Breaking Boundaries in Lung Cancer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pdf Liste Totale Des Chansons
40ú Comórtas Amhrán Eoraifíse 1995 Finale - Le samedi 13 mai 1995 à Dublin - Présenté par : Mary Kennedy Sama (Seule) 1 - Pologne par Justyna Steczkowska 15 points / 18e Auteur : Wojciech Waglewski / Compositeurs : Mateusz Pospiezalski, Wojciech Waglewski Dreamin' (Révant) 2 - Irlande par Eddie Friel 44 points / 14e Auteurs/Compositeurs : Richard Abott, Barry Woods Verliebt in dich (Amoureux de toi) 3 - Allemagne par Stone Und Stone 1 point / 23e Auteur/Compositeur : Cheyenne Stone Dvadeset i prvi vijek (Vingt-et-unième siècle) 4 - Bosnie-Herzégovine par Tavorin Popovic 14 points / 19e Auteurs/Compositeurs : Zlatan Fazlić, Sinan Alimanović Nocturne 5 - Norvège par Secret Garden 148 points / 1er Auteur : Petter Skavlan / Compositeur : Rolf Løvland Колыбельная для вулкана - Kolybelnaya dlya vulkana - (Berceuse pour un volcan) 6 - Russie par Philipp Kirkorov 17 points / 17e Auteur : Igor Bershadsky / Compositeur : Ilya Reznyk Núna (Maintenant) 7 - Islande par Bo Halldarsson 31 points / 15e Auteur : Jón Örn Marinósson / Compositeurs : Ed Welch, Björgvin Halldarsson Die welt dreht sich verkehrt (Le monde tourne sens dessus dessous) 8 - Autriche par Stella Jones 67 points / 13e Auteur/Compositeur : Micha Krausz Vuelve conmigo (Reviens vers moi) 9 - Espagne par Anabel Conde 119 points / 2e Auteur/Compositeur : José Maria Purón Sev ! (Aime !) 10 - Turquie par Arzu Ece 21 points / 16e Auteur : Zenep Talu Kursuncu / Compositeur : Melih Kibar Nostalgija (Nostalgie) 11 - Croatie par Magazin & Lidija Horvat 91 points / 6e Auteur : Vjekoslava Huljić -

Cabrillo Festival of Contemporarymusic of Contemporarymusic Marin Alsop Music Director |Conductor Marin Alsop Music Director |Conductor 2015
CABRILLO FESTIVAL OFOF CONTEMPORARYCONTEMPORARY MUSICMUSIC 2015 MARINMARIN ALSOPALSOP MUSICMUSIC DIRECTOR DIRECTOR | | CONDUCTOR CONDUCTOR SANTA CRUZ CIVIC AUDITORIUM CRUZ CIVIC AUDITORIUM SANTA BAUTISTA MISSION SAN JUAN PROGRAM GUIDE art for all OPEN<STUDIOS ART TOUR 2015 “when i came i didn’t even feel like i was capable of learning. i have learned so much here at HGP about farming and our food systems and about living a productive life.” First 3 Weekends – Mary Cherry, PrograM graduate in October Chances are you have heard our name, but what exactly is the Homeless Garden Project? on our natural Bridges organic 300 Artists farm, we provide job training, transitional employment and support services to people who are homeless. we invite you to stop by and see our beautiful farm. You can Good Times pick up some tools and garden along with us on volunteer + September 30th Issue days or come pick and buy delicious, organically grown vegetables, fruits, herbs and flowers. = FREE Artist Guide Good for the community. Good for you. share the love. homelessgardenproject.org | 831-426-3609 Visit our Downtown Gift store! artscouncilsc.org unique, Local, organic and Handmade Gifts 831.475.9600 oPen: fridays & saturdays 12-7pm, sundays 12-6 pm Cooper House Breezeway ft 110 Cooper/Pacific Ave, ste 100G AC_CF_2015_FP_ad_4C_v2.indd 1 6/26/15 2:11 PM CABRILLO FESTIVAL OF CONTEMPORARY MUSIC SANTA CRUZ, CA AUGUST 2-16, 2015 PROGRAM BOOK C ONTENT S For information contact: www.cabrillomusic.org 3 Calendar of Events 831.426.6966 Cabrillo Festival of Contemporary -

