Liquid Chromatography Tandem Mass Spectrometry Determination Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Extracts from PRAC Recommendations on Signals Adopted at the 9-12 March 2020 PRAC
6 April 20201 EMA/PRAC/111218/2020 Corr2,3 Pharmacovigilance Risk Assessment Committee (PRAC) New product information wording – Extracts from PRAC recommendations on signals Adopted at the 9-12 March 2020 PRAC The product information wording in this document is extracted from the document entitled ‘PRAC recommendations on signals’ which contains the whole text of the PRAC recommendations for product information update, as well as some general guidance on the handling of signals. It can be found here (in English only). New text to be added to the product information is underlined. Current text to be deleted is struck through. 1. Immune check point inhibitors: atezolizumab; cemiplimab; durvalumab – Tuberculosis (EPITT no 19464) IMFINZI (durvalumab) Summary of product characteristics 4.4. Special warnings and precautions for use Immune-mediated pneumonitis [..] Patients with sSuspected pneumonitis should be evaluated confirmed with radiographic imaging and other infectious and disease-related aetiologies excluded, and managed as recommended in section 4.2. LIBTAYO (cemiplimab) Summary of product characteristics 1 Expected publication date. The actual publication date can be checked on the webpage dedicated to PRAC recommendations on safety signals. 2 A footnote was deleted on 8 April 2020 for the signal on thiazide and thiazide-like diuretics (see page 3). 3 A minor edit was implemented in the product information of the signal on thiazide and thiazide-like diuretics on 5 June 2020 (see page 4). Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us Send us a question Go to www.ema.europa.eu/contact Telephone +31 (0)88 781 6000 An agency of the European Union © European Medicines Agency, 2020. -

Isocratic HPLC Method for Simultaneous Determination of Amlodipine and Xipamide in Human Plasma
vv ISSN: 2689-7628 DOI: https://dx.doi.org/10.17352/ojabc CHEMISTRY GROUP Received: 06 April, 2020 Research Article Accepted: 05 May, 2020 Published: 06 May, 2020 *Corresponding author: Mahmoud M Sebaiy, Isocratic HPLC Method for Department of Medicinal Chemistry, Faculty of Pharmacy, Zagazig University, Zagazig, Egypt, Tel: 01062780060; Fаx: 0552303266; Simultaneous Determination E-mail: Keywords: HPLC; Amlodipine; Xipamide; Human of Amlodipine and Xipamide in plasma; Pharmacokinetic https://www.peertechz.com Human Plasma Mahmoud M Sebaiy1*, Hisham E Abdellatef2, Mohamed A Elmosallamy3 and Mustafa Kh Alshuwaili3,4 1Department of Medicinal Chemistry, Faculty of Pharmacy, Zagazig University, Zagazig, Egypt 2Department of Analytical Chemistry, Faculty of Pharmacy, Zagazig University, Zagazig, Egypt 3Department of Chemistry, Faculty of Science, Zagazig University, Zagazig, Egypt 4Ministry of Education, Iraq Abstract An HPLC method had been developed and validated for rapid simultaneous separation and determination of the two antihypertensive drugs, amlodipine and xipamide in human plasma within 5 minutes. Drugs are extracted from plasma using methanol, the environmentally benign solvent, for protein precipitation technique. Separation ® was carried out on a Thermo Scientifi c BDS Hypersil C8 column (5μm, 2.50x4.60 mm) using a mobile phase of methanol: 0.025M KH2PO4 (70: 30, v/v) adjusted to pH 3.49 with ortho - phosphoric acid at ambient temperature. The fl ow rate was 1 ml/min and maximum absorption was measured using DAD detector at 235nm. The retention times of amlodipine and xipamide were recorded to be 4.51 and 3.38 minutes, respectively, indicating a shorter analysis time. Limits of detection were reported to be 0.17 and 0.25 μg/ml for amlodipine and xipamide, respectively, showing a high degree of the method sensitivity. -

Azosemide Is More Potent Than Bumetanide and Various Other Loop
