System Specific Trauma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Suplento1 Volumen 71 En
S1 Volumen 71 Mayo 2015 Revista Española de Vol. 71 Supl. 1 • Mayo 2015 Vol. Clínica e Investigación Órgano de expresión de la Sociedad Española de SEINAP Investigación en Nutrición y Alimentación en Pediatría Sumario XXX CONGRESO DE LA SOCIEDAD espaÑOLA DE CUIDADOS INTENSIVOS PEDIÁTRICOS Toledo, 7-9 de mayo de 2015 MESA REDONDA: ¿HACIA DÓNDE VAMOS EN LA MESA REDONDA: EL PACIENTE AGUDO MONITORIZACIÓN? CRONIFICADO EN UCIP 1 Monitorización mediante pulsioximetría: ¿sólo saturación 47 Nutrición en el paciente crítico de larga estancia en UCIP. de oxígeno? P. García Soler Z. Martínez de Compañón Martínez de Marigorta 3 Avances en la monitorización de la sedoanalgesia. S. Mencía 53 Traqueostomía, ¿cuándo realizarla? M.A. García Teresa Bartolomé y Grupo de Sedoanalgesia de la SECIP 60 Los cuidados de enfermería, ¿un reto? J.M. García Piñero 8 Avances en neuromonitorización. B. Cabeza Martín CHARLA-COLOQUIO SESIÓN DE PUESTA AL DÍA: ¿ES BENEFICIOSA LA 64 La formación en la preparación de las UCIPs FLUIDOTERAPIA PARA MI PACIENTE? españolas frente al riesgo de epidemias infecciosas. 13 Sobrecarga de líquidos y morbimortalidad asociada. J.C. de Carlos Vicente M.T. Alonso 68 Lecciones aprendidas durante la crisis del Ébola: 20 Estrategias de fluidoterapia racional en Cuidados experiencia del intensivista de adultos. J.C. Figueira Intensivos Pediátricos. P. de la Oliva Senovilla Iglesias 72 El niño con enfermedad por virus Ébola: un nuevo reto MESA REDONDA: INDICADORES DE CALIDAD para el intensivista pediátrico. E. Álvarez Rojas DE LA SECIP 23 Evolución de la cultura de seguridad en UCIP. MESA REDONDA: UCIP ABIERTAS 24 HORAS, La comunicación efectiva. -
Managing a Rib Fracture: a Patient Guide
Managing a Rib Fracture A Patient Guide What is a rib fracture? How is a fractured rib diagnosed? A rib fracture is a break of any of the bones that form the Your doctor will ask questions about your injury and do a rib cage. There may be a single fracture of one or more ribs, physical exam. or a rib may be broken into several pieces. Rib fractures are The doctor may: usually quite painful as the ribs have to move to allow for normal breathing. • Push on your chest to find out where you are hurt. • Watch you breathe and listen to your lungs to make What is a flail chest? sure air is moving in and out normally. When three or more neighboring ribs are fractured in • Listen to your heart. two or more places, a “flail chest” results. This creates an • Check your head, neck, spine, and belly to make sure unstable section of chest wall that moves in the opposite there are no other injuries. direction to the rest of rib cage when you take a breath. • You may need to have an X-ray or other imaging test; For example, when you breathe in your rib cage rises out however, rib fractures do not always show up on X-rays. but the flail chest portion of the rib cage will actually fall in. So you may be treated as though you have a fractured This limits your ability to take effective deep breaths. rib even if an X-ray doesn’t show any broken bones. -

Skin Injuries – Can We Determine Timing and Mechanism?
