Ultrasound-Mediated Mesenchymal Stem Cells Transfection As A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
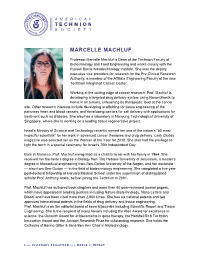
Marcelle Machluf
MARCELLE MACHLUF Professor Marcelle Machluf is Dean of the Technion Faculty of Biotechnology and Food Engineering and works closely with the Russell Berrie Nanotechnology Institute. She was the deputy executive vice president for research for the Pre-Clinical Research Authority, a member of the Affiliate Engineering Faculty of the new Technion Integrated Cancer Center. Working at the cutting edge of cancer research, Prof. Machluf is developing a targeted drug delivery system using Nano-Ghosts to home in on tumors, unleashing its therapeutic load at the cancer site. Other research interests include developing scaffolding for tissue engineering of the pancreas heart and blood vessels; and developing carriers for cell delivery with applications for treatment such as diabetes. She also has a laboratory in Nanyung Technological University of Singapore, where she is working on a leading tissue regenerative project. Israel’s Ministry of Science and Technology recently named her one of the nation’s “60 most impactful scientists” for her work in advanced cancer therapies and drug delivery. Lady Globes magazine also selected her as the Woman of the Year for 2018. She also had the privilege to light the torch in a special ceremony for Israel’s 70th Independent Day. Born in Morocco, Prof. Machluf immigrated as a child to Israel with her family in 1964. She received her bachelor’s degree in biology from The Hebrew University of Jerusalem, a master’s degree in biomedical engineering from Ben-Gurion University of the Negev, and her doctorate — also from Ben-Gurion — in the field of biotechnology engineering. She completed a five-year post-doctoral fellowship at Harvard Medical School under the supervision of distinguished scholar Prof. -

Innovation Report
Israel Innovation Authority’s 2019 Innovation Report Foreword by the CEO and Chairman of the Board of the Israel Innovation Authority The Israel Innovation Authority is proud to present its 2019 Innovation Report . These are unusual times. In recent weeks, the coronavirus outbreak (COVID-19) has caused economic upheaval to the Israeli economy and to the global economy at large. We are just beginning to grapple with the virus and its ramifications, but it is already clear that there will be profound consequences for the Israeli economy in general and for Israeli high-tech in particular. Israel’s high-tech sector, which has been an integral part of global innovation as a whole, will inevitably face momentous challenges and uncertainty. We are already witnessing a decline in international economic activity, stagnation in investments, and frequently imposed restrictions on the movement of people and goods. These constraints make groundbreaking innovation almost impossible to carry out. These are trying times for the Israel Innovation Authority as well. Israel’s transitional government is hindering its ability to advance legislation and policy, and is slowing down public budgeting mechanisms. In late 2019, this forced the Innovation Authority to delay payment to companies. Moreover, since there was no approved state budget at the outset of 2020, the Israel Innovation Authority was unable to provide new grants or to continue its funding of the Israeli innovation ecosystem. Nonetheless, we believe that the data presented in this report indicates that the Israeli high-tech sector is entering this coronavirus crisis in relatively good shape. 2019 was a record-breaking year for Israeli high-tech in all surveyed parameters: private capital raising, exports, the number of skilled tech workers, state revenue from taxes, and more. -

