall Brick Program 30 Michigan Air National Guard History Books 31 1 TAPS NAME MI ANG SERVICE DATE OF DEATH CMSgt William A. Cieciek 1953-1985 3 Feb 19 SMSgt Macon “Mickey” Davis ????-???? 28 Dec 18 Col Donald G. Miller 1968-1988 18 Jan 19 MSgt Cyrus “Cy” Napper ????-1994 23 Jan 19 Col Leon D. Worden 1953-1975 20 Feb 19 HONOR ROLL Due to the large number of Honor Roll members, only those who have either become Life Members or who have achieved a higher membership status since the last issue are listed below. A complete Honor Roll membership roster is published annually in the July issue. LIFE MEMBER Mr. & Mrs. Robert D. Drinkall (TACOM) Maj Chris Salaniuk (MI ANG) LOST & FOUND Our database of former members of the Michigan ANG continues to grow. Regrettably many of our alumni are deceased and many are without addresses. So when we find out where our former members are, we’ll try to put some information in the MANGBANG about them. -

Michigan Law Protecting the Civilian Jobs of Michigan National Guard Members on State Active Duty
MI-2015-NG Michigan Law Protecting The Civilian Jobs Of Michigan National Guard Members On State Active Duty By Captain Samuel F. Wright, JAGC, USN (Ret).1 And Kyle E. HelmiCk2 Today’s National Guard traces its origins to 1636, when the Massachusetts Bay Colony established the Massachusetts militia to defend the Colony against attacks by the PeQuot Indians. Other Colonies and states established similar state militias, and those state militias were Called to federal duty for the Revolutionary War, the War of 1812, the MexiCan-AmeriCan War, the Civil War, and the Spanish-AmeriCan War. Under federal legislation enacted very early in the 20th Century, state militia forCes have been given major federal assistanCe in pay, training, and eQuipment and have been given federal status as part of the Army National Guard of the United States, one of the seven Reserve Components of the United States Armed ForCes.3 After World War II, when the Air Force beCame a separate serviCe rather than part of the Army, Congress Created the Air National Guard of the United States as a similar hybrid state-federal military serviCe. Anthony Wayne V is a Staff Sergeant (SSG) in the MiChigan Army National Guard. When he enlisted, he took two enlistment oaths, one to the State of MiChigan and one to the United States of AmeriCa. He joined two overlapping but legally distinCt organizations. The Michigan Army National Guard is the present-day eQuivalent of the MiChigan State Militia. The Army National Guard of the United States is one of the seven Reserve Components of the United States armed forCes. -
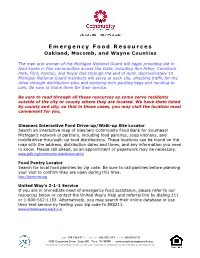
Emergency Food Resources Oakland, Macomb, and Wayne Counties
E m e r g e n c y F o o d R e s o u r c e s Oakland, Macomb, and Wayne Counties The men and women of the Michigan National Guard will begin providing aid to food banks in five communities across the state, including Ann Arbor, Comstock Park, Flint, Pontiac, and Royal Oak through the end of April. Approximately 10 Michigan National Guard members will serve at each site, directing traffic for the drive-through distribution sites and assisting with packing bags and handing to cars. Be sure to thank them for their service. Be sure to read through all these resources as some serve residents outside of the city or county where they are located. We have them listed by county and city, so that in those cases, you may visit the location most convenient for you. Gleaners Interactive Food Drive-up/Walk-up Site Locator Search an interactive map of Gleaners Community Food Bank for Southeast Michigan’s network of partners, including food pantries, soup kitchens, and mobile drive-thru/walk-up food distributions. These locations can be found on the map with the address, distribution dates and times, and any information you need to know. Please call ahead, as an appointment or paperwork may be necessary. www.gcfb.org/community-distribution-sites/ Food Pantry Locator Search for local food pantries by zip code. Be sure to call pantries before planning your visit to confirm they are open during this time. http://pantrynet.org United Way’s 2-1-1 Service If you are in immediate need of emergency food assistance, please refer to our resources below or contact the United Way’s Help and referral line by dialing 211 or 1-800-552-1183. -

