Nuclear Genetic Defects of Mitochondrial ATP Synthase
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Amplification of 8Q21 in Breast Cancer Is Independent of MYC and Associated with Poor Patient Outcome
Modern Pathology (2010) 23, 603–610 & 2010 USCAP, Inc. All rights reserved 0893-3952/10 $32.00 603 Amplification of 8q21 in breast cancer is independent of MYC and associated with poor patient outcome Matthias Choschzick1, Paula Lassen1, Annette Lebeau1, Andreas Holger Marx1, Luigi Terracciano2, Uwe Heilenko¨tter3, Fritz Jaenicke4, Carsten Bokemeyer5, Jakob Izbicki6, Guido Sauter1 and Ronald Simon1 1Institute of Pathology, University Medical Centre Hamburg-Eppendorf, Hamburg, Germany; 2Institute of Pathology, University Hospital Basel, Basel, Switzerland; 3Department of Gynaecology, Hospital Itzehoe, Itzehoe, Germany; 4Department of Gynaecology, University Medical Centre Hamburg-Eppendorf, Hamburg, Germany; 5Department of Oncology, Hematology, Bone Marrow Transplantation with Section Pneumology, University Hospital Hamburg-Eppendorf, Hamburg, Germany and 6Department of Surgery, University Medical Centre Hamburg-Eppendorf, Hamburg, Germany Copy number gains involving the long arm of chromosome 8, including high-level amplifications at 8q21 and 8q24, have been frequently reported in breast cancer. Although the role of the MYC gene as the driver of the 8q24 amplicon is well established, the significance of the 8q21 amplicon is less clear. The breast cancer cell line SK-BR-3 contains three separate 8q21 amplicons, the distal two of which correspond to putative target genes TPD52 and WWP1. To understand the effect of proximal 8q21 amplification on breast cancer phenotype and patient prognosis, we analyzed 8q21 copy number changes using fluorescence in situ hybridization (FISH) in a tissue microarray containing more than 2000 breast cancers. Amplification at 8q21 was found in 3% of tumors, and was associated with medullary type (Po0.03), high tumor grade (Po0.0001), high Ki67 labeling index (Po0.05), amplification of MYC (Po0.0001), HER2, MDM2, and CCND1 (Po0.05 each), as well as the total number of gene amplifications (Po0.0001). -

Human Diseases Associated with Defects in Assembly of OXPHOS Complexes
Essays in Biochemistry (2018) 62 271–286 https://doi.org/10.1042/EBC20170099 Review Article Human diseases associated with defects in assembly of OXPHOS complexes Daniele Ghezzi1,2 and Massimo Zeviani3 1Molecular Neurogenetics, Foundation IRCCS Neurological Institute Besta, Milan, Italy; 2Department of Pathophysiology and Transplantation, University of Milan, Milan, Italy; 3Medical Research Council – Mitochondrial Biology Unit, University of Cambridge, Cambridge, U.K. Correspondence: Massimo Zeviani ([email protected]) The structural biogenesis and functional proficiency of the multiheteromeric complexes forming the mitochondrial oxidative phosphorylation system (OXPHOS) require the con- certed action of a number of chaperones and other assembly factors, most of which are specific for each complex. Mutations in a large number of these assembly factors arere- sponsible for mitochondrial disorders, in most cases of infantile onset, typically character- ized by biochemical defects of single specific complexes. In fact, pathogenic mutations in complex-specific assembly factors outnumber, in many cases, the repertoire of mutations found in structural subunits of specific complexes. The identification of patients with spe- cific defects in assembly factors has provided an important contribution to the nosological characterization of mitochondrial disorders, and has also been a crucial means to identify a huge number of these proteins in humans, which play an essential role in mitochondrial bioenergetics. The wide use of next generation sequencing (NGS) has led to and will allow the identifcation of additional components of the assembly machinery of individual com- plexes, mutations of which are responsible for human disorders. The functional studies on patients’ specimens, together with the creation and characterization of in vivo models, are fundamental to better understand the mechanisms of each of them. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Multivariate Analysis Reveals Genetic Associations of the Resting Default