Detailed-Program
08:20-09:00 Registration, Morning Coffee & Mingling 09:00-09:20 Opening session 09:00 Assaf Zinger - Organizing Committee, Technion-Israel Institute of Technology 09:10 Prof. Dan Peer- ICRS President, Tel-Aviv University 09:20-10:00 Plenary Lecture TURNING CONTROLLED RELEASE TECHNOLOGY INTO PRODUCTS: THE STORY OF SOL-GEL Dr. Alon Seri-Levy- CEO, Sol-Gel Technologies 10:00-11:00 Session A: RNA/ DNA Delivery Systems & Imaging 10:00 BIO-INSPIRED ANIONIC NANOPARTICLES FOR DELIVERY OF PLASMID DNA Stav Shamir, Efrat Forti, Matan Goldstein, Smadar Cohen Avram and Stella Goldstein-Goren Department of Biotechnology Engineering, Ben-Gurion University of the Negev, Beer-Sheva, Israel 10:10 TARGETING PANCREATIC DUCTAL ADENOCARCINOMA WITH A POLYMERIC NANOCARRIER AND AN ANTICANCER MICRORNA POLYPLEX Hadas Gibori, Shay Eliyahu, Adva krivitsky and Ronit Satchi-Fainaro Department of Physiology and Pharmacology, Sackler School of Medicine, Tel-Aviv University, Tel-Aviv, Israel 10:20 SYSTEMIC GENE SILENCING IN PRIMARY T LYMPHOCYTES USING TARGETED LIPID NANOPARTICLES Ranit Kedmi1,2,3*, Srinivas Ramishetti1,2,3*, Meir Goldsmith1,2,3, Fransisca Leonard4, Andrew G. Sprague5, Biana Godin4, Michael Gozinz, Pieter R. Cullis6, Derek M. Dykxhoorn7, Dan Peer1,2 1Laboratory of NanoMedicine, Department of Cell Research and Immunology, George S. Wise Faculty of Life Sciences, 2Department of Materials Sciences and Engineering, Faculty of Engineering, 3Center for Nanoscience and Nanotechnology, and z School of Chemistry, Tel- Aviv University, Tel Aviv, Israel, 4Department of NanoMedicine, Houston Methodist Research Institute, Houston, Texas, United States, 5Alnylam Pharmaceuticals, Cambridge,Massachusetts, United States, 6Department of Biochemistry & Molecular Biology, Life Science Centre, University of British Columbia, Vancouver, Canada, 7Dr. -

Pharmaceuticsand
2nd Edition of Global Conference on Pharmaceutics and Drug Delivery Systems June 04-06, 2018 | Rome, Italy PDDS 2018 The multifaceted aspects of drug delivery VENUE Holiday Inn Rome Aurelia Via Aurelia, Km 8.400, 00165 Rome, Italy https://pharmaceuticsconference.com Presenters PDDS 2018 Ana Carolina Kogawa Ali Dehshahri Anayanti Arianto Attila Gacsi Biana Godin Universidade Estadual Paulista Shiraz University of Medical University of Sumatera Utara University of Szeged Houston Methodist Research – UNESP, Brazil Sciences Indonesia Hungary Institute, USA Iran Chaodong Wu Csaba Hetenyi Daniel Zucker El Hassane Larhrib Elaine Frances Enright Texas A&M University University of Pecs NOF Europe GmbH University of Huddersfield University College Cork USA Hungary Germany UK Ireland Enise Ece Gurdal Esmaiel Jabbari Eugenia V. Gurevich Faiza Naseer Georgina Kate Such Yeditepe University University of South Carolina Vanderbilt University University of Huddersfield University of Melbourne Turkey USA USA UK Australia Gerald H Tomkin Gerhard Winter Gillian Hutcheon Guo-Ping Zhou Hadrien Calmet Beacon Hospital and Trinity LMU Munchen Liverpool John Moores Guangxi Academy of Sciences Barcelona Supercomputing College Dublin, Ireland Germany University, UK China Center (BSC-CNS), Spain Hakim Bangun Hassan Saeiahan Hemant K. S. Yadav Hyung Jun Ahn Ilya Yakavets University of Sumatera Utara Iran University of Medical RAK Medical & Health Science Korea Institute of Sceince and Universite de Lorraine Indonesia science, Iran University, UAE Technology, Republic -