www.nature.com/scientificreports OPEN Azosemide is more potent than bumetanide and various other loop diuretics to inhibit the sodium- Received: 21 November 2017 Accepted: 14 June 2018 potassium-chloride-cotransporter Published: xx xx xxxx human variants hNKCC1A and hNKCC1B Philip Hampel 1,2, Kerstin Römermann1, Nanna MacAulay 3 & Wolfgang Löscher1,2 The Na+–K+–2Cl− cotransporter NKCC1 plays a role in neuronal Cl− homeostasis secretion and represents a target for brain pathologies with altered NKCC1 function. Two main variants of NKCC1 have been identifed: a full-length NKCC1 transcript (NKCC1A) and a shorter splice variant (NKCC1B) that is particularly enriched in the brain. The loop diuretic bumetanide is often used to inhibit NKCC1 in brain disorders, but only poorly crosses the blood-brain barrier. We determined the sensitivity of the two human NKCC1 splice variants to bumetanide and various other chemically diverse loop diuretics, using the Xenopus oocyte heterologous expression system. Azosemide was the most potent NKCC1 inhibitor (IC50s 0.246 µM for hNKCC1A and 0.197 µM for NKCC1B), being about 4-times more potent than bumetanide. Structurally, a carboxylic group as in bumetanide was not a prerequisite for potent NKCC1 inhibition, whereas loop diuretics without a sulfonamide group were less potent. None of the drugs tested were selective for hNKCC1B vs. hNKCC1A, indicating that loop diuretics are not a useful starting point to design NKCC1B-specifc compounds. Azosemide was found to exert an unexpectedly potent inhibitory efect and as a non-acidic compound, it is more likely to cross the blood-brain barrier than bumetanide. Te Na+–K+–2Cl− cotransporter NKCC1 (encoded by SLC12A2) plays an important role in Cl- uptake in neu- rons both in developing brain and in adult sensory neurons1,2. -

Presented By: Dr. Joohee Pradhan Assistant Professor Department of Pharmaceutical Sciences, MLSU, Udaipur
Presented By: Dr. Joohee Pradhan Assistant Professor Department of Pharmaceutical Sciences, MLSU, Udaipur OUTLINE • Introduction and Definition • Relevant Physiology of Urine Formation • Classification: different ways • Carbonic anhydrase inhibitors: Acetazolamide*, Methazolamide, Dichlorphenamide. • Thiazides: Chlorthiazide*, Hydrochlorothiazide, Hydroflumethiazide, Cyclothiazide, • Loop diuretics: Furosemide*, Bumetanide, Ethacrynic acid. • Potassium sparing Diuretics: Spironolactone, Triamterene, Amiloride. • Osmotic Diuretics: Mannitol 2 Introduction and Definition • Diuretics (natriuretics) are drugs which cause a net loss of Na+ and water in urine and hence increase the urine output (or) urine volume. • The primary action of most diuretics is the direct inhibition of Na+ reabsorption (increased excretion) at one or more of the four major sites along the nephron. • An increased Na+ excretion is accompanied by anion like Cl- Since NaCl is the major determinant of extracellular fluid volume; Diuretics reduce extracellular fluid volume (decrease in oedema) by decreasing total body NaCl content. 3 Introduction and Definition • Diuretics are very effective in the treatment of conditions like: o chronic heart failure o nephrotic syndrome o chronic hepatic diseases o hypertension o Pregnancy associated oedema o Cirrhosis of the liver. 4 Relevant Physiology of Urine Formation • Kidneys are the organs responsible for urine formation. Two important functions of the kidney are: o To maintain a homeostatis balance of electrolytes and water. o To excrete water soluble end products of metabolites. • Each kidney contains approximately one million nephrons and is capable of forming urine independently. • Urine formation starts from glomerular filtration (g.f.) in a prodigal way. • Normally, about 180 L of fluid is filtered everyday: all soluble constituents of blood minus the plasma proteins (along with substances bound to them) and lipids, are filtered at the glomerulus. -

Evidence Review G: Step 4 Treatment
