Newer Bronchodilators
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
New Zealand Data Sheet
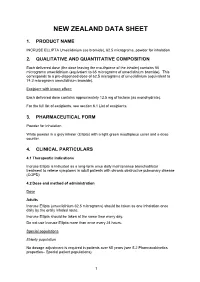
NEW ZEALAND DATA SHEET 1. PRODUCT NAME INCRUSE ELLIPTA Umeclidinium (as bromide), 62.5 micrograms, powder for inhalation 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each delivered dose (the dose leaving the mouthpiece of the inhaler) contains 55 micrograms umeclidinium (equivalent to 65 micrograms of umeclidinium bromide). This corresponds to a pre-dispensed dose of 62.5 micrograms of umeclidinium (equivalent to 74.2 micrograms umeclidinium bromide). Excipient with known effect: Each delivered dose contains approximately 12.5 mg of lactose (as monohydrate). For the full list of excipients, see section 6.1 List of excipients. 3. PHARMACEUTICAL FORM Powder for Inhalation White powder in a grey inhaler (Ellipta) with a light green mouthpiece cover and a dose counter. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Incruse Ellipta is indicated as a long-term once daily maintenance bronchodilator treatment to relieve symptoms in adult patients with chronic obstructive pulmonary disease (COPD). 4.2 Dose and method of administration Dose Adults Incruse Ellipta (umeclidinium 62.5 micrograms) should be taken as one inhalation once daily by the orally inhaled route. Incruse Ellipta should be taken at the same time every day. Do not use Incruse Ellipta more than once every 24 hours. Special populations Elderly population No dosage adjustment is required in patients over 65 years (see 5.2 Pharmacokinetics properties– Special patient populations). 1 Renal impairment No dosage adjustment is required in patients with renal impairment (see 5.2 Pharmacokinetics properties – Special patient populations). Hepatic impairment No dosage adjustment is required in patients with mild or moderate hepatic impairment. Incruse Ellipta has not been studied in patients with severe hepatic impairment (see 5.2 Pharmacokinetics properties– Special patient populations). -

Stable Pressurised Aerosol Solution Composition of Glycopyrronium Bromide and Formoterol Combination
(19) TZZ¥¥_T (11) EP 3 384 898 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 10.10.2018 Bulletin 2018/41 A61K 9/00 (2006.01) A61M 15/00 (2006.01) A61K 31/167 (2006.01) A61K 31/40 (2006.01) (2006.01) (2006.01) (21) Application number: 18171127.6 B65D 83/54 A61K 31/573 A61K 31/54 (2006.01) A61K 45/06 (2006.01) (2006.01) (2006.01) (22) Date of filing: 23.12.2014 A61K 9/12 A61K 31/58 A61M 39/22 (2006.01) (84) Designated Contracting States: • COPELLI, Diego AL AT BE BG CH CY CZ DE DK EE ES FI FR GB 43100 PARMA (IT) GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO • DAGLI ALBERI, Massimiliano PL PT RO RS SE SI SK SM TR 43100 PARMA (IT) Designated Extension States: • USBERTI, Francesca BA ME 43100 PARMA (IT) • ZAMBELLI, Enrico (30) Priority: 30.12.2013 EP 13199784 43100 PARMA (IT) (62) Document number(s) of the earlier application(s) in (74) Representative: Bianchetti Bracco Minoja S.r.l. accordance with Art. 76 EPC: Via Plinio, 63 14825154.9 / 3 089 735 20129 Milano (IT) (71) Applicant: Chiesi Farmaceutici S.p.A. Remarks: 43100 Parma (IT) This application was filed on 08-05-2018 as a divisional application to the application mentioned (72) Inventors: under INID code 62. • BONELLI, Sauro 43100 PARMA (IT) (54) STABLE PRESSURISED AEROSOL SOLUTION COMPOSITION OF GLYCOPYRRONIUM BROMIDE AND FORMOTEROL COMBINATION (57) The invention concerns an aerosol solution lower than the limit of quantification, when stored in ac- composition intended for use with a pressurised metered celerated conditions at 25°C and 60% relative humidity dose inhaler, comprising glycopyrronium bromide and (RH) for 6 months in a can internally coated by a resin formoterol, or a salt thereof or a solvate of said salt, op- comprising a fluorinated ethylene propylene (FEP) poly- tionally in combination with one or more additional active mer. -