Central Michigan University ROTC Chippewa Battalion 2011-2012
DEPARTMENT OF MILITARY SCIENCE / VOLUME 12 / FALL 2012 ALUMNI NEWSLETTER Central Michigan University ROTC Chippewa Battalion 2011-2012 2012 ROTC Hall of Fame Inductees COL (R) Gene D. Bruce MAJ (R) Thomas J. Jenks LTC (R) Lawrence E. Warner Cadre 1972-1977 Class of 1973 Class of 1962 2012 Football Schedule: Seven home games!!!!! INSIDE THIS ISSUE: Thur. Aug 30 Southeast Missouri State • Commissioning Ceremonies Sat. Sep 8 Michigan State • ROTC Alumni President’s address • State of the Battalion Sat. Sep 22 @ Iowa City • Field Leadership Reaction Course Sat. Sep 29 @ Northern Illinois • Cadet Summer Experiences Sat. Oct 6 @ Toledo • Hall of Fame/Military Ball • News from Alumni Fri. Oct 12 Navy (Military Day) Sat. Oct. 20 Ball State (Homecoming) Sat. Oct. 27 Akron Sat. Nov. 3 Western Michigan Sat. Nov. 10 @ Eastern Michigan Sat. Nov. 17 Miami Fri. Nov. 23 @ Massachusetts Fri. Nov. 30 MAC Championship @ Detroit 1 DEPARTMENT OF MILITARY SCIENCE / VOLUME 12 / FALL 2012 2011-2012 ROTC Commissioned Second Lieutenants Ferris State University and Central Michigan University Congratulations to the new alumni! CMU AUGUST 2011 FSU MAY 2012 MICHAEL C. ANDERSON CORY J. BUTER BRANCHED: Transportation (Army Reserve) BRANCHED: Adjutant General (National Guard) HOMETOWN: Pentwater, MI HOMETOWN: Grand Haven, MI STEVE FEDEWA DAKODA S. DONNELLY BRANCHED: Quartermaster (Active Duty) BRANCHED: Field Artillery (Active Duty) HOMETOWN: Ovid-Elsie, MI HOMETOWN: Greenville, MI THOMAS J. GORECKI JR ROBERT J. SALESKI BRANCHED: Adjutant General (Army Reserve) BRANCHED: Ordnance (National Guard) HOMETOWN: Ferndale, MI HOMETOWN: Detroit, MI HARMONY M. MCCOY DARREK R. LADERMANN BRANCHED: Engineer (Active Duty) BRANCHED: Aviation (National Guard) HOMETOWN: Midland, MI HOMETOWN: Greenville, MI DAVID S. -

FY22 TAILS 1,465,000 1,465,000 FY23 Totals 18,905,000 18,905,000
DEPARTMENT OF MILITARY & VETERANS AFFAIRS 5-Year Capital Outlay Budget Plan FY 2022-2026 October 31, 2020 I. MIARNG The Michigan National Guard strives to be fully manned, trained, and equipped to accomplish multi domain operations during any assigned State or Federal mission. Critical to our overall readiness remains the dignified and respectful treatment of all our members and a culture that accepts diversity. Securing consistent funding for maintenance and modernization and establishing facilities in locations that enable strategic objectives greatly affects our ability to gain and retain a quality and diverse workforce. Our ability to improve Readiness Centers (RC) by means of Sustainment, Restoration & Modernization and our ability to improve and construct Readiness Centers by military construction (MILCON) are integral to mission accomplishment, our ability to defend the nation, and protecting the lives and property of the State of Michigan’s citizens. Programmatic Changes: Because of anticipated competition for federal and state funds, the Construction and Facilities Management Office (CFMO) has been proactive in contracting master plans for our two training sites, our airfield, our readiness centers and our facility maintenance shops. With these initiatives, CFMO is developing short, mid and long-term goals that are aligned with the DMVA Strategic Plan. This will include upgrading and right-sizing readiness centers and facility maintenance shops statewide, and where practical, purchasing of buildings that meet our requirements and location needs. At Camp Grayling, we will be focusing on achieving the classification of an ARNG “Director’s Pick” training location. This title recognizes the installation as a key ARNG readiness building location, increasing the potential for MILCON projects needed to achieve key outcomes within the DMVA Strategic Plan. -