Skin injuries – can we determine timing and mechanism? Jo Tully VFPMS Seminar 2016 What skin injuries do we need to consider? • Bruising • Commonest accidental and inflicted skin injury • Basic principles that can be applied when formulating opinion • Abrasions • Lacerations }we need to be able to tell the difference • Incisions • Stabs/chops • Bite marks – animal v human / inflicted v ‘accidental’ v self-inflicted Our role…. We are often/usually/always asked…………….. • “What type of injury is it?” • “When did this injury occur?” • “How did this injury occur?” • “Was this injury inflicted or accidental?” • IS THIS CHILD ABUSE? • To be able to answer these questions (if we can) we need knowledge of • Anatomy/physiology/healing - injury interpretation • Forces • Mechanisms in relation to development, plausibility • Current evidence Bruising – can we really tell which bruises are caused by abuse? Definitions – bruising • BLUNT FORCE TRAUMA • Bruise =bleeding beneath intact skin due to BFT • Contusion = bruise in deeper tissues • Haematoma - extravasated blood filling a cavity (or potential space). Usually associated with swelling • Petechiae =Pinpoint sized (0.1-2mm) hemorrhages into the skin due to acute rise in venous pressure • medical causes • direct forces • indirect forces Medical Direct Indirect causes mechanical mechanical forces forces Factors affecting development and appearance of a bruise • Properties of impacting object or surface • Force of impact • Duration of impact • Site - properties of body region impacted (blood supply, -
Immune Thrombocytopenia Purpura (ITP)
Immune Thrombocytopenia Purpura (ITP) Information for patients and carers from the Haematology Department What is ITP? Immune thrombocytopenic purpura (ITP) is a condition which causes the number of platelets in Spleen your blood to be reduced. Platelets are cells that help blood to clot and they help to prevent bleeding and bruising after an injury. If you do not have enough platelets in your blood, you are likely to bruise easily or may be unable to stop bleeding if you cut yourself. In ITP, your body’s immune system destroys your own platelets. White blood cells in your blood and your spleen (an organ in your abdomen) are part of your immune system. One of their actions is to produce antibodies which help your body to fight Diagram showing the position of infections. If you develop ITP, your immune system the spleen becomes overactive and produces antibodies that cause your platelets to be destroyed in the spleen; this results in a low platelet count. ITP is a type of autoimmune condition (which means your immune system is acting against your body rather than for it). ITP in adults is more common in women than men. It is very different from ITP in children, who usually get ITP after a viral infection but who recover without any treatment. ITP in adults normally needs treatment. Some people with ITP have other autoimmune conditions, such as rheumatoid arthritis, or infections such as hepatitis or HIV. If you have any of these medical issues, your ITP may be treated slightly differently. 1 of 8 ITP (August 2021) A normal platelet count is between 150 and 400 thousand million platelets per litre of blood. -

Anesthesia for Trauma
Anesthesia for Trauma Maribeth Massie, CRNA, MS Staff Nurse Anesthetist, The Johns Hopkins Hospital Assistant Professor/Assistant Program Director Columbia University School of Nursing Program in Nurse Anesthesia OVERVIEW • “It’s not the speed which kills, it’s the sudden stop” Epidemiology of Trauma • ~8% worldwide death rate • Leading cause of death in Americans from 1- 45 years of age • MVC’s leading cause of death • Blunt > penetrating • Often drug abusers, acutely intoxicated, HIV and Hepatitis carriers Epidemiology of Trauma • “Golden Hour” – First hour after injury – 50% of patients die within the first seconds to minutesÆ extent of injuries – 30% of patients die in next few hoursÆ major hemorrhage – Rest may die in weeks Æ sepsis, MOSF Pre-hospital Care • ABC’S – Initial assessment and BLS in trauma – GO TEAM: role of CRNA’s at Maryland Shock Trauma Center • Resuscitation • Reduction of fractures • Extrication of trapped victims • Amputation • Uncooperative patients Initial Management Plan • Airway maintenance with cervical spine protection • Breathing: ventilation and oxygenation • Circulation with hemorrhage control • Disability • Exposure Initial Assessment • Primary Survey: – AIRWAY • ALWAYS ASSUME A CERVICAL SPINE INJURY EXISTS UNTIL PROVEN OTHERWISE • Provide MANUAL IN-LINE NECK STABILIZATION • Jaw-thrust maneuver Initial Assessment • Airway cont’d: – Cervical spine evaluation • Cross table lateral and swimmer’s view Xray • Need to see all seven cervical vertebrae • Only negative CT scan R/O injury Initial Assessment • Cervical -