Good Short Total Song 1 64 0 64 R2 JINGLE
Index Good Short Total Song 1 64 0 64 R2 JINGLE - NOCNI 03 2 63 0 63 R2 JINGLE - NOCNI 04 3 59 0 59 R2 JINGLE - NOCNI 02 4 57 0 57 R2 JINGLE - NOCNI 05 5 56 0 56 R2 JINGLE - NOCNI 06 6 52 0 52 SHAWN MENDES, CAMILA CABELLO - SENORITA 7 51 0 51 PINK - WALK ME HOME 8 51 0 51 LAMAI - SPET TE SLISIM 9 51 0 51 ENRIQUE IGLESIAS FT. BAD BUNNY - EL BANO 10 50 0 50 PEDRO CAPO & FARRUKO - CALMA [REMIX] 11 50 0 50 IMAGINE DRAGONS - BAD LIAR 12 50 0 50 ALVARO SOLER - LA CINTURA 13 50 0 50 ED SHEERAN - PERFECT 14 50 0 50 AVA MAX - SO AM I 15 49 0 49 ARIANA GRANDE - NO TEARS LEFT TO CRY 16 49 0 49 LEWIS CAPALDI - SOMEONE YOU LOVED 17 49 0 49 AVA MAX - KINGS & QUEENS 18 48 0 48 LEWIS CAPALDI - BEFORE YOU GO 19 48 0 48 MAROON 5 - GIRLS LIKE YOU [DH CUT] 20 47 0 47 MAROON 5 - MEMORIES 21 46 0 46 LADY GAGA & BRADLEY COOPER - SHALLOW 22 46 0 46 GEORGE EZRA - SHOTGUN 23 45 0 45 THE WEEKND - BLINDING LIGHTS 24 45 0 45 PINK - A MILLION DREAMS 25 45 0 45 TOM WALKER - LEAVE A LIGHT ON 26 44 0 44 ED SHEERAN, JUSTIN BIEBER - I DON T CARE 27 43 0 43 AVA MAX - SALT 28 43 0 43 YOUNOTUS, JANIECK & SENEX - NARCOTIC 29 42 0 42 NINA PUSLAR - SVET NA DLANI 30 41 0 41 LUIS FONSI FT. -

Redox DAS Artist List for Period: 01.12.2020
Page: Redox D.A.S. Artist List for01.12.2020 period: - 31.12.2020 Date time: Title: Artist: min:sec 01.12.2020 00:06:24 HAVE A HOLLY JOLLY CHRISTMAS JOHNNY MATHIS 00:01:57 01.12.2020 00:08:31 BURNING UP MADONNA 00:03:39 01.12.2020 00:12:10 ZLOMLJENO SRCE PIKA BOŽIČ KONTREC 00:03:43 01.12.2020 00:16:13 DON T PAY THE FERRYMAN CHRIS DE BURGH 00:03:24 01.12.2020 00:19:35 NELL ARIA MARCELLA BELLA 00:03:48 01.12.2020 00:23:25 POVEJ NAGLAS ANDREJ IKICA 00:03:13 01.12.2020 00:26:45 LOVE ASHLEE SIMPSON 00:02:31 01.12.2020 00:29:17 SWEET CAROLINA NEIL DIAMOND 00:03:19 01.12.2020 00:32:34 AMAZONKA SAŠKA SMODEJ 00:03:03 01.12.2020 00:35:37 POP N SYNC 00:02:54 01.12.2020 00:38:37 PUTTING ON THE RITZ TACO 00:03:18 01.12.2020 00:41:55 PLOVEMO TRETJI KANU 00:04:30 01.12.2020 00:46:23 TOUCH LITTLE MIX 00:03:28 01.12.2020 00:49:57 EXTENDED DREAM SPAGNA 00:05:44 01.12.2020 00:55:40 THAT S THE TRUTH MCFLY 00:03:48 01.12.2020 00:59:28 MOMENTS IN LOVE BO ANDERSEN AND BERNIE PAUL00:04:27 01.12.2020 01:04:16 NAPOVEDNIK krajše 7 NOČ 00:02:29 01.12.2020 01:04:24 1 DEL 7 NOČ 00:00:43 01.12.2020 01:04:59 OBLADI OBLADA ORG MARMALADE 00:02:59 01.12.2020 01:07:54 VMESNI 2 7 NOČ 00:00:44 01.12.2020 01:07:59 ANOTHER SATURDAY NIGHT SAM COOKE 00:02:38 01.12.2020 01:10:36 PRIDI DALA TI BOM CVET EVA SRŠEN 00:02:50 01.12.2020 01:13:27 VMESNI 2 7 NOČ 00:00:44 01.12.2020 01:13:31 THAT S AMORE DEAN MARTIN FEAT FRANK SINATRA00:03:06 01.12.2020 01:16:38 2 DEL 7 NOČ 00:00:49 01.12.2020 01:17:27 MY WAY FRANK SINATRA 00:04:35 01.12.2020 01:21:55 VMESNI 2 7 NOČ 00:00:44 01.12.2020 -
LOOK! Secretary