Multivariate analysis reveals genetic associations of PNAS PLUS the resting default mode network in psychotic bipolar disorder and schizophrenia Shashwath A. Medaa,1, Gualberto Ruañob,c, Andreas Windemuthb, Kasey O’Neila, Clifton Berwisea, Sabra M. Dunna, Leah E. Boccaccioa, Balaji Narayanana, Mohan Kocherlab, Emma Sprootena, Matcheri S. Keshavand, Carol A. Tammingae, John A. Sweeneye, Brett A. Clementzf, Vince D. Calhoung,h,i, and Godfrey D. Pearlsona,h,j aOlin Neuropsychiatry Research Center, Institute of Living at Hartford Hospital, Hartford, CT 06102; bGenomas Inc., Hartford, CT 06102; cGenetics Research Center, Hartford Hospital, Hartford, CT 06102; dDepartment of Psychiatry, Beth Israel Deaconess Hospital, Harvard Medical School, Boston, MA 02215; eDepartment of Psychiatry, University of Texas Southwestern Medical Center, Dallas, TX 75390; fDepartment of Psychology, University of Georgia, Athens, GA 30602; gThe Mind Research Network, Albuquerque, NM 87106; Departments of hPsychiatry and jNeurobiology, Yale University, New Haven, CT 06520; and iDepartment of Electrical and Computer Engineering, The University of New Mexico, Albuquerque, NM 87106 Edited by Robert Desimone, Massachusetts Institute of Technology, Cambridge, MA, and approved April 4, 2014 (received for review July 15, 2013) The brain’s default mode network (DMN) is highly heritable and is Although risk for psychotic illnesses is driven in small part by compromised in a variety of psychiatric disorders. However, ge- highly penetrant, often private mutations such as copy number netic control over the DMN in schizophrenia (SZ) and psychotic variants, substantial risk also is likely conferred by multiple genes bipolar disorder (PBP) is largely unknown. Study subjects (n = of small effect sizes interacting together (7). According to the 1,305) underwent a resting-state functional MRI scan and were “common disease common variant” (CDCV) model, one would analyzed by a two-stage approach. -

ATPAF2 CRISPR/Cas9 KO Plasmid (M): Sc-434234
SANTA CRUZ BIOTECHNOLOGY, INC. ATPAF2 CRISPR/Cas9 KO Plasmid (m): sc-434234 BACKGROUND APPLICATIONS The Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) and ATPAF2 CRISPR/Cas9 KO Plasmid (m) is recommended for the disruption of CRISPR-associated protein (Cas9) system is an adaptive immune response gene expression in mouse cells. defense mechanism used by archea and bacteria for the degradation of foreign genetic material (4,6). This mechanism can be repurposed for other 20 nt non-coding RNA sequence: guides Cas9 functions, including genomic engineering for mammalian systems, such as to a specific target location in the genomic DNA gene knockout (KO) (1,2,3,5). CRISPR/Cas9 KO Plasmid products enable the U6 promoter: drives gRNA scaffold: helps Cas9 identification and cleavage of specific genes by utilizing guide RNA (gRNA) expression of gRNA bind to target DNA sequences derived from the Genome-scale CRISPR Knock-Out (GeCKO) v2 library developed in the Zhang Laboratory at the Broad Institute (3,5). Termination signal Green Fluorescent Protein: to visually REFERENCES verify transfection CRISPR/Cas9 Knockout Plasmid CBh (chicken β-Actin 1. Cong, L., et al. 2013. Multiplex genome engineering using CRISPR/Cas hybrid) promoter: drives expression of Cas9 systems. Science. 339: 819-823. 2A peptide: allows production of both Cas9 and GFP from the 2. Mali, P., et al. 2013. RNA-guided human genome engineering via Cas9. same CBh promoter Science 339: 823-826. Nuclear localization signal 3. Ran, F.A., et al. 2013. Genome engineering using the CRISPR-Cas9 system. Nuclear localization signal SpCas9 ribonuclease Nat. Protoc. 8: 2281-2308. -

Mitochondrial Medicine in the Omics Era