Hypersalivation in Children and Adults
Pharmacological Management of Hypersalivation in Children and Adults Scope: Adult patients with Parkinson’s disease, children with neurodisability, cerebral palsy, long-term ventilation with drooling, and drug-induced hypersalivation. ASSESSMENT OF SEVERITY/RESPONSE TO TREATMENT: Severity of drooling can be assessed subjectively via discussion with patients and their carers/parents and by observation. Amount of drooling can be quantified by measuring the number of bibs required per day and this can also be graded using the Thomas-Stonell and Greenberg scale: • 1 = Dry (no drooling) • 2 = Mild (moist lips) • 3 = Moderate (wet lips and chin) • 4 = Severe (damp clothing) CONSIDERATIONS FOR PRESCRIBING/TITRATION No evidence to support the use of one particular treatment over another. Drug choice is to be determined by individual patient factors. When prescribing/titrating antimuscarinic drugs to treat hypersalivation always take account of: • Coexisting conditions (for example, history of urinary retention, constipation, glaucoma, dental issues, reflux etc.) • Use of other existing medication affecting the total antimuscarinic burden • Risk of adverse effects Titrate dose upward until the desired level of dryness, side effects or maximum dose reached. Take into account the preferences of the patients and their carers/ parents, and the age range and indication covered by the marketing authorisations (see individual summaries of product characteristics, BNF or BNFc for full prescribing information). FIRST LINE DRUG TREATMENT OPTIONS FOR ADULTS -

COPD Agents Review – October 2020 Page 2 | Proprietary Information
COPD Agents Therapeutic Class Review (TCR) October 1, 2020 No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage or retrieval system without the express written consent of Magellan Rx Management. All requests for permission should be mailed to: Magellan Rx Management Attention: Legal Department 6950 Columbia Gateway Drive Columbia, Maryland 21046 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended to be educational in nature and is intended to be used for informational purposes only. Send comments and suggestions to [email protected]. October 2020 -

New Zealand Data Sheet
NEW ZEALAND DATA SHEET 1. PRODUCT NAME TRELEGY ELLIPTA 100/62.5/25 fluticasone furoate (100 micrograms)/umeclidinium (as bromide) (62.5 micrograms)/vilanterol (as trifenatate) (25 micrograms), powder for inhalation 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each delivered dose (the dose leaving the mouthpiece of the inhaler) contains 92 micrograms fluticasone furoate, 55 micrograms umeclidinium (equivalent to 65 micrograms umeclidinium [as bromide]) and 22 micrograms vilanterol (as trifenatate). This corresponds to a pre-dispensed dose of 100 micrograms fluticasone furoate, 62.5 micrograms umeclidinium (equivalent to 74.2 micrograms umeclidinium bromide) and 25 micrograms vilanterol (as trifenatate). Excipient with known effect: Each delivered dose contains approximately 25 milligrams of lactose (as monohydrate). For the full list of excipients, see Section 6.1 List of excipients. 3. PHARMACEUTICAL FORM Powder for inhalation. White powder in a light grey inhaler (Ellipta) with a beige mouthpiece cover and a dose counter. 4. CLINICAL PARTICULARS 4.1. Therapeutic indications TRELEGY ELLIPTA is indicated for the maintenance treatment of adults with moderate to severe chronic obstructive pulmonary disease (COPD) who require treatment with a long- acting muscarinic receptor antagonist (LAMA) + long-acting beta2-receptor agonist (LABA) + inhaled corticosteroid (ICS). TRELEGY ELLIPTA should not be used for the initiation of COPD treatment. 4.2. Dose and method of administration Patients can be changed from their existing inhalers to TRELEGY ELLIPTA at the next dose. However it is important that patients do not take other LABA or LAMA or ICS while taking TRELEGY ELLIPTA. A stepwise approach to the management of COPD is recommended, including the cessation of smoking and a pulmonary rehabilitation program. -