VOLUME XII. NEWTOWN, FRIDAY, SEPTEMBER 6, 1889. SIX PAGES. NUMBER 36. Old age and infirmity have made Jane Cards Are out for the marriage of Kl- - Brush so feeble that it was deemed nec- mer' B. Hawley, formerly of Hawley-vill- e, C. LYON & HINDLEY. essary, to appoint a conservator, and to Miss Cornelia Belle Estey of H. B E N N E T T. Charles II. Peck was chosen, tn He Chicago, September 17. July. ... has applied to the probate court for per mission to sell her real estate and the Town election Octo AT THE SEASON occurs, this year, OUR SALES THUS FAR FOR THIS IN auction will bike She ber 7. The selectmen of Newtown will -- place, Saturday. 3HE 3L hus only the house in which she lives and meet at the town clerk's ofllce.Saturday, a,... that is worth, probably,-no- t more than September 28, from 9am until 5pm9 e IsSOO, w Fairchild of South Britain for new J. R MENABY CO'S. SCHOOL SHOES r r George the purpose of making voters. CHILDREN'S BUILDERS, MANUFACTURERS, FARMERS holds a mortgage for $600, and she owes No person can be made a voter whose other small bills, aggregating, possibly, name Is not on the list to be made,Thurs-day- 1, $50. The mortgage to Mr Fairchild was September 19, at 3 p m. Those de- an immense stock of AND MECHANICS - Have been large but we are prepared with vv:: made at different times, $300 each,- to siring to be made voters, this Fall, should these goods in an almost endless assortment of styles and at very cover money advanced by him in small hand their name to any of the registrars sums. -

Europack 2004
www.eurovision-spain.com XLIX Festival de eurovisión Estambul – Turquía – 12 y 15 de mayo de 2003 Europack 2004 SEMIFINAL visítanos en www.eurovision-spain.com europack 2003 | pág 1 www.eurovision-spain.com XLIX Festival de eurovisión Estambul – Turquía – 12 y 15 de mayo de 2003 Estimados visitantes y amigos de www.eurovision-spain.com ya tenemos aquí un nuevo festival de eurovisión, en esta ocasión con dos galas, la final y la semifinal , hemos llegado al fin del camino que comenzamos hace casi un año siguiendo todo el proceso de organización del festival, casi 365 intentando ofreceros la mejor información y servicios, porque eurovisión se vive más que un día al año. Como hicimos el año pasado aquí teneis nuestro europack, pero en esta ocasión dividido en dos partes para sigáis el festival con toda la información que necesitéis en cada momento, lista de países, canciones, letras en versión original y traducción al castellano y tablero de puntuaciones total, todo ello para que tan sólo tengas que imprimirlo y empezar a vivir el festival desde ahora. El Europack de la final será publicado una vez se conozcan los finalistas Gracias a todos por vuestro apoyo durante esta temporada eurovisiva y esperamos contar con todos en la nueva que hoy comienza para el festival de la canción de eurovisión. Saludos a todos y gracias en nombre de todos los que hacemos www.eurovisión-spain.com europack 2003 | pág 2 www.eurovision-spain.com XLIX Festival de eurovisión Estambul – Turquía – 12 y 15 de mayo de 2003 Lista de participantes: XLIX Festival de Eurovisión final: 15/05/04 | semifinal: 12/05/04 Sede: Estambul, Turquía - Abdi Ipekci Votación: de 1 a 8, 10 y 12 - (votos alfabéticamente 36-final y 33-semi) Participantes: 14 finalistas + 10 semifinalistas Semifinal nº País Intérprete - canción pts. -