Michigan Army National Guard Soldiers Continue Operations in Houghton County
FOR IMMEDIATE RELEASE News Release No. 16 – June 27, 2018 Michigan Army National Guard Soldiers Continue Operations in Houghton County LANSING, MICH. The Michigan National Guard remains in Michigan’s Upper Peninsula assisting with repair operations following severe rain that caused extensive washouts. The deployment has been extended to Tuesday, July 3, to help with projects to make the roads passable. Approximately 70 Soldiers from armories in Kingsford, Iron River, Calumet, Sault Ste. Marie and Montague were activated in response to the emergency declaration issued by Governor Snyder June 18. The Soldiers are members of 107th Engineer Battalion headquartered in Ishpeming and the 507th Engineer Battalion headquartered in Kalamazoo. The Soldiers have been moving gravel to repair affected areas. The temporary repairs allow stranded residents avenues of entry and exit that have been destroyed by the floodwaters; also improving the public health capabilities allowing for passage by emergency medical services. “Our Soldiers have made progress, but more work needs to be done. They stand ready to help and remain committed to completing their mission,” said Maj. Gen. Greg Vadnais, adjutant general of the Michigan National Guard and director of the Michigan Department of Military and Veterans Affairs. “The men and women I work with never fail to impress me. I hope we have been able to provide comfort to our Michigan residents who will be dealing with the aftermath of this destructive flooding for quite some time.” About the Michigan National Guard The Michigan National Guard’s 10,000 Soldiers and Airmen stand ready to serve both state and nation. -
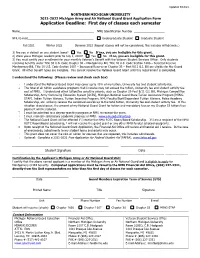
Michigan Army and Air National Guard Grant Application Form Application Deadline: First Day of Classes Each Semester
Updated 7/16/21 NORTHERN MICHIGAN UNIVERSITY 2021-2022 Michigan Army and Air National Guard Grant Application Form Application Deadline: First day of classes each semester Name______________________________________________ NMU Identification Number ___________________ NMU E-mail_________________________________________ Undergraduate Student Graduate Student ______ Fall 2021 _____Winter 2022 _____ Summer 2022 (Repeat classes will not be considered, this includes withdrawals.) 1) Are you in default on any student loans? Yes No If yes, you are ineligible for this grant. 2) Were you a Michigan resident prior to July 1, 2020? Yes No If no, you are ineligible for this grant. 3) You must certify your enrollment for your monthly Veteran’s Benefit with the Veteran Student Services Office. Only students receiving benefits under Title 38 U.S. Code Chapter 30 – Montgomery Bill, Title 10 U.S. Code Section 1606 – Selected Reserve Montgomery Bill, Title 10 U.S. Code Section 1607 – Increased Reserve or Chapter 33 – Post 9/11 G.I. Bill are eligible for the Guard Grant. All other benefit types are ineligible. You cannot receive the National Guard Grant until this requirement is completed. I understand the following: (Please review and check each box) I understand the National Guard Grant may cover up to 45% of my tuition, University fee and student activity fee. The total of all tuition assistance programs that I receive may not exceed the tuition, University fee and student activity fee cost of NMU. I understand other tuition/fee sensitive awards, such as Chapter 33-Post 9/11 G.I. Bill, Michigan Competitive Scholarship, Army Continuing Education System [ACES], Michigan National Guard State Tuition Assistance Program [MING- STAP], Indian Tuition Waivers, Tuition Incentive Program, NMU Faculty/Staff/Dependent Tuition Waivers, Police Academy Scholarship, etc. -

Veterans Benefits
VETERANS Benefits & Services For Michigan Military Veterans To better assist you, the veterans information listed in this booklet has been organized into 3 levels of available Veterans programs – FEDERAL, STATE, and LOCAL. Much of the information contained in this booklet comes from the U.S. Department of Veterans Affairs web site at www.va.gov. For more state and local information, visit www.michigan.gov and www.michiganveterans.com. This booklet also provides valuable federal, state and local veteran contact information. Prepared by the Michigan Legislature This information is provided free to Michigan citizens and is not for reproduction for resale or profit. This information was accurate at the time of printing. teran Ve s Benefits & Services Table of Contents Dear Veteran Thank You for Your Service . 3 Education and Training Education and Training – Federal Programs . 4 Education and Training – State of Michigan Programs . 7 Educational Benefits for Children of Disabled or Deceased Veterans . 8 Employment Employment – Federal Programs . 9 Employment – State of Michigan Programs . 11 Apprenticeship Programs for Discharged Veterans . 13 Health Care Health Care and Hospital Benefits – Federal Programs . 15 Military Exposures . 22 Health Care and Hospital Benefits – State of Michigan . 23 Veterans’ Facility Ombudsman . 24 Homeless Veterans . 24 Women Veterans Health Care . 26 Michigan VA Medical Facilities and Outpatient Clinics . 27 Monetary Benefits . 28 Home Loans and Tax Credits Home Loan Guaranties – Federal Programs . 31 State of Michigan Benefits . 33 Life Insurance . 34 Dependent and Survivor Benefits Burial Benefits . 36 Survivor Benefits for Spouse and Children – Federal Benefits . 38 Financial Emergencies and Veterans Resources Programs – State of Michigan . -