Mitochondrial Medicine in the Omics Era Joyeeta Rahman1 and Shamima Rahman1,2* 1 Mitochondrial Research Group, UCL Great Ormond Street Institute of Child Health and 2 Metabolic Unit, Great Ormond Street Hospital NHS Foundation Trust, London, UK *Correspondence to: Professor Shamima Rahman Mitochondrial Research Group Genetics and Genomic Medicine UCL Great Ormond Street Institute of Child Health London WC1N 1EH, UK. Telephone: +44 (0)2079052608 [email protected] Keywords: Mitochondrial disease, OXPHOS, signalling, omics, genomics, transcriptomics, proteomics, metabolomics, mitochondrial stress response, treatment 1 Abstract Mitochondria are dynamic bioenergetic organelles whose maintenance requires ~1500 proteins from two genomes. Mutations in either the mitochondrial or nuclear genome can disrupt a plethora of cellular metabolic and homeostatic functions. Mitochondrial diseases represent one the most common and severe groups of inherited genetic disorders, characterised by clinical, biochemical, and genetic heterogeneity, diagnostic odysseys, and lack of curative therapies. This review aims to discuss recent advances in mitochondrial biology and medicine arising from widespread utilisation of high-throughput omics technologies, and also includes a broad discussion of emerging therapies for mitochondrial disease. New insights into both bioenergetic and biosynthetic mitochondrial functionalities have expedited the genetic diagnosis of primary mitochondrial disorders, and identified novel mitochondrial pathomechanisms and new targets -
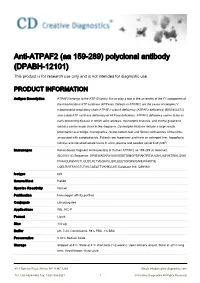
Anti-ATPAF2 (Aa 159-289) Polyclonal Antibody (DPABH-12101) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-ATPAF2 (aa 159-289) polyclonal antibody (DPABH-12101) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Antigen Description ATPAF2 belongs to the ATP12 family. It may play a role in the assembly of the F1 component of the mitochondrial ATP synthase (ATPase). Defects in ATPAF2 are the cause of complex V mitochondrial respiratory chain ATPAF2 subunit deficiency (ATPAF2 deficiency) [MIM:604273]; also called ATP synthase deficiency or ATPase deficiency. ATPAF2 deficiency seems to be an early presenting disease in which lactic acidosis, dysmorphic features, and methyl glutaconic aciduria can be major clues in the diagnosis. Dysmorphic features include a large mouth, prominent nasal bridge, micrognathia, rocker-bottom feet and flexion contractures of the limbs associated with camptodactyly. Patients are hypertonic and have an enlarged liver, hypoplastic kidneys and elevated lactate levels in urine, plasma and cerebro spinal fluid (CSF). Immunogen Recombinant fragment corresponding to Human ATPAF2 aa 159-289 (C terminal). (BC004114).Sequence: DPIIEWAEKRYGVEISSSTSIMGPSIPAKTREVLVSHLASYNTWALQGIE FVAAQLKSMVLTLGLIDLRLTVEQAVLLSRLEEEYQIQKWGNIEWAHDYE LQELRARTAAGTLFIHLCSESTTVKHKLLKE Database link: Q8N5M1 Isotype IgG Source/Host Rabbit Species Reactivity Human Purification Immunogen affinity purified Conjugate Unconjugated Applications WB, IHC-P Format Liquid Size 100 μg Buffer pH: 7.20; Constituents: 98% PBS, 1% BSA Preservative 0.02% Sodium Azide Storage Shipped at 4°C. Store at 4°C short term (1-2 -

Mitochondrial Dysfunction and Its Role in Tissue-Specific Cellular Stress
Review www.cell-stress.com Mitochondrial dysfunction and its role in tissue-specific cellular stress David Pacheu-Grau1,*, Robert Rucktäschel1 and Markus Deckers1,* 1 Department of Cellular Biochemistry, University Medical Center Göttingen, Germany. * Corresponding Authors: David Pacheu-Grau, University Medical Center Göttingen, Department of Cellular Biochemistry, Humboldtallee 23, 37073 Göttingen, Germany. Phone: +49-(0)551-394571; E-mail: [email protected]; Markus Deckers, University Medical Center Göttingen, Department of Cellular Biochemistry, Humboldtallee 23, 37073 Göttingen, Germany. Phone: +49-(0)551-395983; E-mail: [email protected] ABSTRACT Mitochondrial bioenergetics require the coordination of two dif- doi: 10.15698/cst2018.07.147 ferent and independent genomes. Mutations in either genome will affect mi- Received originally: 26.04.2018 tochondrial functionality and produce different sources of cellular stress. De- in revised form: 13.06.2018, Accepted 14.06.2018, pending on the kind of defect and stress, different tissues and organs will be Published 13.07.2018. affected, leading to diverse pathological