Attractive Rumson
SECTION ONE EGIST SECTION ONE VOLUME LXV, NO. 22. HEETBAMK, N. J.; THURSD5Y7TTOVEMBER 19, 1942. PAGES 1 TO 14 Attractive Rumson Holiday Issue ' Start Second Drive For Recruits Needed Headlights Must Be Next Wednesday For The WAAGS Women, you want to do your - The Bed Bank Register next Payroll AllotfneniiElarL 'paftrHore li~yaui'"opportunity!— DitnmedGutTotkorraw week will appear Wednesday . .Enlist In. the Women's, Army, Instead of Thursday, this being Auxiliary Corps and releaso ' duo to Thanksgiving falling on able-bodied'men for active com- . publication day, * . ,. Campaign Opens Today To Sign bat duty. There are unexcelled Walter L. Tepper Buy* In order that our advertisers opportunities for women be-1 New Regulations Prohibit Use will get tbe full pulling power twecn tho ages of 21 and 45 for of The Register's large circuln- Up The Remaining 10 Percent advancement in tho corps as Of Upper Beam At Any Time Large Shore Front Estate latlon for that Issue, we will ad- well as training and prepara-: vance our publication day to F -*• tlon for the future. The rate of Headlights on all automobiles Walter I. Topper of Humson has •^Wednesday, as stated "above. In Accordance with national' plans; pay 13 the same ks the. pay for purchased from the Metropolitan In- . We respectfully solicit tho ;he Monmouth County War Savings 1 >pcratcd at night in Monmouth) Ten Of Jacobs the corresponding rank In the Organ Recital :ounty, excepting Upper Freehold, surance company, the former Haley Hermine Hudon To further co-operation of our cor- itaff and its sub-committee, the Mon- Army. -

Redox DAS Artist List for Period: 01.06.2021
Page: Redox D.A.S. Artist List for01.06.2021 period: - 30.06.2021 Date time: Title: Artist: min:sec 01.06.2021 00:03:46 MELODY D AMOURE FACTS AND FICTION 00:03:41 01.06.2021 00:07:27 I CAN T HELP MYSELF BONNIE POINTER 00:05:20 01.06.2021 00:12:47 IT S COMPLICATED MARAAYA FEAT BQL 00:03:39 01.06.2021 00:16:33 PAME PAME EVANGELIA 00:02:14 01.06.2021 00:18:48 MILLE BRACCIA LAURA PAUSINI 00:03:23 01.06.2021 00:22:11 STOPAJ Z MANO V KORAK UROŠ ZAGOŽEN 00:03:38 01.06.2021 00:26:01 ABSOLUTELY EVERYBODY PEPPER 00:03:40 01.06.2021 00:29:42 BETTER LOVE DAPHNE 00:03:42 01.06.2021 00:33:43 LAST IN LINE NYLON BEAT 00:03:22 01.06.2021 00:37:05 I WANNA WAKE UP WITH YOU ERANN DD 00:03:27 01.06.2021 00:40:50 THE FIRST CRY THOMAS ANDERS 00:04:33 01.06.2021 00:45:24 MINE MINE MINE CHRISTOPHER 00:03:14 01.06.2021 00:48:34 2 HEARTS KYLIE MINOGUE 00:02:50 01.06.2021 00:51:32 TISOČ LET GOLDEN EYE 00:03:52 01.06.2021 00:55:24 SORRYS NOT GOOD ENOUGH MCFLY 00:04:23 01.06.2021 00:59:46 FEMME LIKE U K MARO 00:03:57 01.06.2021 01:04:38 I COME IN PEACE JOE COCKER 00:04:14 01.06.2021 01:08:54 PRIDI DALA TI BOM CVET EVA SRŠEN 00:02:50 01.06.2021 01:11:44 MY LITTLE BABY MIKE BERRY 00:01:53 01.06.2021 01:13:41 HYMN 4 MY SOUL JOE COCKER 00:03:42 01.06.2021 01:18:01 WHERE WOULD I BE NOW JOE COCKER 00:05:24 01.06.2021 01:26:21 THE THINGS WE DO FOR LOVE 10 CC 00:03:14 01.06.2021 01:29:36 IT S IN HIS KISS LINDA LEWIS 00:03:17 01.06.2021 01:32:57 DON T LET ME BE MISUNDERSTOODJOE COCKER 00:03:49 01.06.2021 01:37:36 LET THE HEALING BEGIN JOE COCKER 00:04:10 01.06.2021 01:41:51 -