Bleeds and Bruises in Children with Haemophilia
Bleeds and Bruises in CHildren WiTH HaeMOPHilia MusCle ANd/or JoiNt Bleeds Call the parent/guardian P.r.i.C.e. siGNs oF A serious HeAd Bleed P : Protection * Headache. Lower Limb: Take weight off the joint or muscle * drowsiness. Upper Limb: No carrying using affected arm * Nausea. r : rest * Vomiting. • Rest means rest! * unsteady Balance. • Try not to allow use of the joint or muscle where * irritability. possible. * Confusion. * seizures. i : ice * loss of consciousness. • Regular ice packs can help with pain & reduce swelling. • Put an ice pack over the affected area for 20 minutes. Repeat every two hours. DO NOT leave the ice pack on for more than 20 minutes siGNs oF A soFt tissue DO NOT place ice pack directly on skin (Use a tea Bleed towel/cold pack cover) * Bruising, discolouring of skin. C : Compression * Mild swelling. • Use an elasticated bandage to compress the affected area to reduce swelling. e : elevation • Elevate the affected limb to help reduce swelling. siGNs oF AN ABdoMiNAl • Keep the affected joint or muscle above the level of the Bleed heart. * Bloody, black or tar-like First Aid bowel motions. * red or brown urine. Mouth & Gum Bleeds * Pain. These can be hard to control because clots that form are * Vomiting of blood (blood washed away by saliva or knocked off by the tongue or food. Try giving the child an ice cube or ice pop to suck. may be red or black). These bleeds may need treatment by parents or the treatment centre. Nosebleeds siGNs oF BleediNG iNto tHe Tilt head forward and pinch the bridge of the nose below the bone for 10 - 20 minutes and / or put an ice-pack on JoiNts or MusCles the bridge of the nose for not more than 5 minutes. -

Delayed Traumatic Hemothorax in Older Adults
Open access Brief report Trauma Surg Acute Care Open: first published as 10.1136/tsaco-2020-000626 on 8 March 2021. Downloaded from Complication to consider: delayed traumatic hemothorax in older adults Jeff Choi ,1 Ananya Anand ,1 Katherine D Sborov,2 William Walton,3 Lawrence Chow,4 Oscar Guillamondegui,5 Bradley M Dennis,5 David Spain,1 Kristan Staudenmayer1 ► Additional material is ABSTRACT very small hemothoraces rarely require interven- published online only. To view, Background Emerging evidence suggests older adults tion whereas larger hemothoraces often undergo please visit the journal online immediate drainage. However, emerging evidence (http:// dx. doi. org/ 10. 1136/ may experience subtle hemothoraces that progress tsaco- 2020- 000626). over several days. Delayed progression and delayed suggests HTX in older adults with rib fractures may development of traumatic hemothorax (dHTX) have not experience subtle hemothoraces that progress in a 1Surgery, Stanford University, been well characterized. We hypothesized dHTX would delayed fashion over several days.1 2 If true, older Stanford, California, USA be infrequent but associated with factors that may aid adults may be at risk of developing empyema or 2Vanderbilt University School of Medicine, Nashville, Tennessee, prediction. other complications without close monitoring. USA Methods We retrospectively reviewed adults aged ≥50 Delayed progression and delayed development of 3Radiology, Vanderbilt University years diagnosed with dHTX after rib fractures at two traumatic hemothorax (dHTX) have not been well Medical Center, Nashville, level 1 trauma centers (March 2018 to September 2019). characterized in literature. The ageing US popula- Tennessee, USA tion and increasing incidence of rib fractures among 4Radiology, Stanford University, dHTX was defined as HTX discovered ≥48 hours after Stanford, California, USA admission chest CT showed either no or ’minimal/trace’ older adults underscore a pressing need for better 5Department of Surgery, HTX. -

Isolated Plantar Vein Thrombosis Resembling a Corn with a Bruise
