ICD-10 Guide for Common Non-Malignant Blood Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Evans Syndrome As Rare Presentation in Systemic Lupus Erythematosus
International Journal of Health Sciences and Research www.ijhsr.org ISSN: 2249-9571 Case Report Evans Syndrome as Rare Presentation in Systemic Lupus Erythematosus Dr Sabarish Mahalingam1, Dr P. Z. Wadia2, Dr Priyanka Lad1 1Resident Doctor, Department of Internal Medicine, Government Medical College, Surat 2Additional Professor, Department of Internal Medicine, Government Medical College, Surat Corresponding Author: Dr Sabarish Mahalingam ABSTRACT Evans syndrome is a rare disorder in which the body’s immune system produces antibodies that mistakenly destroy red blood cells, platelets and sometimes certain white blood cell known as neutrophils. It is one of the rare presenting features of autoimmune disorders, especially systemic lupus erythematosus (SLE), and sometimes may even precede the onset of disease. Primary Evans syndrome with no cause is very rare and is seen in children. Here, we describe a case of secondary Evans syndrome with severe autoimmune hemolytic anemia leading to acute kidney injury. This is one of the rare presentations of SLE and there are only few case reports. Key word: Evans syndrome, systemic lupus erythematosus, autoimmune haemolytic anaemia. INTRODUCTION literature; [9-11] therefore, the characteristics Evans syndrome (ES), which was and outcome of adult's ES are poorly first described in 1951, is an autoimmune known. disorder characterized by the simultaneous or sequential development of autoimmune CASE REPORT hemolytic anemia (AIHA) and immune A 28 aged female came to (ITP) and/or immune neutropenia in the emergency department with the complain of absence of any underlying cause. [1,2] ES has breathlessness for past 5 days. On been since its first description considered or examination, patient was pale and defined as an “idiopathic” condition and tachypneic, systemic examination was thus mainly as a diagnosis of exclusion, ES normal. -

Case Report Treatment of Severe Evans Syndrome with an Allogeneic Cord Blood Transplant
Bone Marrow Transplantation, (1997) 20, 427–429 1997 Stockton Press All rights reserved 0268–3369/97 $12.00 Case report Treatment of severe Evans syndrome with an allogeneic cord blood transplant E Raetz1, PG Beatty2 and RH Adams1 Departments of 1Pediatrics and 2Medicine, University of Utah School of Medicine, Salt Lake City, UT, USA Summary: began experiencing increased difficulty with mucosal bleeding, which prompted frequent platelet transfusions. At Immunosuppressive therapy is commonly used in the 4. years, he had a major gastrointestinal bleed, followed management of autoimmune disorders. As marrow- 1 month later by an intracranial hemorrhage. He required derived lymphocytes appear to play a key role in these transient ventilator support, but eventually regained full diseases, lymphoid ablation followed by replacement neurologic function. Direct (DAT) and indirect (IAT) with autologous or allogeneic stem cells may be a thera- Coombs evaluations were always 3+ positive. Due to the peutic option. We report a 5-year-old boy with severe severe and refractory nature of his disease, the option of Evans syndrome which consists of immune thrombocy- novel therapy with bone marrow transplantation was topenia and Coombs-positive hemolytic anemia. He was pursued. rendered into complete remission with marrow ablation HLA typing of the family, and a search of the unrelated followed by rescue with an HLA-identical sibling cord marrow donor registries, did not identify an appropriate blood transplant. He unexpectedly died 9 months donor, but DNA-based typing for HLA-A, -B, -DRB1 of following transplant from acute hepatic failure of the amniotic fluid of a sibling fetus, of 6 months gestational unknown etiology. -
Simultaneous Pure Red Cell Aplasia and Auto-Immune Hemolytic Anemia in a Previously Healthy Infant
Simultaneous Pure Red Cell Aplasia and Auto-immune Hemolytic Anemia in a Previously Healthy Infant Robert P. Sanders, MD July 16, 2002 Case Presentation Patient Z.H. • Previously Healthy 7 month old WM • Presented to local ER 6/30 with 1 wk of decreased activity and appetite, low grade temp, 2 day h/o pallor. • Noted to have severe anemia, transferred to LeBonheur • Review of Systems – ? Single episode of dark urine – 4 yo sister diagnosed with Fifth disease 1 wk prior to onset of symptoms, cousin later also diagnosed with Fifth disease – Otherwise negative ROS •PMH – Term, no complications – Normal Newborn Screen – Hospitalized 12/01 with RSV • Medications - None • Allergies - NKDA • FH - Both parents have Hepatitis C (pt negative) • SH - Lives with Mom, 4 yo sister • Development Normal Physical Exam • 37.2 167 33 84/19 9.3kg • Gen - Alert, pale, sl yellow skin tone, NAD •HEENT -No scleral icterus • CHEST - Clear • CV - RRR, II/VI SEM at LLSB • ABD - Soft, BS+, no HSM • SKIN - No Rash • NEURO - No Focal Deficits Labs •CBC – WBC 20,400 • 58% PMN 37% Lymph 4% Mono 1 % Eo – Hgb 3.4 • MCV 75 MCHC 38.0 MCH 28.4 – Platelets 409,000 • Retic 0.5% • Smear - Sl anisocytosis, Sl hypochromia, Mod microcytes, Sl toxic granulation • G6PD Assay 16.6 U/g Hb (nl 4.6-13.5) • DAT, Broad Spectrum Positive – IgG negative – C3b, C3d weakly positive • Chemistries – Total Bili 2.0 – Uric Acid 4.8 –LDH 949 • Urinalysis Negative, Urobilinogen 0.2 • Blood and Urine cultures negative What is your differential diagnosis? Differential Diagnosis • Transient Erythroblastopenia of Childhood • Diamond-Blackfan syndrome • Underlying red cell disorder with Parvovirus induced Transient Aplastic Crisis • Immunohemolytic anemia with reticulocytopenia Hospital Course • Admitted to ICU for observation, transferred to floor 7/1. -