Technion Israel Institute of Technology
Technion Israel Institute of Technology The Technion In operation since 1924, the Technion is the oldest university in Israel. Since its founding, the institute has educated three generations of men and women who have played a key role in laying the country’s infrastructure and establishing its crucial defense and high-tech industries. In the new millennium, Technion’s role at the forefront of the global network of science and technology has never been more vital. The university offers degrees in science and engineering, and related fields such as architecture, medicine, industrial management and education in an intellectually invigorating environment. Great emphasis is also placed on its humanities and social science programs, the incorporation of which take on ever-increasing importance in today’s multi-faceted workplace. But Technion’s goals go beyond providing a well- rounded technical education. At the institute, scientific instruction is interwoven with professional ethics, producing leaders sensitive to social and environmental issues. The dissemination of knowledge doesn’t end in the classroom. The Technion actively publishes its discoveries in journals and popular manuscripts, and aims to spark scientific and technological interest among youth through popular lectures and programs. Technion laboratories are also dedicated to enhancing the country’s economy – they offer novel solutions, research facilities, and world-class expertise. As a whole, the Technion is committed to its role as the country’s top facility for science and technology, a role that is necessary for the future of Israel and to all of humanity. Faculties and Centers Lokey Center Biology Biomedical Engineering Biotechnology and Food Engineering Chemical Engineering The Lorry I. -
Israel Partnership for Research October 18 - 21, 2013
UNIVERSITY OF MICHIGAN – ISRAEL PARTNERSHIP FOR RESEARCH OCTOBER 18 - 21, 2013 An International Scientific Symposium focused on the latest advances in Cardiovascular, Cancer and Neurobiology Research Symposium and associated grants have been generously supported by: D. Dan & Betty Kahn Foundation | Meredith and David Kaplan A. Alfred Taubman Medical Research Institute and other generous supporters of the U-M – Israel Partnership for Research TABLE OF CONTENTS SYMPOSIUM AGENDA 1-5 ABSTRACTS (IN ORDER OF PRESENTATION) SUNDAY Ami Aronheim 8 Omer Berenfeld 9 Peleg Hasson & Santhi Ganesh 10 Marcelle Machluf & Jérôme Kalifa 11 Ofer Binah & Daniel Michele 12 Doron Aronson 13 Oren Schuldiner 15 Izhak Kehat 16 Shelly Tzlil 17 Orit Kollet 18 Zaid Abbasi 19 Yuval Shaked 20 Eran Elinav 21 Ronen Rubinshtein 22 Orly Reiner 23 Ofer Fainaru 24 MONDAY Adam Stein 26 Henry Paulson 27 Mordechai Choder 28 Michal Schwartz 29 José Jalife 30 Gad Rennert 31 Theodore Lawrence 32 Eran Hornstein 33 Ivan Maillard 34 Ariel Roguin 35 Zvulun Elazar 36 Michael Aviram 37 Eva Feldman 38 Zvi Livneh 39 David Pinsky 40 Amir Landesberg 41 Berta Strulovici 43 CONTACT INFORMATION University of Michigan 46 Technion Institute of Technology 48 Weizmann Institute of Science 51 EXTRA PAGES FOR NOTE TAKING 54-58 SYMPOSIUM AGENDA SUNDAY, OCTOBER 20, 2013 SAMUEL AND JEAN FRANKEL CARDIOVASCULAR CENTER MARVIN AND BETTY DANTO AUDITORIUM 8:00-8:30 am CONTINENTAL BREAKFAST 8:30-8:40 am WELCOME & OPENING REMARKS David Pinsky (UM) MODERATORS: Donna Martin (UM) / Hector Valdivia (UM) 8:42-9:52 -
The 9Th Biennial Meeting of the Israeli Chapter of the Controlled Release Society New Trends and Technologies in Drug Delivery