JE Hahm, et al pISSN 1013-9087ㆍeISSN 2005-3894 Ann Dermatol Vol. 31, No. 1, 2019 https://doi.org/10.5021/ad.2019.31.1.66 CASE REPORT Isolated Plantar Vein Thrombosis Resembling a Corn with a Bruise Ji Eun Hahm, Kang Su Kim, Jae Won Ha, Chul Woo Kim, Sang Seok Kim Department of Dermatology, Kangdong Sacred Heart Hospital, College of Medicine, Hallym University, Seoul, Korea Plantar vein thrombosis, rarely-reported disease, is usually or callus, plantar fibromatosis, or plantar verruca1. Among accompanied by pain and tenderness in the plantar region laborers, they may develop from excess pressure on the and should be differentiated from other dermatological con- bony prominences of the feet, repetitive uneven friction ditions causing plantar pain, such as hemorrhagic corn/cal- from footwear, or gait abnormalities. Plantar vein throm- lus, plantar epidermal cyst, verruca, or plantar fibromatosis. bosis is a rare condition causing plantar pain. The exact A 52-year-old man presented with a violaceous tender sub- cause of plantar vein thrombosis is yet unclear, but predis- cutaneous nodule overlying a hyperkeratotic plaque on his posing conditions, such as prior trauma, surgery, paraneo- sole. Initially, he thought it was a corn and applied keratolytic plastic syndromes, or coagulation disorders have been agents, which failed to work. Sonography revealed a well-de- described. To date, there is no established treatment ex- marcated mass with increased peripheral vascularity. His cept surgical excision, but reportedly, nonsteroidal anti-in- pain was relieved after a complete wide excision, which con- flammatory drug or heparin with elastic bandage is known firmed the mass to be plantar vein thrombosis after histo- to be effective for symptomatic control2-5. -

Case Report Forearm Compartment Syndrome Following Thrombolytic Therapy for Massive Pulmonary Embolism: a Case Report and Review of Literature
Hindawi Publishing Corporation Case Reports in Orthopedics Volume 2011, Article ID 678525, 4 pages doi:10.1155/2011/678525 Case Report Forearm Compartment Syndrome following Thrombolytic Therapy for Massive Pulmonary Embolism: A Case Report and Review of Literature Ravi Badge and Mukesh Hemmady Department of Trauma and Orthopaedics Surgery, Wrightington, Wigan and Leigh NHS Trust, Wigan WN1 2NN, UK Correspondence should be addressed to Ravi Badge, [email protected] Received 2 November 2011; Accepted 6 December 2011 Academic Editor: M. K. Lyons Copyright © 2011 R. Badge and M. Hemmady. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Use of thrombolytic therapy in pulmonary embolism is restricted in cases of massive embolism. It achieves faster lysis of the thrombus than the conventional heparin therapy thus reducing the morbidity and mortality associated with PE. The compartment syndrome is a well-documented, potentially lethal complication of thrombolytic therapy and known to occur in the limbs involved for vascular lines or venepunctures. The compartment syndrome in a conscious and well-oriented patient is mainly diagnosed on clinical ground with its classical signs and symptoms like disproportionate pain, tense swollen limb and pain on passive stretch. However these findings may not be appropriately assessed in an unconscious patient and therefore the clinicians should have high index of suspicion in a patient with an acutely swollen tense limb. In such scenarios a prompt orthopaedic opinion should be considered. In this report, we present a case of acute compartment syndrome of the right forearm in a 78 years old male patient following repeated attempts to secure an arterial line for initiating the thrombolytic therapy for the management of massive pulmonary embolism. -

Pediatric Shock
REVIEW Pediatric shock Usha Sethuraman† & Pediatric shock accounts for significant mortality and morbidity worldwide, but remains Nirmala Bhaya incompletely understood in many ways, even today. Despite varied etiologies, the end result †Author for correspondence of pediatric shock is a state of energy failure and inadequate supply to meet the metabolic Children’s Hospital of Michigan, Division of demands of the body. Although the mortality rate of septic shock is decreasing, the severity Emergency Medicine, is on the rise. Changing epidemiology due to effective eradication programs has brought in Carman and Ann Adams new microorganisms. In the past, adult criteria had been used for the diagnosis and Department of Pediatrics, 3901 Beaubien Boulevard, management of septic shock in pediatrics. These have been modified in recent times to suit Detroit, MI 48201, USA the pediatric and neonatal