Case Report Evans Syndrome
Bangladesh Med J. 2018 Sept; 47(3) Case Report Evans Syndrome: A Case Report *Biswas SK1, BiswasT2, Khondoker N3, Alam MR4, Rahim MA5, Paul HK6, Shahin MA7, Hasan MN 8, Bhuiyan AKMM9 Abstract: INTRODUCTION Evans syndrome, a combined clinical condition of autoimmune Evans syndrome is an uncommon clinical condition de!ned haemolytic anaemia (AHA) and idiopathic thrombocytopaenic by the combination of autoimmune hemolytic anemia 1 purpura (ITP) and has non-speci!c pathogenesis. "e clinical (AHA) and idiopathic thrombocytopenic purpura (ITP). It cases are extremely rare, since only 4% of AHA or ITP are is a chronic immune- associated disease which has unknown incorporated with Evans. It is distinguished from di#erentials, pathophysiology. "e true Evans syndrome is diagnosed such as lupus, IgA de!ciency, and acquired immunode!ciency, when possibility of other confounding disorders is excluded. by peripheral blood !lm, bone marrow, Coombs test, and In 1951, Dr. Robert Evan discovered the spectrum like coagulation pro!le. A case of adult female from Pabna, relationship between these two combined diseases after 1 Bangladesh is documented in this report. She complained of studying twenty-four cases. Epidemiologically, the high grade intermittent fever, exertional dyspnea, icteric skin condition is extremely rare that only less than 4% of ITP or 2-5 and sclera. Other features included mild splenomegaly, dark AHA are diagnosed as Evans syndrome. "ere is evidence urine, and profuse sweating after fever. Investigation reports of both cellular and humoral immune-abnormalities in 6 were consistent with AHA and ITP, with normal coagulation Evans syndrome. Di#erent scientists provided di#erent and viral pro!le. -
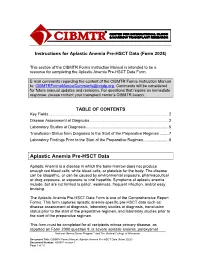
Aplastic Anemia Pre-HSCT Data (Form 2028)
Instructions for Aplastic Anemia Pre-HSCT Data (Form 2028) This section of the CIBMTR Forms Instruction Manual is intended to be a resource for completing the Aplastic Anemia Pre-HSCT Data Form. E-mail comments regarding the content of the CIBMTR Forms Instruction Manual to: [email protected]. Comments will be considered for future manual updates and revisions. For questions that require an immediate response, please contact your transplant center’s CIBMTR liaison. TABLE OF CONTENTS Key Fields ............................................................................................................. 2 Disease Assessment at Diagnosis ........................................................................ 2 Laboratory Studies at Diagnosis ........................................................................... 5 Transfusion Status from Diagnosis to the Start of the Preparative Regimen ........ 7 Laboratory Findings Prior to the Start of the Preparative Regimen ....................... 8 Aplastic Anemia Pre-HSCT Data Aplastic Anemia is a disease in which the bone marrow does not produce enough red blood cells, white blood cells, or platelets for the body. The disease can be idiopathic, or can be caused by environmental exposure, pharmaceutical or drug exposure, or exposure to viral hepatitis. Symptoms of aplastic anemia include, but are not limited to pallor, weakness, frequent infection, and/or easy bruising. The Aplastic Anemia Pre-HSCT Data Form is one of the Comprehensive Report Forms. This form captures aplastic -