conditions. There is no curative ther- apy for mitochondrial diseases, nevertheless, there are strategies described that fight the various stress forms caused by the malfunctioning organelles. Keywords: mitochondrial dysfunction, Here, we will revise the main kinds of stress generated by mutations in mito- cellular stress, mitochondrial chondrial genes and outline several ways of fighting this stress. pathology, therapy. Abbreviations: ADOA – autosomal dominant optic atrophy, AROA – autosomal recessive optic atrophy, ARS – aminoacyl-tRNA synthetase, CL – cardiolipin, CRISPR – clustered regularly interspaced short palindromic repeats, LHON – Leber’s hereditary optic neuropathy, mt - mitochondrial OXPHOS – oxidative phosphorylation, ROS – reactive oxygen species. -

Human Mitochondrial Pathologies of the Respiratory Chain and ATP Synthase: Contributions from Studies of Saccharomyces Cerevisiae
life Review Human Mitochondrial Pathologies of the Respiratory Chain and ATP Synthase: Contributions from Studies of Saccharomyces cerevisiae Leticia V. R. Franco 1,2,* , Luca Bremner 1 and Mario H. Barros 2 1 Department of Biological Sciences, Columbia University, New York, NY 10027, USA; [email protected] 2 Department of Microbiology,Institute of Biomedical Sciences, Universidade de Sao Paulo, Sao Paulo 05508-900, Brazil; [email protected] * Correspondence: [email protected] Received: 27 October 2020; Accepted: 19 November 2020; Published: 23 November 2020 Abstract: The ease with which the unicellular yeast Saccharomyces cerevisiae can be manipulated genetically and biochemically has established this organism as a good model for the study of human mitochondrial diseases. The combined use of biochemical and molecular genetic tools has been instrumental in elucidating the functions of numerous yeast nuclear gene products with human homologs that affect a large number of metabolic and biological processes, including those housed in mitochondria. These include structural and catalytic subunits of enzymes and protein factors that impinge on the biogenesis of the respiratory chain. This article will review what is currently known about the genetics and clinical phenotypes of mitochondrial diseases of the respiratory chain and ATP synthase, with special emphasis on the contribution of information gained from pet mutants with mutations in nuclear genes that impair mitochondrial respiration. Our intent is to provide the yeast mitochondrial specialist with basic knowledge of human mitochondrial pathologies and the human specialist with information on how genes that directly and indirectly affect respiration were identified and characterized in yeast. Keywords: mitochondrial diseases; respiratory chain; yeast; Saccharomyces cerevisiae; pet mutants 1. -

Characterizing Genomic Duplication in Autism Spectrum Disorder by Edward James Higginbotham a Thesis Submitted in Conformity
Characterizing Genomic Duplication in Autism Spectrum Disorder by Edward James Higginbotham A thesis submitted in conformity with the requirements for the degree of Master of Science Graduate Department of Molecular Genetics University of Toronto © Copyright by Edward James Higginbotham 2020 i Abstract Characterizing Genomic Duplication in Autism Spectrum Disorder Edward James Higginbotham Master of Science Graduate Department of Molecular Genetics University of Toronto 2020 Duplication, the gain of additional copies of genomic material relative to its ancestral diploid state is yet to achieve full appreciation for its role in human traits and disease. Challenges include accurately genotyping, annotating, and characterizing the properties of duplications, and resolving duplication mechanisms. Whole genome sequencing, in principle, should enable accurate detection of duplications in a single experiment. This thesis makes use of the technology to catalogue disease relevant duplications in the genomes of 2,739 individuals with Autism Spectrum Disorder (ASD) who enrolled in the Autism Speaks MSSNG Project. Fine-mapping the breakpoint junctions of 259 ASD-relevant duplications identified 34 (13.1%) variants with complex genomic structures as well as tandem (193/259, 74.5%) and NAHR- mediated (6/259, 2.3%) duplications. As whole genome sequencing-based studies expand in scale and reach, a continued focus on generating high-quality, standardized duplication data will be prerequisite to addressing their associated biological mechanisms. ii Acknowledgements I thank Dr. Stephen Scherer for his leadership par excellence, his generosity, and for giving me a chance. I am grateful for his investment and the opportunities afforded me, from which I have learned and benefited. I would next thank Drs. -