1: Gastro-Intestinal System
1 1: GASTRO-INTESTINAL SYSTEM Antacids .......................................................... 1 Stimulant laxatives ...................................46 Compound alginate products .................. 3 Docuate sodium .......................................49 Simeticone ................................................... 4 Lactulose ....................................................50 Antimuscarinics .......................................... 5 Macrogols (polyethylene glycols) ..........51 Glycopyrronium .......................................13 Magnesium salts ........................................53 Hyoscine butylbromide ...........................16 Rectal products for constipation ..........55 Hyoscine hydrobromide .........................19 Products for haemorrhoids .................56 Propantheline ............................................21 Pancreatin ...................................................58 Orphenadrine ...........................................23 Prokinetics ..................................................24 Quick Clinical Guides: H2-receptor antagonists .......................27 Death rattle (noisy rattling breathing) 12 Proton pump inhibitors ........................30 Opioid-induced constipation .................42 Loperamide ................................................35 Bowel management in paraplegia Laxatives ......................................................38 and tetraplegia .....................................44 Ispaghula (Psyllium husk) ........................45 ANTACIDS Indications: -

West Sussex Health and Social Care NHS Trust
SUSSEX PARTNERSHIP NHS FOUNDATION TRUST MEDICINES FORMULARY GUIDELINE VERSION 26 RATIFYING GROUP (individual formulary Drugs and Therapeutics Group (DTG) decisions and linked guidelines) DATE PUBLISHED July 2021 NEXT REVIEW DATE July 2023 FORMULARY SPONSOR Chief Medical Officer FORMULARY EDITOR Chief Pharmacist LINKED POLICIES AND GUIDELINES Linked policies and antipsychotic Physical health linked guidelines guidelines • Antipsychotics, guidelines for cardiac • Antipsychotics, prescribing guidelines rhythm screening (ECGs) • Asenapine, prescribing guidelines • Antipsychotics, guidelines for the • Clozapine inpatient and community management of weight gain and team policies metabolic disturbances • Clozapine, protocol for the use of • Metformin, information for GPs on its intramuscular injection use with antipsychotics • Clopixol Acuphase, prescribing • Hyperprolactinaemia, prescribing guideline guidelines on the treatment of • Lurasidone, prescribing guidelines antipsychotic induced symptoms • Perinatal mental health, prescribing • Anticoagulants, prescribing guidelines guidelines • Insulin, prescribing guidelines • Rapid tranquilisation policy • Medicines code Long acting antipsychotic guidelines Anxiolytics and hypnotic guidelines • Long acting antipsychotic injections, • Alcohol and benzodiazepine guidelines for use dependence (adults), prescribing • Aripiprazole long acting injection, guidelines for inpatients • Benzodiazepine as anxiolytics (adults), prescribing guidelines prescribing guidelines • Olanzapine long-acting injection, -