Immune-Mediated Hemolytic Anemia and Thrombocytopenia in Clonal B-Cell Disorders: a Review
Immune-Mediated Hemolytic Anemia and Thrombocytopenia in Clonal B-Cell Disorders: A Review Urshila Durani, MD, MPH, Ronald S. Go, MD, and Neil E. Kay, MD The authors are affiliated with the Abstract: Autoimmune hemolytic anemia (AIHA) and immune Division of Hematology in the Depart- thrombocytopenia purpura (ITP) have been associated with B-cell ment of Medicine at the Mayo Clinic lymphoproliferative disorders. Here, we review the epidemiology, in Rochester, Minnesota. Dr Durani pathogenesis, diagnosis, and treatment of these autoimmune disor- is a fellow, Dr Go is an associate ders, specifically in the setting of B-cell malignancies. AIHA and ITP professor of medicine, and Dr Kay is a professor of medicine. are classically associated with chronic lymphocytic leukemia (CLL) but have also been reported in plasmacytic and lymphoprolifera- tive disorders. AIHA includes both warm AIHA and cold agglutinin Corresponding author: disease, the latter of which is strongly associated with Walden- Neil E. Kay, MD ström macroglobulinemia. The pathogenesis of these cytopenias Mayo Clinic varies with the underlying disease, but malignant cells serving as 200 First St SW Rochester, MN 55905 antigen-presenting cells to T lymphocytes, with the generation of Tel: (507) 284-2511 autoreactive lymphocytes, may be involved. The diagnosis requires E-mail: [email protected] the presence of hemolysis and a positive direct antiglobulin test result. In a minority of cases, the direct antiglobulin test result is negative, and more specialized testing may be required. Data on the prognostic effect of these comorbidities are conflicting, and the prognosis may vary depending on when in the B-cell malignant process the cytopenia(s) develops. -

An Incidental Case of Transient Erythroblastopenia of Childhood
Clinical Pediatrics: Open Access Case Report An Incidental Case of Transient Erythroblastopenia of Childhood Allen Mao1*, Brian Gavan2, Curtis Turner3 1University of South Alabama, College of Medicine, Mobile, Alabama, USA;2Department of Pediatrics, University of South Alabama Children’s and Women’s Hospital, Mobile, Alabama, USA;3Department of Pediatrics, University of South Alabama Children’s and Women’s Hospital, Mobile, Alabama, USA ABSTRACT We highlight a pediatric case of Transient Erythroblastopenia of Childhood (TEC) and compare with published reports and contrast TEC with other causes of anemia, most notably Diamond Blackfan Anemia (DBA). Secondly, many of the business. The development of anemia may be subtle, and TEC is a diagnosis of exclusion. The broad differential diagnoses of anemia include decreased RBC production (erythropoiesis) or increased RBC destruction (hemolytic anemias). Decreased RBC production includes viral suppression and bone marrow failure (congenital or acquired). Keywords: Hepatosplenomegaly; Anemia; Erythroblastopenia; Echovirus INTRODUCTION CASE PRESENTATION Transient Erythroblastopenia of Childhood (TEC) is Our patient was a healthy 12 month old African American male characterized by a temporary cessation of erythrocyte production with no significant past medical history who presented for a well- with continued production of white blood cells and platelets in child checkup. Screening CBC and lead level were obtained. His previously healthy children. This is the most common Pediatric vital signs were temperature 36.6°C, pulse 136, and respiratory Pure Red Cell Aplasia (PRCA), an isolated anemia with rate 28. The physical exam was significant for mild conjunctival reticulocytopenia [1]. The etiology is unknown, yet suspected pallor, his height was in the 89th percentile, weight in 42nd causes of Transient Erythroblastopenia of Childhood (TEC) percentile, and he had no abnormal facies, digit abnormalities, include preceding viral illnesses (e.g. -