THE 9TH BIENNIAL MEETING OF THE ISRAELI CHAPTER OF THE CONTROLLED RELEASE SOCIETY NEW TRENDS AND TECHNOLOGIES IN DRUG DELIVERY AND IN CONTROLLED-RELEASE BASED CONSUMER PRODUCTS September 9-11, 2014 Hacienda Forestview Hotel, Maalot, Israel 1 ORGANIZING COMMITTEE Prof. Ronit Satchi-Fainaro, Tel-Aviv University - ICRS President Dr. Ayelet David, Ben-Gurion University of the Negev Prof. Boaz Tirosh, The Hebrew University of Jerusalem Prof. Avi Domb, The Hebrew University of Jerusalem Prof. Smadar Cohen, Ben-Gurion University of the Negev Prof. Chezy Barenholtz, The Hebrew University of Jerusalem Dr. Avi Schroeder, Technion – Israel Institute of Technology Prof. Rimona Margalit, Tel-Aviv University Prof. Dan Peer, Tel-Aviv University Prof. Shulamit Levenberg, Technion – Israel Institute of Technology Prof. Rosa Azhari, Ort Braude Prof. Marcelle Machluf, Technion – Israel Institute of Technology Dr. Raphael Nudelman, Teva Pharmaceutical Industries Dr. Anat Eldar-Boock, Tel-Aviv University Dr. Dikla Ben-Shushan, Tel-Aviv University 2 SPONSORS 3 PROGRAM Tuesday –September 9, 2014 From 8:00 BUS TRANSPORTATION FROM the Technion, Tel Aviv University, Hebrew University of Jerusalem- Hadassah Ein Karem, Ben-Gurion University of the Negev 12:30 - 14:00 REGISTRATION AND POSTERS SETUP 13:00 LUNCH 14:00 - 14:15 WELCOME AND INTRODUCTORY REMARKS Ronit Satchi-Fainaro, ICRS President 14:15 – 16:20 SESSION 1 NANOMEDICINES IN CANCER TREATMENT Chairpersons: Ehud Gazit and Ronit Satchi-Fainaro 14:15 – 15:00 KEYNOTE PRESENTATION Prof. Henry Brem (Johns Hopkins -

The 9Th Biennial Meeting of the Israeli Chapter of the Controlled Release Society
THE 9TH BIENNIAL MEETING OF THE ISRAELI CHAPTER OF THE CONTROLLED RELEASE SOCIETY NEW TRENDS AND TECHNOLOGIES IN DRUG DELIVERY AND IN CONTROLLED-RELEASE BASED CONSUMER PRODUCTS September 9-11, 2014 Hacienda Forestview Hotel, Maalot, Israel 1 ORGANIZING COMMITTEE Prof. Ronit Satchi-Fainaro, Tel-Aviv University - ICRS President Dr. Ayelet David, Ben-Gurion University of the Negev Prof. Boaz Tirosh, The Hebrew University of Jerusalem Prof. Avi Domb, The Hebrew University of Jerusalem Prof. Smadar Cohen, Ben-Gurion University of the Negev Prof. Chezy Barenholtz, The Hebrew University of Jerusalem Dr. Avi Schroeder, Technion – Israel Institute of Technology Prof. Rimona Margalit, Tel-Aviv University Prof. Dan Peer, Tel-Aviv University Prof. Shulamit Levenberg, Technion – Israel Institute of Technology Prof. Rosa Azhari, Ort Braude Prof. Marcelle Machluf, Technion – Israel Institute of Technology Dr. Raphael Nudelman, Teva Pharmaceutical Industries Dr. Anat Eldar-Boock, Tel-Aviv University Dr. Dikla Ben-Shushan, Tel-Aviv University 2 SPONSORS 3 PROGRAM Tuesday –September 9, 2014 From 8:00 BUS TRANSPORTATION FROM the Technion, Tel Aviv University, Hebrew University of Jerusalem- Hadassah Ein Karem, Ben-Gurion University of the Negev 12:30 - 14:00 REGISTRATION AND POSTERS SETUP 13:00 LUNCH 14:00 - 14:15 WELCOME AND INTRODUCTORY REMARKS Ronit Satchi-Fainaro, ICRS President 14:15 – 16:20 SESSION 1 NANOMEDICINES IN CANCER TREATMENT Chairpersons: Ehud Gazit and Ronit Satchi-Fainaro 14:15 – 15:00 KEYNOTE PRESENTATION Prof. Henry Brem (Johns Hopkins -
INDUSTRY GUIDE to the TECHNION Research Projects Research Services Technology Transfer Cover: Acquired Using High Resolution Scanning Electron Microscopy