Mark Adam Scott Mitochondrial Survival Without Oxygen
Mark Adam Scott Mitochondrial survival without oxygen Faculty of Mathematics and Natural Sciences University of Oslo 2017 Mitochondrial survival without oxygen By Mark Adam Scott Thesis presented for the degree of PHILOSOPHIAE DOCTOR Department of Biosciences Faculty of Mathematics and Natural Sciences University of Oslo 2017 © Mark Adam Scott, 2018 Series of dissertations submitted to the Faculty of Mathematics and Natural Sciences, University of Oslo No. 1949 ISSN 1501-7710 All rights reserved. No part of this publication may be reproduced or transmitted, in any form or by any means, without permission. Cover: Hanne Baadsgaard Utigard. Print production: Reprosentralen, University of Oslo. Acknowledgements I would like to begin by expressing my gratitude to Göran Nilsson, Kåre-Olav Stensløkken, the Research Council of Norway, the European Research Council, and the University of Oslo for creating this opportunity for me. I am fortunate to have had supervisors that allowed me the freedom to explore the techniques that I was interested in developing. I am also grateful that my PhD enabled me not just to achieve the academic goals that I had set for myself but several other goals as well. Chief among them, being able to see as much of Europe as I’d hoped to. I was fortunate to have a talented and supportive group of colleagues and office mates throughout my PhD. Thank you Sjannie, Christina, Marco, Anette, and especially Cathrine, thank you for teaching me everything I needed to know about the entire process of qPCR, from cloning through to analysis. Antje, thank you for welcoming me into the world of electron microscopy. -

Downloaded Per Proteome Cohort Via the Web- Site Links of Table 1, Also Providing Information on the Deposited Spectral Datasets
www.nature.com/scientificreports OPEN Assessment of a complete and classifed platelet proteome from genome‑wide transcripts of human platelets and megakaryocytes covering platelet functions Jingnan Huang1,2*, Frauke Swieringa1,2,9, Fiorella A. Solari2,9, Isabella Provenzale1, Luigi Grassi3, Ilaria De Simone1, Constance C. F. M. J. Baaten1,4, Rachel Cavill5, Albert Sickmann2,6,7,9, Mattia Frontini3,8,9 & Johan W. M. Heemskerk1,9* Novel platelet and megakaryocyte transcriptome analysis allows prediction of the full or theoretical proteome of a representative human platelet. Here, we integrated the established platelet proteomes from six cohorts of healthy subjects, encompassing 5.2 k proteins, with two novel genome‑wide transcriptomes (57.8 k mRNAs). For 14.8 k protein‑coding transcripts, we assigned the proteins to 21 UniProt‑based classes, based on their preferential intracellular localization and presumed function. This classifed transcriptome‑proteome profle of platelets revealed: (i) Absence of 37.2 k genome‑ wide transcripts. (ii) High quantitative similarity of platelet and megakaryocyte transcriptomes (R = 0.75) for 14.8 k protein‑coding genes, but not for 3.8 k RNA genes or 1.9 k pseudogenes (R = 0.43–0.54), suggesting redistribution of mRNAs upon platelet shedding from megakaryocytes. (iii) Copy numbers of 3.5 k proteins that were restricted in size by the corresponding transcript levels (iv) Near complete coverage of identifed proteins in the relevant transcriptome (log2fpkm > 0.20) except for plasma‑derived secretory proteins, pointing to adhesion and uptake of such proteins. (v) Underrepresentation in the identifed proteome of nuclear‑related, membrane and signaling proteins, as well proteins with low‑level transcripts.