503 © Springer Nature Switzerland AG 2021 D. M. Kamat, M. Frei
Index A Acute splenic sequestration crisis (ASSC), 71 Abnormal chromosomal breakage test, 387 Adenosine deaminase activity (ADA), 372 ABO hemolytic disease, 325 Allo-immune thrombocytopenia, 116 Acquired aplastic anemia (AAA) Alternative pathway, 489 clinical features, 371 Anemia, 323, 326 definition and classifications, 371 chronic disease, 375, 376 diagnosis and management, 371 congenital dyserythropoietic anemias, 381 etiology and pathogenesis, 371 fanconi anemia, 374, 375 incidence, 370 folic acid deficiency, 380, 381 Acquired disorders of coagulation iron deficiency anemia, 377–379 coaguloapathy vitamin B12 deficiency, 379, 380 liver failure, 264 ANKRD26-related thrombocytopenia massive transfusion, 264, 265 (ANKRD26-RT), 143 disseminated intravascular Anticoagulation therapy, 348–350 coagulation, 261–263 Antiphospholipid antibodies (APAs), 273 platelet dysfunction, renal failure, 263 Antithrombin (AT) deficiency, 272 sepsis Aplastic anemia (AA) consensus definition, 259 clinical presentation, 393 multiple hematologic diagnosis and severity stratification, manifestations, 259 393, 395 organ injury, 260 differential diagnosis, 393 pathogenesis, 260 eltrombopag, 397 TAMOF, 261 epidemiology, 391 TTP, 261 etiology, 392 Acquired thromboembolic events, 346 hematopoietic stem cell transplant, 398 Acquired von Willebrand Syndrome (AVWS) idiopathic AA, 391 definition, 240 immunosuppressive therapy, 396 diagnosis, 240–242 infection prevention and treatment, 396 management, 242–244 pathophysiology, 392 pathophysiology, 240 transfusion support, -

Evans' Syndrome
Journal of Clinical Medicine Review Evans’ Syndrome: From Diagnosis to Treatment Sylvain Audia 1,* , Natacha Grienay 1, Morgane Mounier 2, Marc Michel 3 and Bernard Bonnotte 1 1 Service de Médecine Interne et Immunologie Clinique, Centre de Référence Constitutif des Cytopénies Auto-Immunes de l’Adulte, Centre Hospitalo-Universitaire Dijon Bourgogne, Université de Bourgogne Franche Comté, 21000 Dijon, France; [email protected] (N.G.); [email protected] (B.B.) 2 Registre des Hémopathies Malignes de Côte d’Or, Centre Hospitalo-Universitaire Dijon Bourgogne, Université de Bourgogne Franche Comté, UMR 1231 Dijon, 21000 Dijon, France; [email protected] 3 Service de Médecine Interne 1, Centre de Référence des Cytopénies Auto-Immunes de l’Adulte, Centre Hospitalo-Universitaire Henri Mondor, 94000 Créteil, France; [email protected] * Correspondence: [email protected]; Tel.: +333-80-29-34-32 Received: 11 October 2020; Accepted: 25 November 2020; Published: 27 November 2020 Abstract: Evans’ syndrome (ES) is defined as the concomitant or sequential association of warm auto-immune haemolytic anaemia (AIHA) with immune thrombocytopenia (ITP), and less frequently autoimmune neutropenia. ES is a rare situation that represents up to 7% of AIHA and around 2% of ITP. When AIHA and ITP occurred concomitantly, the diagnosis procedure must rule out differential diagnoses such as thrombotic microangiopathies, anaemia due to bleedings complicating ITP, vitamin deficiencies, myelodysplastic syndromes, paroxysmal nocturnal haemoglobinuria, or specific conditions like HELLP when occurring during pregnancy. As for isolated auto-immune cytopenia (AIC), the determination of the primary or secondary nature of ES is important. Indeed, the association of ES with other diseases such as haematological malignancies, systemic lupus erythematosus, infections, or primary immune deficiencies can interfere with its management or alter its prognosis. -