National Institute for Health and Care Excellence Final Hypertension in adults: diagnosis and management [G] Evidence review for step 4 treatment NICE guideline NG136 Intervention evidence review underpinning recommendations 1.4.44 to 1.4.50 in the guideline August 2019 Final This evidence review was developed by the National Guideline Centre Hypertension in adults: Final Contents Disclaimer The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, professionals are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or service users. The recommendations in this guideline are not mandatory and the guideline does not override the responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and, where appropriate, their carer or guardian. Local commissioners and providers have a responsibility to enable the guideline to be applied when individual health professionals and their patients or service users wish to use it. They should do so in the context of local and national priorities for funding and developing services, and in light of their duties to have due regard to the need to eliminate unlawful discrimination, to advance equality of opportunity and to reduce health inequalities. Nothing in this guideline should be interpreted in a way that would be inconsistent with compliance with those duties. NICE guidelines cover health and care in England. Decisions on how they apply in other UK countries are made by ministers in the Welsh Government, Scottish Government, and Northern Ireland Executive. -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -
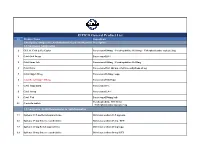
EIPICO General Product List
EIPICO General Product List S.N Product Name Inqredients 1.Analgesics, Antipyretics ,Antiinflammatories & AntirheumaticsDescription 1.1.Analgesics Antipyretics 1 CETAL Cold & Flu Caplet Paracetamol 500mg + Pseudoephdrine Hcl 30mg + Chlorpheniramine maleate 2mg. 2 Cetal Oral Drops Paracetamol 10% 3 Cetal Sinus Tab Paracetamol 500mg + Pseudoephdrine Hcl30mg 4 Cetal Extra Paracetamol D.C 500 mg + Caffiene anhydrous 65 mg 5 Cetal Supp 120 mg Paracetamol 120mg / supp. 6 Cetal Rectal Supp* 300 mg Paracetamol 300/Supp 7 Cetal Suspension Paracetamol 5% 8 Cetal Syrup Paracetamol 2.4% 9 Cetal Tab Paracetamol 500mg /tab. Pseudoephedrine HCl 30 mg 10 Conta-flu tablets +Chlorpheniramine maleate 3 mg 1.2.Analgesics ,Antiinflammatories & Antirheumatics 11 Epifenac 12.5 mg Rectal suppositories Diclofenac sodium 12.5 mg/supp. 12 Epifenac 25 mg Enteric coated tablets Diclofenac sodium 25 mg / ECT 13 Epifenac 25 mg Rectal suppositories Diclofenac sodium 25 mg/supp. 14 Epifenac 50 mg Enteric coated tablets Diclofenac sodium 50 mg/ ECT 15 Epifenac 50 mg Rectal suppositories Diclofenac sodium Micronised 50mg/Supp 16 Epifenac 75 mg Sustained Release sugar coated Tablets (T) Diclofenac sodium Micronised 75 mg/ SR SCT 17 Epifenac 100 mg Rectal suppositories Diclofenac sodium 100 mg/supp. 18 Epifenac 100 mg Sustained Release sugar coated Tablets (T) Diclofenac sodium Micronised 100 mg/SR SCT 19 Epifenac ampoule for IM injection or IV infusion Diclofenac sodium 75 mg / 3 ml 20 Epicotil 20 mg film coated tablets Tenoxicam 20 mg /FCT 21 Epicotil 20 mg suppository -

Sulfa Allergy: Cross-Reactivity Versus Multiple Concurrent Allergies
American Journal of Infectious Diseases 9 (4): 148-154, 2013 ISSN: 1553-6203 ©2013 Science Publication doi:10.3844/ajidsp.2013.148.154 Published Online 9 (4) 2013 (http://www.thescipub.com/ajid.toc) Sulfa Allergy: Cross-Reactivity Versus Multiple Concurrent Allergies 1Muhammad Tariq Shakoor, 2Samia Ayub and 3Zunaira Ayub 1Resident Physician, Internal Medicine Department, St Mary Mercy Hospital, Livonia, MI, USA 2Resident Physicain, Internal Medicine Department, Mount Auburn Hospital, Cambridge, MA, USA 3Medical Student, Fatima Jinnah Medical College, Lahore, Pakistan Received 2012-10-13, Revised 2013-05-01; Accepted 2013-12-02 ABSTRACT As a medical resident we have always been taught that there is some sort of cross reactivity between sulfonamide antibiotics and nonantibiotic sulfonamides. Even the manufacturer’s package inserts contain a precautionary statement about possible Cross-reactivity. The most common approach to this problem is avoidance of all sulfa containing drugs. However, there are few data supporting this contraindication. Thus we may be withholding appropriate therapies from patients unnecessarily. To provide a critical and comprehensive review of literature to explore either cross reactivity between sulfonamide antibiotics and