INDUSTRY GUIDE TO THE TECHNION Research Projects Research Services Technology Transfer Cover: Acquired using high resolution scanning electron microscopy Maria Koifman Khristosov, Prof. Boaz Pokroy Group Faculty of Materials Science and Engineering INDUSTRY GUIDE TO THE TECHNION Research Projects Research Services Technology Transfer Produced by The Technion Research and Development Foundation (TRDF). © 2017 Technion - Israel Institute of Technology, all rights reserved. Second edition. No reproduction, copy or transmissions of this publication may be made without written permission of the Technion - Israel Institute of Technology. Industry Guide to the Technion Contents 6 FROM THE PRESIDENT 61 Thermal and Energy Laboratory 8 ABOUT THE TECHNION 61 Radiation Safety in Construction Laboratory 12 Research Cooperation with Industry 62 Seskin Virtual Construction Laboratory 13 Research Promotion Unit 64 Norman and Helen Asher Space Research Institute (ASRI) 15 Industrial Affiliates Programs 65 Distributed Space Systems Laboratory (DSSL) 16 Research Equipment and Infrastructure 65 Electric Propulsion Laboratory 19 Research Contracts 65 Space Interferometry Laboratory 23 Technology Transfer 66 Aerospace Plasma Laboratory 24 Technion Technology Transfer (T3) 66 SAMSON Project 29 Alfred Mann Institute at the Technion (AMIT) 69 Solid State Institute (SSI) 30 Technion Drive Accelerator 70 Ion Implantation Laboratory 31 BioRap Technologies Ltd. 70 Near Field Optical Scanning and Raman Microscopy Laboratory 71 Variable Temperature, Ultra-High Vacuum, Scanning Probe 33 INTERDISCIPLINARY RESEARCH PROGRAMS Microscope (VT-UHVSPM) Laboratory 34 Technion Cyber Security Research Center 72 Surface Science Laboratory 36 Nancy and Stephen Grand Technion Energy Program (GTEP) 75 Stephen and Nancy Grand Water Research Institute (GWRI) 38 Technion Photovoltaic Laboratory 79 Transportation Research Institute (TRI) 38 Technion Hydrogen Technologies Research Laboratory (HTR) 80 Mobility Management Research Center 39 Leona M. -

Annual Report GERMANY the NETHERLANDS BERLIN Mr
FRIENDS OF THE ISRAEL CANCER ASSOCIATION Annual Report GERMANY THE NETHERLANDS BERLIN Mr. Robert Drake Mr. Michael Zehden Friends of the Israel Cancer Association In Holland Mrs. Julia Sengewitz Stichting B.K.I. Deutsch Israelische Hilfe für Krebskranke Kinder e.V Register Amsterdam Nr. 204207 Tauentzienstraße 7a Vijverweg 11 2015 D - 10789 Berlin NL - 2243 HR Wassenaar Germany The Netherlands Tel.: +49-30-521.325.452. Tel.: +31-70-511.37.45. Fax: +49-30-521.325.451. Mobile: +31-6-53.20.44.18. E-Mail: [email protected] E-Mail: [email protected] FRANKFURT UNITED KINGDOM Mrs. Orna Knoch Mrs. Vered Aaron Frankfurter Gesellschaft der Freunde und Förderer der Friends of the Israel Cancer Association Annual Report 2015 Krebsbekämpfung in Israel e.V Registered Charity No. 260710 Kaiserstraße 56 c/o Berwin Leighton Paisner LLP D - 60329 Frankfurt Adelaide House Germany London Bridge Tel.: +49-69-23.09.38. London EC4R 9HA Mobile: +49-177-589.36.16. United Kingdom E-Mail: [email protected] Tel: +44-793-263.11.28. Website: http://www.israelkrebshilfe.de/ E-Mail: [email protected] Honorary Treasurer - Mr. Martin Paisner MUNICH E-Mail: [email protected] Mrs. Anita Kaminski Gesellschaft zur Förderung der Krebshilfe in Israel, UNITED STATES OF AMERICA Komitee für Bayern, Munich Ms. Jill Cooper Böcklin Straße 12 Israel Cancer Association USA D - 80636 Munich 2751 S. Dixie Highway, Suite 3A Germany West Palm Beach Tel.: +49-89-15.30.39. 33405 Florida Mobile: +49-179-524.92.10. United States of America E-Mail: [email protected] Tel.: +1-561-832.92.77. -

Therapeutic Ultrasound Facilitates Antiangiogenic Gene Delivery and Inhibits Prostate Tumor Growth