VSO by County.Xlsx
VETERANS AFFAIRS AND REHABILITATION RESOURCES As a district commander, you may encounter situations during your commandership where a veteran will approach you in reference to financial assistance. You should always refer them to the appropriate agencies within the veteran's community such as Red Cross, Veterans Trust Fund, Soldier/Sailor Relief Commission, etc. If, however, these options have been exhausted, department headquarters provides the following options based on eligibility and available resources. The American Legion Department of Michigan Veteran Services Regional Office Our staff is dedicated to providing the very best veterans’ advocacy to Michigan Veterans and their families. They can assist with Claims Preparation, Presentation and appeal counsel in Veterans’ benefits services. Assist you and your Dependents in getting the Benefits that you have earned by your service to your country. American Legion Veterans Affairs and Rehabilitation Mr. Gary Easterling, Director Patrick V. McNamara Federal Building Room 1210 477 Michigan Avenue Detroit, MI 48226 Office Phone (313) 964-6640 Fax (313) 964-5697 e-mail - [email protected] Monday thru Friday 8:00 am to 4:00 pm ------------------------------------- Call the Detroit office for Field Service Officer Schedule -------------------------------------- Find a County Veteran Service Office for Michigan veteran trust fund questions at http://www.michiganveterans.com/Home/Benefit-Counselors American Legion National "Temporary Financial Assistance" Program: Application must be for wartime veterans who have minor children in the home. Application can be obtained from department headquarters by contacting Kim Siedelberg at 517.371.4720, ext. 13 or Department VAR Director Gary Easterling 313.964.6640. Department Welfare Fund: To assist with emergency needs such as food, rent, or utilities. -
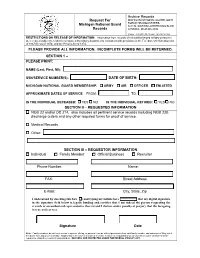
Request for Michigan National Guard Records Archive Records PLEASE
Archive Records Request For MICHIGAN NATIONAL GUARD JOINT FORCE HEADQUARTERS Michigan National Guard 3411 N. MARTIN LUTHER KING BLVD Records LANSING, MI 48906-2934 Phone: (517)481-8331 Fax: (517)481-8363 RESTRICTIONS ON RELEASE OF INFORMATION: Information from records of retired/discharged military personnel are released subject to restrictions imposed by military departments consistent with provisions in the Freedom of Information Act of 1967 (Revised 1974) and the Privacy Act of 1974. PLEASE PROVIDE ALL INFORMATION. INCOMPLETE FORMS WILL BE RETURNED. SECTION 1 – INFORMATION REQUIRED TO LOCATE RECORDS PLEASE PRINT: NAME (Last, First, MI): _______________________________________________________ SSN/SERVICE NUMBER(S): __________________ DATE OF BIRTH: _________________ MICHIGAN NATIONAL GUARD MEMBERSHIP: ARMY AIR OFFICER ENLISTED APPROXIMATE DATES OF SERVICE FROM: _________________ TO: ___________________ IS THE INDIVIDUAL DECEASED: YES NO IS THE INDIVIDUAL RETIRED: YES NO SECTION II – REQUESTED INFORMATION NGB 22 and/or DD 214, also includes all pertinent service records including NGB 23B discharge orders and any other required forms for proof of service. Medical Records Other: ________________________________________________________________ __________________________________________________________________________ SECTION III – REQUESTOR INFORMATION Individual Family Member Official Business Recruiter __________________________ _________________________________________ Phone Number: Name: __________________________ _________________________________________ -

Michigan Air Guard Historical Association July
Michigan Air Guard Historical Association Website: www.selfridgeairmuseum.org Email: [email protected] July - September 2020 TABLE OF CONTENTS PAGE Taps 2 - 3 127th Wing Happenings 3-4 110th Attack Wing Happenings 5-6 This Day in History 7-10 Museum Happenings 11-28 RV Storage Area 28 Memorial Wall Brick Program 29 Michigan Activity Pass 30 Macomb County Heritage Alliance’s ‘Passport Program’ 39 MAGHA Membership Application 31 1 MANGBANG July-September 2020 TAPS NAME MI ANG SERVICE DATE OF DEATH Tracy McQueen 31 August 2020 Tracy Wallace McQueen, Sr., 1939-1920: age 81, of Jodi Lane in Irvine, passed away Monday, August 31, 2020, at the University of Kentucky Medical Center following a long illness. He was born July 25, 1939 in Estill County and was the son of the late Clay and Ethel Wells McQueen. He was a retired United States Army veteran of 34 years and 6 months who served during the Korean Conflict and the Vietnam War. He was a Kentucky Colonel and a member of the American Legion. He was also a member of the Pine Hill Baptist Church and had lived in Estill County most of his life. He is survived by: His wife: Melba A. Wade McQueen,3 daughters: Dawn (Simon) Mortimer of London, Kelley Harlow of Estill Co., Susan McQueen of Estill Co., 2 sons: Tracy McQueen, Jr. of North Carolina, Patrick McQueen of Perryville, 2 half-brothers: Bobby McQueen and Michael McQueen, 8 grandchildren: William D. Harlow, Benjamin J. McQueen, Shelby D. (Derrick) Neal, Jonathan L. McQueen, Connor D. Harlow, Stephen D.