nonantibiotic sulfonamides is a fact or fiction and to present an approach to use nonantibiotic sulfonamides in sulfa allergic patients. A PubMed and general medline search was conducted using the individual names of nonantibiotic sulfonamides. We reviewed all of the available case reports and studies regarding sulfonamide antibiotic cross-reactivity with nonantibiotic sulfonamides. Also reviewed the manufacturer’s package insert for each nonantibiotic sulfonamide drug for information concerning possible cross-reactivity with sulfonamide antibiotics. Sulfa drug allergy is one word holding the whole cross-reactivity theory in it. -

Review of Existing Classification Efforts
Project No. TREN-05-FP6TR-S07.61320-518404-DRUID DRUID Driving under the Influence of Drugs, Alcohol and Medicines Integrated Project 1.6. Sustainable Development, Global Change and Ecosystem 1.6.2: Sustainable Surface Transport 6th Framework Programme Deliverable 4.1.1 Review of existing classification efforts Due date of deliverable: (15.01.2008) Actual submission date: (07.02.2008) Start date of project: 15.10.2006 Duration: 48 months Organisation name of lead contractor for this deliverable: UGent Revision 1.0 Project co-funded by the European Commission within the Sixth Framework Programme (2002-2006) Dissemination Level PU Public X PP Restricted to other programme participants (including the Commission Services) RE Restricted to a group specified by the consortium (including the Commission Services) CO Confidential, only for members of the consortium (including the Commission Services) Task 4.1 : Review of existing classification efforts Authors: Kristof Pil, Elke Raes, Thomas Van den Neste, An-Sofie Goessaert, Jolien Veramme, Alain Verstraete (Ghent University, Belgium) Partners: - F. Javier Alvarez (work package leader), M. Trinidad Gómez-Talegón, Inmaculada Fierro (University of Valladolid, Spain) - Monica Colas, Juan Carlos Gonzalez-Luque (DGT, Spain) - Han de Gier, Sylvia Hummel, Sholeh Mobaser (University of Groningen, the Netherlands) - Martina Albrecht, Michael Heiβing (Bundesanstalt für Straßenwesen, Germany) - Michel Mallaret, Charles Mercier-Guyon (University of Grenoble, Centre Regional de Pharmacovigilance, France) - Vassilis Papakostopoulos, Villy Portouli, Andriani Mousadakou (Centre for Research and Technology Hellas, Greece) DRUID 6th Framework Programme Deliverable D.4.1.1. Revision 1.0 Review of Existing Classification Efforts Page 2 of 127 Introduction DRUID work package 4 focusses on the classification and labeling of medicinal drugs according to their influence on driving performance. -

High Performance Liquid Chromatography for Simultaneous Determination of Xipamide, Triamterene and Hydrochlorothiazide in Bulk Drug Samples and Dosage Forms
Acta Pharm. 66 (2016) 109–118 Original research paper DOI: 10.1515/acph-2016-0022 High performance liquid chromatography for simultaneous determination of xipamide, triamterene and hydrochlorothiazide in bulk drug samples and dosage forms SOAD S. ABD EL-HAY1, 2 A novel, simple and robust high-performance liquid chro- 2, 3 HISHAM HASHEM matography (HPLC) method was developed and validated AYMAN A. GOUDA4 for simultaneous determination of xipamide (XIP), triam- terene (TRI) and hydrochlorothiazide (HCT) in their bulk 1 Faculty of Pharmacy powders and dosage forms. Chromatographic separation Pharmaceutical Chemistry Department was carried out in less than two minutes. The separation King Abdulaziz University was performed on a RP C-18 stationary phase with an iso- Saudi Arabia cratic elution system consisting of 0.03 mol L–1 orthophos- phoric acid (pH 2.3) and acetonitrile (ACN) as the mobile 2 Faculty of Pharmacy phase in the ratio of 50:50, at 2.0 mL min–1 fl ow rate at room Department of Analytical Chemistry temperature. Detection was performed at 220 nm. Valida- Zagazig University, Egypt tion was performed concerning system suitability, limits of detection and quantitation, accuracy, precision, linearity 3 Faculty of Pharmacy and robustness. Calibration curves were rectilinear over Pharmaceutical Chemistry Department the range of 0.195–100 μg mL–1 for all the drugs studied. Jazan University, Saudi Arabia Recovery values were 99.9, 99.6 and 99.0 % for XIP, TRI and HCT, respectively. The method was applied to simultane- 4 Faculty of Science ous determination of the studied analytes in their pharma- Department of Analytical Chemistry ceutical dosage forms. -