Fluticasone Furoate and Vilanterol for the Treatment of Chronic Obstructive Pulmonary Disease
Expert Review of Respiratory Medicine ISSN: 1747-6348 (Print) 1747-6356 (Online) Journal homepage: http://www.tandfonline.com/loi/ierx20 Fluticasone furoate and vilanterol for the treatment of chronic obstructive pulmonary disease Gaetano Caramori, Paolo Ruggeri, Paolo Casolari, Kian Fan Chung, Giuseppe Girbino & Ian M. Adcock To cite this article: Gaetano Caramori, Paolo Ruggeri, Paolo Casolari, Kian Fan Chung, Giuseppe Girbino & Ian M. Adcock (2017): Fluticasone furoate and vilanterol for the treatment of chronic obstructive pulmonary disease, Expert Review of Respiratory Medicine, DOI: 10.1080/17476348.2017.1386564 To link to this article: http://dx.doi.org/10.1080/17476348.2017.1386564 Accepted author version posted online: 28 Sep 2017. Submit your article to this journal View related articles View Crossmark data Full Terms & Conditions of access and use can be found at http://www.tandfonline.com/action/journalInformation?journalCode=ierx20 Download by: [Imperial College London Library] Date: 29 September 2017, At: 01:13 Publisher: Taylor & Francis Journal: Expert Review of Respiratory Medicine DOI: 10.1080/17476348.2017.1386564 Review Fluticasone furoate and vilanterol for the treatment of chronic obstructive pulmonary disease Gaetano Caramori1*, Paolo Ruggeri1, Paolo Casolari2, Kian Fan Chung3, Giuseppe Girbino1, Ian M. Adcock3. 1Unità Operativa Complessa di Pneumologia, Dipartimento di Scienze Biomediche, Odontoiatriche e delle Immagini Morfologiche e Funzionali (BIOMORF) Università degli Studi di Messina, Italy. 2Centro Interdipartimentale per lo Studio delle Malattie Infiammatorie delle Vie Aeree e Patologie Fumo-correlate (CEMICEF; formerly Centro di Ricerca su Asma e BPCO), Sezione di Medicina Interna e Cardiorespiratoria, Università di Ferrara, Ferrara, Italy. 3Airways Disease Section, National Heart and Lung Institute, Royal Brompton Hospital Biomedical Research Unit, Imperial College London, UK. -

Long-Acting Beta-Agonists in the Management of Chronic Obstructive Pulmonary Disease: Current and Future Agents
UCLA UCLA Previously Published Works Title Long-acting beta-agonists in the management of chronic obstructive pulmonary disease: current and future agents Permalink https://escholarship.org/uc/item/7s74p6sc Journal Respiratory Research, 11(1) ISSN 1465-9921 Authors Tashkin, Donald P Fabbri, Leonardo M Publication Date 2010-10-29 DOI http://dx.doi.org/10.1186/1465-9921-11-149 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Tashkin and Fabbri Respiratory Research 2010, 11:149 http://respiratory-research.com/content/11/1/149 REVIEW Open Access Long-acting beta-agonists in the management of chronic obstructive pulmonary disease: current and future agents Donald P Tashkin1*, Leonardo M Fabbri2 Abstract Chronic obstructive pulmonary disease (COPD) is characterized by progressive airflow limitation and debilitating symptoms. For patients with moderate-to-severe COPD, long-acting bronchodilators are the mainstay of therapy; as symptoms progress, guidelines recommend combining bronchodilators from different classes to improve efficacy. Inhaled long-acting b2-agonists (LABAs) have been licensed for the treatment of COPD since the late 1990s and include formoterol and salmeterol. They improve lung function, symptoms of breathlessness and exercise limita- tion, health-related quality of life, and may reduce the rate of exacerbations, although not all patients achieve clini- cally meaningful improvements in symptoms or health related quality of life. In addition, LABAs have an acceptable safety profile, and are not associated with an increased risk of respiratory mortality, although adverse effects such as palpitations and tremor may limit the dose that can be tolerated. Formoterol and salmeterol have 12-hour durations of action; however, sustained bronchodilation is desirable in COPD. -

The Use of Stems in the Selection of International Nonproprietary Names (INN) for Pharmaceutical Substances
WHO/PSM/QSM/2006.3 The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances 2006 Programme on International Nonproprietary Names (INN) Quality Assurance and Safety: Medicines Medicines Policy and Standards The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 © World Health Organization 2006 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. -