2371 Therapeutic ultrasound facilitates antiangiogenic gene delivery and inhibits prostate tumor growth Maayan Duvshani-Eshet, Ofra Benny, to tumors in general, and to deliver angiogenic inhibitors Avigail Morgenstern, and Marcelle Machluf to prostate cancer in particular. [Mol Cancer Ther 2007;6(8):2371–82] The Faculty of Biotechnology and Food Engineering, Technion-Israel Institute of Technology, Haifa, Israel Introduction Abstract Antiangiogenic gene therapy is a promising approach to Gene therapy clinical trials are limited due to several inhibit neovascularization via angiogenesis, the growth of hurdles concerning the type of vector used, particularly, new blood vessels from preexisting ones. Gene therapy the viral vectors, and transfection efficacy when non– vectors can localize the DNA at the site of interest, lead- viral vectors are used. Therapeutic ultrasound is a ing to the expression of the angiogenic inhibitor (1). Such promising non–viral technology that can be used in the an approach can overcome drawbacks associated with clinical setting. Here, for the first time, we show the effi- stability, quantity, and long-term administration, which cacy of therapeutic ultrasound to deliver genes encoding involve antiangiogenic protein regiments. Nevertheless, for hemopexin-like domain fragment (PEX), an inhibitor of clinical applications of gene therapy, in general, are still in angiogenesis, to prostate tumors in vivo. Moreover, the the beginning stages due to several hurdles concerning addition of an ultrasound contrast agent (Optison) to the transfection efficiency and the type of vectors used, par- transfection process was evaluated. Prostate cancer cells ticularly the viral ones, which are subject to safety issues and endothelial cells (EC) were transfected in vitro with (2, 3). -

Waterproof Sunscreen
TECHNION Israel Institute of Technology Number 2, 2016 www.focus.technion.ac.il WATERPROOF SUNSCREEN Marine and freshwater cyanobacteria protect their photosynthesis Marine and freshwater cyanobacteria protect themselves from system from overexposure over-excitation in strong light by activating the Orange Carotenoid Protein (OCP). The picture depicts three bacteria, one in full sunlight (top, reddish), one in shade (bottom, orange hue) and one in the middle. (Image courtesy of Itay Goldshmid, Macromolecular Research Laboratory). While we are all familiar with The defense mechanism was deciphered Prof. Marcelle Machluf’s trailblazing work into a novel drug delivery system is showcased at Ben Gurion photosynthesis from the plant world, not in cyanobacteria (once known as “blue- NANO GHOST International Airport. everyone knows that it is also essential green algae”). The main player in this for all living things in the animal kingdom. mechanism is Orange Carotenoid Protein See story on page 3 Even those organisms that do not (OCP). OCP modifies its structure and color BUSTERS photosynthesize, do consume its primary in response to intense light, blocking the Special delivery to product: glucose. flow of energy that reaches the center of combat cancer the photosynthetic reaction. Due to the importance of this process, The ultimate goal in cancer therapy is a organisms have developed mechanisms “In this study we discovered how the OCP “magic bullet” that provides a versatile that protect them from overexposure to blocks the energy,” explains Adir, who is the delivery platform for site-specific targeting sunlight. Just as photographic film can be current dean. “In effect, the protein acts as of multiple compartments of the cancer overexposed, natural photosynthetic systems a biological switch.