Diuretics in the Treatment of Patients Who Present Congestive Heart Failure and Hypertension
Journal of Human Hypertension (2002) 16 (Suppl 1), S104–S113 2002 Nature Publishing Group All rights reserved 0950-9240/02 $25.00 www.nature.com/jhh Diuretics in the treatment of patients who present congestive heart failure and hypertension AJ Reyes Institute of Cardiovascular Theory, Montevideo, Uruguay The main operational objective of diuretic therapy in ment natriuresis in patients with congestive heart failure patients who present congestive heart failure and hyper- and hypertension. The state of renal function, the exis- tension is to reduce or to suppress excess bodily fluid. tence of certain co-morbid conditions, potential Effective diuretic therapy decreases cardiac size when untoward drug actions, and possible interactions of the heart is dilated, and it reduces lung congestion and diuretics with nutrients and with other drugs are some excess water. Consequently, external respiratory work of the factors that must be considered at the time of diminishes and cardiac output would be redistributed in deciding on the diuretic drug(s) and dose(s) to be pre- favour of systemic vascular beds other than that of the scribed. Spironolactone has been found to increase life respiratory muscles; dyspnoea decreases markedly and expectancy and to reduce hospitalisation frequency there is a slight reduction in fatigue. This clinical when added to the conventional therapeutic regimen of improvement and the fall in body weight caused by patients with advanced congestive heart failure and sys- diuretics entail an increase in effort capacity. Sub- tolic dysfunction. Therefore, spironolactone should be sequent exercise training ameliorates the abnormal ven- the drug of choice to oppose the kaliuretic effect of a tilatory response to physical effort and the skeletal mus- loop or of a thiazide-type diuretic. -
PRAC Recommendations on Signals Adopted at the 9-12 March 2020 PRAC Meeting
6 April 20201 EMA/PRAC/111214/2020 Corr2,3,4 Pharmacovigilance Risk Assessment Committee (PRAC) PRAC recommendations on signals Adopted at the 9-12 March 2020 PRAC meeting This document provides an overview of the recommendations adopted by the Pharmacovigilance Risk Assessment Committee (PRAC) on the signals discussed during the meeting of 9-12 March 2020 (including the signal European Pharmacovigilance Issues Tracking Tool [EPITT]5 reference numbers). PRAC recommendations to provide supplementary information are directly actionable by the concerned marketing authorisation holders (MAHs). PRAC recommendations for regulatory action (e.g. amendment of the product information) are submitted to the Committee for Medicinal Products for Human Use (CHMP) for endorsement when the signal concerns Centrally Authorised Products (CAPs), and to the Co-ordination Group for Mutual Recognition and Decentralised Procedures – Human (CMDh) for information in the case of Nationally Authorised Products (NAPs). Thereafter, MAHs are expected to take action according to the PRAC recommendations. When appropriate, the PRAC may also recommend the conduct of additional analyses by the Agency or Member States. MAHs are reminded that in line with Article 16(3) of Regulation No (EU) 726/2004 and Article 23(3) of Directive 2001/83/EC, they shall ensure that their product information is kept up to date with the current scientific knowledge including the conclusions of the assessment and recommendations published on the European Medicines Agency (EMA) website (currently acting as the EU medicines webportal). For CAPs, at the time of publication, PRAC recommendations for update of product information have been agreed by the CHMP at their plenary meeting (23-26 March 2020) and corresponding variations will be assessed by the CHMP.