population. In this article we review the pathophysiology, Tel.: +1 313 745 5260 epidemiology and recent guidelines in the management of pediatric shock. Fax: +1 313 993 7166 [email protected] Shock is an acute syndrome in which the circu- to generate ATP. It is postulated that in the face of latory system is unable to provide adequate oxy- prolonged systemic inflammatory insult, overpro- gen and nutrients to meet the metabolic duction of cytokines, nitric oxide and other medi- demands of vital organs [1]. Due to the inade- ators, and in the face of hypoxia and tissue quate ATP production to support function, the hypoperfusion, the body responds by turning off cell reverts to anaerobic metabolism, causing the most energy-consuming biophysiological acute energy failure [2]. -

Orthopedic Trauma Postoperative Care and Rehab
Orthopedic Trauma Postoperative Care and Rehab Serge Charles Kaska, MD Name that Beach 100$ Still 100$ 75$ 50$ 1$ Omaha • June 6th 1941 • !st Infantry Division • 2000 KIA LIFE OR LIMB THREAT 1. Compartment Syndrome 2. Fat Emboli Syndrome 3. Pulmonary Embolism 4. Shock Compartment syndrome case A 16 year old male was retrieving a tire from his truck bed on the side of the highway in the pouring rain when a car careens off of the road and sandwiches the patients legs between the bumpers at freeway speed. Acute compartment syndrome Compartment syndrome DEFINED Definition: Elevated tissue pressure within a closed fascial space • Pathogenesis – Too much in-flow: results in edema or hemorrhage – Decreased outflow: results in venous obstruction caused by tight dressing and/or cast. • Reduces tissue perfusion • Results in cell death Compartment syndrome tissue survival • Muscle – 3-4 hours: reversible changes – 6 hours: variable damage – 8 hours: irreversible changes • Nerve – 2 hours: looses nerve conduction – 4 hours: neuropraxia – 8 hours: irreversible changes Physical exam 1. Pain 2. Pain 3. Pain Physical exam • Inspection – Swelling, skin is tight and shiny • Motion – Active motion will be refused or unable. Must see dorsiflexion • Palpation – Severe pain with palpation • Alarming pain with passive stretch Physical exam • Dorsiflexion Physical Exam • Palpation – Severe pain with palpation • Alarming pain with passive stretch Physical exam • Evaluations from nurses, therapists, and orthotech’s are CRITICAL • If you call a doctor and say that -
Mechanical Ventilation Guide
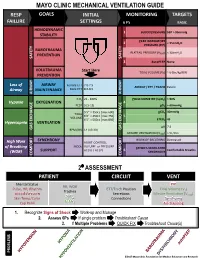
MAYO CLINIC MECHANICAL VENTILATION GUIDE RESP GOALS INITIAL MONITORING TARGETS FAILURE SETTINGS 6 P’s BASIC HEMODYNAMIC 1 BLOOD PRESSURE SBP > 90mmHg STABILITY PEAK INSPIRATORY 2 < 35cmH O PRESSURE (PIP) 2 BAROTRAUMA PLATEAU PRESSURE (P ) < 30cmH O PREVENTION PLAT 2 SAFETY SAFETY 3 AutoPEEP None VOLUTRAUMA Start Here TIDAL VOLUME (V ) ~ 6-8cc/kg IBW PREVENTION T Loss of AIRWAY Female ETT 7.0-7.5 AIRWAY / ETT / TRACH Patent Airway MAINTENANCE Male ETT 8.0-8.5 AIRWAY AIRWAY FiO2 21 - 100% PULSE OXIMETRY (SpO2) > 90% Hypoxia OXYGENATION 4 PEEP 5 [5-15] pO2 > 60mmHg 5’5” = 350cc [max 600] pCO2 40mmHg TIDAL 6’0” = 450cc [max 750] 5 VOLUME 6’5” = 500cc [max 850] ETCO2 45 Hypercapnia VENTILATION pH 7.4 GAS GAS EXCHANGE BPM (RR) 14 [10-30] GAS EXCHANGE MINUTE VENTILATION (VMIN) > 5L/min SYNCHRONY WORK OF BREATHING Decreased High Work ASSIST CONTROL MODE VOLUME or PRESSURE of Breathing PATIENT-VENTILATOR AC (V) / AC (P) 6 Comfortable Breaths (WOB) SUPPORT SYNCHRONY COMFORT COMFORT 2⁰ ASSESSMENT PATIENT CIRCUIT VENT Mental Status PIP RR, WOB Pulse, HR, Rhythm ETT/Trach Position Tidal Volume (V ) Trachea T Blood Pressure Secretions Minute Ventilation (V ) SpO MIN Skin Temp/Color 2 Connections Synchrony ETCO Cap Refill 2 Air-Trapping 1. Recognize Signs of Shock Work-up and Manage 2. Assess 6Ps If single problem Troubleshoot Cause 3. If Multiple Problems QUICK FIX Troubleshoot Cause(s) PROBLEMS ©2017 Mayo Clinic Foundation for Medical Education and Research CAUSES QUICK FIX MANAGEMENT Bleeding Hemostasis, Transfuse, Treat cause, Temperature control HYPOVOLEMIA Dehydration Fluid Resuscitation (End points = hypoxia, ↑StO2, ↓PVI) 3rd Spacing Treat cause, Beware of hypoxia (3rd spacing in lungs) Pneumothorax Needle D, Chest tube Abdominal Compartment Syndrome FLUID Treat Cause, Paralyze, Surgery (Open Abdomen) OBSTRUCTED BLOOD RETURN Air-Trapping (AutoPEEP) (if not hypoxic) Pop off vent & SEE SEPARATE CHART PEEP Reduce PEEP Cardiac Tamponade Pericardiocentesis, Drain.