Cdr Clinical Review Report for Incruse Ellipta
Common Drug Review Clinical Review Report January 2018 Drug umeclidinium bromide (Incruse Ellipta) Indicated for long-term, once daily maintenance bronchodilator treatment of airflow obstruction in patients with chronic obstructive Indication pulmonary disease (COPD), including chronic bronchitis and emphysema. List in a similar manner to other long-acting muscarinic antagonists Listing request (LAMAs) as a maintenance bronchodilator treatment for COPD. Dosage form(s) Dry powder for oral inhalation, 62.5 mcg per inhalation Manufacturer GlaxoSmithKline Canada Inc. (GSK) This review report was prepared by the Canadian Agency for Drugs and Technologies in Health (CADTH). In addition to CADTH staff, the review team included a clinical expert in respirology who provided input on the conduct of the review and the interpretation of findings. Disclaimer: The information in this document is intended to help Canadian health care decision-makers, health care professionals, health systems leaders, and policy-makers make well-informed decisions and thereby improve the quality of health care services. While patients and others may access this document, the document is made available for informational purposes only and no representations or warranties are made with respect to its fitness for any particular purpose. The information in this document should not be used as a substitute for professional medical advice or as a substitute for the application of clinical judgment in respect of the care of a particular patient or other professional judgment in any decision-making process. The Canadian Agency for Drugs and Technologies in Health (CADTH) does not endorse any information, drugs, therapies, treatments, products, processes, or services. While care has been taken to ensure that the information prepared by CADTH in this document is accurate, complete, and up-to-date as at the applicable date the material was first published by CADTH, CADTH does not make any guarantees to that effect. -

Patent Application Publication ( 10 ) Pub . No . : US 2019 / 0192440 A1
US 20190192440A1 (19 ) United States (12 ) Patent Application Publication ( 10) Pub . No. : US 2019 /0192440 A1 LI (43 ) Pub . Date : Jun . 27 , 2019 ( 54 ) ORAL DRUG DOSAGE FORM COMPRISING Publication Classification DRUG IN THE FORM OF NANOPARTICLES (51 ) Int . CI. A61K 9 / 20 (2006 .01 ) ( 71 ) Applicant: Triastek , Inc. , Nanjing ( CN ) A61K 9 /00 ( 2006 . 01) A61K 31/ 192 ( 2006 .01 ) (72 ) Inventor : Xiaoling LI , Dublin , CA (US ) A61K 9 / 24 ( 2006 .01 ) ( 52 ) U . S . CI. ( 21 ) Appl. No. : 16 /289 ,499 CPC . .. .. A61K 9 /2031 (2013 . 01 ) ; A61K 9 /0065 ( 22 ) Filed : Feb . 28 , 2019 (2013 .01 ) ; A61K 9 / 209 ( 2013 .01 ) ; A61K 9 /2027 ( 2013 .01 ) ; A61K 31/ 192 ( 2013. 01 ) ; Related U . S . Application Data A61K 9 /2072 ( 2013 .01 ) (63 ) Continuation of application No. 16 /028 ,305 , filed on Jul. 5 , 2018 , now Pat . No . 10 , 258 ,575 , which is a (57 ) ABSTRACT continuation of application No . 15 / 173 ,596 , filed on The present disclosure provides a stable solid pharmaceuti Jun . 3 , 2016 . cal dosage form for oral administration . The dosage form (60 ) Provisional application No . 62 /313 ,092 , filed on Mar. includes a substrate that forms at least one compartment and 24 , 2016 , provisional application No . 62 / 296 , 087 , a drug content loaded into the compartment. The dosage filed on Feb . 17 , 2016 , provisional application No . form is so designed that the active pharmaceutical ingredient 62 / 170, 645 , filed on Jun . 3 , 2015 . of the drug content is released in a controlled manner. Patent Application Publication Jun . 27 , 2019 Sheet 1 of 20 US 2019 /0192440 A1 FIG .