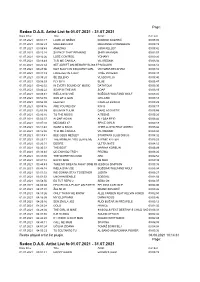
Redox DAS Artist List for Period: 01.07.2021
Page: Redox D.A.S. Artist List for01.07.2021 period: - 31.07.2021 Date time: Title: Artist: min:sec 01.07.2021 00:01:17 LJUBI JO NEŽNO DOMINIK KOZARIČ 00:05:05 01.07.2021 00:06:29 MARLEEN 2004 MARIANNE ROSENBERG 00:03:19 01.07.2021 00:09:48 AMAZING JOSH KELLEY 00:03:42 01.07.2021 00:13:28 SILENCE THAT REMAINS SHIRI MAYMON 00:02:57 01.07.2021 00:16:26 LOSE CONTROL YOHANY 00:03:20 01.07.2021 00:19:49 TI SI ME ČAKALA VILI RESNIK 00:03:04 01.07.2021 00:22:54 SET ADRIFT ON MEMORY BLISS MAXIP M DAWN 00:05:12 01.07.2021 00:28:06 NOT SUCH AN INNOCENT GIRL VICTORIA BECKHAM 00:03:16 01.07.2021 00:31:33 FOREVER IN A DAY TOŠE PROESKI 00:03:47 01.07.2021 00:35:20 ŠE ZELENO VLADO PILJA 00:03:40 01.07.2021 00:38:59 FLY BY II BLUE 00:03:47 01.07.2021 00:42:52 IN EVERY SOUND OF MUSIC DATAFOLK 00:03:30 01.07.2021 00:46:22 SOAP IN THE AIR SOAP 00:03:19 01.07.2021 00:49:41 IMELA SVA VSE BOŽIDAR WOLFAND WOLF 00:03:04 01.07.2021 00:52:50 SUN OF A GUN OH LAND 00:03:18 01.07.2021 00:56:09 HEAVEN CAMILLA BRINCK 00:03:29 01.07.2021 00:59:36 ARE YOU READY R N G 00:03:17 01.07.2021 02:53:35 BULIM IN TULIM DARE ACOUSTIC 00:03:55 01.07.2021 03:00:16 TO THE MUSIC A TEENS 00:03:20 01.07.2021 03:03:37 ALONE AGAIN ALYSSA REID 00:03:44 01.07.2021 03:07:30 MEGAMIX 07 SPICE GIRLS 00:04:18 01.07.2021 03:11:48 WANT U BACK CHER LLOYD FEAT ASTRO 00:03:42 01.07.2021 03:15:30 TI SI ME ČAKALA VILI RESNIK 00:03:04 01.07.2021 03:18:41 BEE GEES MEDLEY STARTRAX CLUB DISCO 00:04:32 01.07.2021 03:23:11 THE MOMENT YOU LEAVE ME ATOMIC KITTEN 00:03:23 01.07.2021 03:26:31 DESIRE ULTRA NATE -

13Th EBSA Congress, July 24-28, 2021, Vienna, Austria
European Biophysics Journal (2021) 50 (Suppl 1):S1–S226 https://doi.org/10.1007/s00249-021-01558-w 13th EBSA congress July 24–28, 2021, Vienna, Austria This supplement was not sponsored by outside commercial interests. It was funded entirely by the publisher. S2 European Biophysics Journal (2021) 50 (Suppl 1):S1–S226 Acknowledgements Silver sponsors: • Bruker Nano Surfaces Division • Beckman Coulter Bronze sponsors: • Boehringer Ingelheim • Elements Exhibitors: • Fida Biosystems • PicoQuant • Teledyne Photometrics • Olympus - Life Science Solutions • REDSHIFT Bio Other Sponsors: • Austrian Physical Society • Hamamatsu Photonics • Nanion Technologies • Lumicks • Springer Nature • Biophysical Society • MDPI / Biomolecules • Carl Zeiss DFG -- Deutsche Forschungsgemeinschaft • • MDPI / Membranes European Biophysics Journal (2021) 50 (Suppl 1):S1–S226 S3 13th EBSA European Biophysics Congress Vienna (Austria), July 24–28, 2021 Organized by Biophysics Austria CONFERENCE CHAIR Elena E. POHL Institute of Physiology, Pathophysiology and Biophysics, University of Veterinary Medicine Vienna Vice President of Biophysics Austria Vice President of EBSA LOCAL ORGANIZING & SCIENTIFIC COMMITTEE Klaus GROSCHNER, Institute of Biophysics, Medical University Graz Carl-Philipp HEISENBERG, Institute of Science and Technology Austria, Klosterneuburg Peter HINTERDORFER, Institute of Biophysics, Johannes Kepler University Linz Andreas HORNER, Institute of Biophysics, Johannes Kepler University Linz Thomas A. KLAR, Institute for Applied Physics, Johannes Kepler -