Hemophilia Update 2015
J. Martin Johnston, MD Pediatric Project ECHO 7 December 2018 Objectives Review history and physical exam as they relate to a potential bleeding disorder Discuss step-wise laboratory evaluation: screening labs and follow-ups Review some common congenital and acquired bleeding disorders, and their management Objectives Review history and physical exam as they relate to a potential bleeding disorder Discuss step-wise laboratory evaluation: screening labs and follow-ups Review some common congenital and acquired bleeding disorders, and their management Objectives Review history and physical exam as they relate to a potential bleeding disorder Discuss step-wise laboratory evaluation: screening labs and follow-ups Review some common congenital and acquired bleeding disorders, and their management The chief complaint “Easy” bruising Nosebleeds Petechiae Menorrhagia Bleeding after Circumcision Tonsillectomy/adenoidectomy, tooth extraction Mild (head) trauma The problem…. • Everyone bleeds. • All bleeding eventually stops. The bleeding history Birth/neonatal Tooth eruption/shedding Bruising Nosebleeds Surgeries? (don’t forget circumcision!) Orthopedic hx (traumas, joints) Menstruation Family history How much bleeding is too much? Neonatal ICH, needle/heel sticks, post-circumcision How much bleeding is too much? Neonatal ICH, needle/heel sticks, post-circumcision Infant Petechiae, chest/back/buttock bruising Consider NAT How much bleeding is too much? Neonatal ICH, needle/heel sticks, post-circumcision Infant -

Blood Toxicity Lab 7
6/22/2020 Blood toxicity lab 7 Blood Basics Blood is a specialized body fluid. It has four main components: plasma, red blood cells, white blood cells, and platelets. Blood has many different functions, including: 1-Transporting oxygen and nutrients to the lungs and tissues 2-Forming blood clots to prevent excess blood loss 3-Carrying cells and antibodies that fight infection 4-Bringing waste products to the kidneys and liver, which filter and clean the blood 5-Regulating body temperature 1 6/22/2020 Hematology: is the science or study of blood, blood-forming organs and blood diseases. In the medical field, hematology includes the treatment of blood disorders and malignancies, including types of hemophilia, leukemia, lymphoma and sickle-cell anemia. Hematotoxicology : is the study of adverse effects of drugs, nontherapeutic chemicals, and other chemicals in our environment on blood and blood-forming tissues. Each of the various blood cells (erythrocytes, granulocytes, and platelets) is produced at a rate of approximately one to three million/s in a healthy adult and several times that rate in conditions where demand for these cells is high, as in hemolytic anemia or suppurative inflammation. The hematopoietic tissue is also susceptible to : 1-The secondary effects of toxic agents that affect the supply of nutrients, such as iron 2- The clearance of toxins and metabolites, such as urea 3- The production of vital growth factors, such as erythropoietin and granulocyte colony- stimulating factor(G-CSF). 2 6/22/2020 The consequences of direct or indirect damage to blood cells and their precursors are predictable and potentially life-threatening. -

Evans Syndrome
CASE REPORT Evans Syndrome Ahmed Al Hazmi, MBBS* *University of Maryland Medical Center, Department of Emergency Medicine, Michael E. Winters, MD, MBA† Baltimore, Maryland †University of Maryland School of Medicine, Department of Emergency Medicine, Baltimore, Maryland Section Editor: Steven Walsh, MD Submission history: Submitted September 22, 2018; Revision received December 31, 2019; Accepted January 23, 2019 Electronically published February 26, 2019 Full text available through open access at http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.2019.1.41028 A 22-year-old man presented to the emergency department with facial swelling, rash, and fatigue. He had a past medical history of pericarditis and pericardial effusion. His evaluation showed anemia and thrombocytopenia. He was admitted for intravenous administration of steroids, plasmapheresis, and workup of his anemia and thrombocytopenia. He was ultimately diagnosed with Evans syndrome as a presenting feature of systemic lupus erythematosus. Plasmapheresis was stopped but administration of steroids continued. His blood counts improved, and the facial swelling and rash subsided. Evans syndrome is an immunologic conundrum that requires early recognition and treatment. [Clin Pract Cases Emerg Med. 2019;3(2):128-131.] INTRODUCTION the chief complaint of facial swelling, which had been present Evans syndrome (ES) is a very rare autoimmune disease for the prior three weeks. The swelling was predominantly on first described in 1951. It is the combination of Coombs- the right side of his face and upper lip. He had no history of positive idiopathic autoimmune hemolytic anemia (IAHA) angioedema, had not started any new medications, and was not and immune thrombocytopenic purpura (ITP).1-3 In addition, aware of an environmental exposure that immediately preceded ES can be associated with the development of neutropenia the onset of swelling.