Promoting Nation Building and Nation Branding Through Western
Master Thesis Promoting Nation Building and Nation branding through Western European Integration in the Eurovision Song Contest Master Program: Politics and Economics of Contemporary Eastern and Southeastern Europe Thessaloniki, University of Macedonia Author: Theodoros Kitsios M1318 Supervisor: Dr. Fotini Tsimpiridou 0 Declaration in Lieu of Oath I hereby declare, under oath, that this master thesis has been my independent work and has not been aided with any prohibited means. I declare, to the best of my knowledge and belief, that all passages taken from published and unpublished sources or documents have been reproduced whether as original, slightly changed or in thought, have been mentioned as such at the corresponding places of the thesis, by citation, where the extent of the original quotes is indicated. The paper has not been submitted for evaluation to another examination authority or has been published in this form or another. Thessaloniki, 01.10.2013 Theodoros Kitsios 1 Acknowledgements I would like to thank Dr. Fotini Tsimpiridou who supervised, advised and supported me throughout the realization of this thesis. No matter which problems would have come up, she was always open and helpful in her counsel. I am really grateful to her, for giving me the chance to fulfill a dream of my early adolescence, to delve into the Eurovision Song Contest from the perspective I have been enraptured since 1990, when I watched the contest for the first time in my life from the couch of my parents’ house. From that time on, I knew there was something more in this show, than what the television programs suggested to be. -

01.06.2018 00:03:11 Hd 055332 Štajerc Zoran Predin
01.06.2018 00:03:11 HD 055332 ŠTAJERC ZORAN PREDIN HELIDON 00:03:13 SLO 01.06.2018 00:06:41 HD 010153 THUNDERSTRUCK BLIZZARD BROTHERS CENTRAL STATION00:03:51 ANG 01.06.2018 00:10:31 HD 032792 THE WINNER TAKES IT ALL ABBA UNIVERSAL MUSIC00:04:48 ANG 01.06.2018 00:15:15 HD 022742 KRALJICA NOČI RATTLE SNAKE 00:02:52 SLO 01.06.2018 00:18:15 HD 053137 MY LIFE BILLY JOEL COLUMBIA 00:03:47 ANG 01.06.2018 00:21:52 HD 022199 WISH YOU WERE HERE PINK FLOYD CBS MUSIC 00:04:58 ANG 01.06.2018 00:26:41 HD 004585 NAJBOLJŠI PAR PERO LOVŠIN HELIDON 00:03:38 SLO 01.06.2018 00:30:29 HD 038314 I STILL HAVEN'T FOUND WHAT I'M LOOKINGU2 & COCOFOR FREEMAN 00:04:46 ANG 01.06.2018 00:35:06 HD 007388 LIGHT MY FIRE WILL YOUNG BMG 00:03:19 ANG 01.06.2018 00:38:15 HD 024127 ZALJUBLJENA DITKA HABERL 00:03:19 SLO 01.06.2018 00:41:47 HD 032792 THE WINNER TAKES IT ALL ABBA UNIVERSAL MUSIC00:04:48 ANG 01.06.2018 00:46:31 HD 021544 DEVEDESETE ĐORĐE BALAŠEVIČ DALLAS 00:05:34 SRB 01.06.2018 00:51:56 HD 016792 GREH TABU 00:03:39 SLO 01.06.2018 00:55:59 HD 003275 FLY AWAY FROM HERE AEROSMITH COLUMBIA 00:04:20 ANG 01.06.2018 01:00:13 HD 005332 LJUBIL BI SE GU GU RTVS 00:04:33 SLO 01.06.2018 01:04:36 HD 033507 SI OK (DJT BY DNE RMX) JAN PLESTENJAK MENART 00:04:21 SLO 01.06.2018 01:09:05 HD 032699 NUMBA 1 (THE TIDE IS HIGH) KARDINAL OFFISHAL FEAT.