Assessment, Management and Decision Making in the Treatment of Polytrauma Patients with Head Injuries
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Crush Injuries Pathophysiology and Current Treatment Michael Sahjian, RN, BSN, CFRN, CCRN, NREMT-P; Michael Frakes, APRN, CCNS, CCRN, CFRN, NREMT-P
LWW/AENJ LWWJ331-02 April 23, 2007 13:50 Char Count= 0 Advanced Emergency Nursing Journal Vol. 29, No. 2, pp. 145–150 Copyright c 2007 Wolters Kluwer Health | Lippincott Williams & Wilkins Crush Injuries Pathophysiology and Current Treatment Michael Sahjian, RN, BSN, CFRN, CCRN, NREMT-P; Michael Frakes, APRN, CCNS, CCRN, CFRN, NREMT-P Abstract Crush syndrome, or traumatic rhabdomyolysis, is an uncommon traumatic injury that can lead to mismanagement or delayed treatment. Although rhabdomyolysis can result from many causes, this article reviews the risk factors, symptoms, and best practice treatments to optimize patient outcomes, as they relate to crush injuries. Key words: crush syndrome, traumatic rhabdomyolysis RUSH SYNDROME, also known as ology, pathophysiology, diagnosis, and early traumatic rhabdomyolysis, was first re- management of crush syndrome. Cported in 1910 by German authors who described symptoms including muscle EPIDEMIOLOGY pain, weakness, and brown-colored urine in soldiers rescued after being buried in struc- Crush injuries may result in permanent dis- tural debris (Gonzalez, 2005). Crush syn- ability or death; therefore, early recognition drome was not well defined until the 1940s and aggressive treatment are necessary to when nephrologists Bywaters and Beal pro- improve outcomes. There are many known vided descriptions of victims trapped by mechanisms inducing rhabdomyolysis includ- their extremities during the London Blitz ing crush injuries, electrocution, burns, com- who presented with shock, swollen extrem- partment syndrome, and any other pathology ities, tea-colored urine, and subsequent re- that results in muscle damage. Victims of nat- nal failure (Better & Stein, 1990; Fernan- ural disasters, including earthquakes, are re- dez, Hung, Bruno, Galea, & Chiang, 2005; ported as having up to a 20% incidence of Gonzalez, 2005; Malinoski, Slater, & Mullins, crush injuries, as do 40% of those surviving to 2004). -

Case Report Forearm Compartment Syndrome Following Thrombolytic Therapy for Massive Pulmonary Embolism: a Case Report and Review of Literature
Hindawi Publishing Corporation Case Reports in Orthopedics Volume 2011, Article ID 678525, 4 pages doi:10.1155/2011/678525 Case Report Forearm Compartment Syndrome following Thrombolytic Therapy for Massive Pulmonary Embolism: A Case Report and Review of Literature Ravi Badge and Mukesh Hemmady Department of Trauma and Orthopaedics Surgery, Wrightington, Wigan and Leigh NHS Trust, Wigan WN1 2NN, UK Correspondence should be addressed to Ravi Badge, [email protected] Received 2 November 2011; Accepted 6 December 2011 Academic Editor: M. K. Lyons Copyright © 2011 R. Badge and M. Hemmady. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Use of thrombolytic therapy in pulmonary embolism is restricted in cases of massive embolism. It achieves faster lysis of the thrombus than the conventional heparin therapy thus reducing the morbidity and mortality associated with PE. The compartment syndrome is a well-documented, potentially lethal complication of thrombolytic therapy and known to occur in the limbs involved for vascular lines or venepunctures. The compartment syndrome in a conscious and well-oriented patient is mainly diagnosed on clinical ground with its classical signs and symptoms like disproportionate pain, tense swollen limb and pain on passive stretch. However these findings may not be appropriately assessed in an unconscious patient and therefore the clinicians should have high index of suspicion in a patient with an acutely swollen tense limb. In such scenarios a prompt orthopaedic opinion should be considered. In this report, we present a case of acute compartment syndrome of the right forearm in a 78 years old male patient following repeated attempts to secure an arterial line for initiating the thrombolytic therapy for the management of massive pulmonary embolism. -

Orthopedic Trauma Postoperative Care and Rehab
Orthopedic Trauma Postoperative Care and Rehab Serge Charles Kaska, MD Name that Beach 100$ Still 100$ 75$ 50$ 1$ Omaha • June 6th 1941 • !st Infantry Division • 2000 KIA LIFE OR LIMB THREAT 1. Compartment Syndrome 2. Fat Emboli Syndrome 3. Pulmonary Embolism 4. Shock Compartment syndrome case A 16 year old male was retrieving a tire from his truck bed on the side of the highway in the pouring rain when a car careens off of the road and sandwiches the patients legs between the bumpers at freeway speed. Acute compartment syndrome Compartment syndrome DEFINED Definition: Elevated tissue pressure within a closed fascial space • Pathogenesis – Too much in-flow: results in edema or hemorrhage – Decreased outflow: results in venous obstruction caused by tight dressing and/or cast. • Reduces tissue perfusion • Results in cell death Compartment syndrome tissue survival • Muscle – 3-4 hours: reversible changes – 6 hours: variable damage – 8 hours: irreversible changes • Nerve – 2 hours: looses nerve conduction – 4 hours: neuropraxia – 8 hours: irreversible changes Physical exam 1. Pain 2. Pain 3. Pain Physical exam • Inspection – Swelling, skin is tight and shiny • Motion – Active motion will be refused or unable. Must see dorsiflexion • Palpation – Severe pain with palpation • Alarming pain with passive stretch Physical exam • Dorsiflexion Physical Exam • Palpation – Severe pain with palpation • Alarming pain with passive stretch Physical exam • Evaluations from nurses, therapists, and orthotech’s are CRITICAL • If you call a doctor and say that -
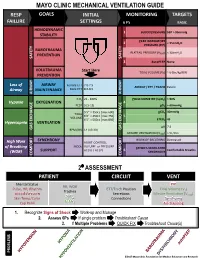
Mechanical Ventilation Guide
MAYO CLINIC MECHANICAL VENTILATION GUIDE RESP GOALS INITIAL MONITORING TARGETS FAILURE SETTINGS 6 P’s BASIC HEMODYNAMIC 1 BLOOD PRESSURE SBP > 90mmHg STABILITY PEAK INSPIRATORY 2 < 35cmH O PRESSURE (PIP) 2 BAROTRAUMA PLATEAU PRESSURE (P ) < 30cmH O PREVENTION PLAT 2 SAFETY SAFETY 3 AutoPEEP None VOLUTRAUMA Start Here TIDAL VOLUME (V ) ~ 6-8cc/kg IBW PREVENTION T Loss of AIRWAY Female ETT 7.0-7.5 AIRWAY / ETT / TRACH Patent Airway MAINTENANCE Male ETT 8.0-8.5 AIRWAY AIRWAY FiO2 21 - 100% PULSE OXIMETRY (SpO2) > 90% Hypoxia OXYGENATION 4 PEEP 5 [5-15] pO2 > 60mmHg 5’5” = 350cc [max 600] pCO2 40mmHg TIDAL 6’0” = 450cc [max 750] 5 VOLUME 6’5” = 500cc [max 850] ETCO2 45 Hypercapnia VENTILATION pH 7.4 GAS GAS EXCHANGE BPM (RR) 14 [10-30] GAS EXCHANGE MINUTE VENTILATION (VMIN) > 5L/min SYNCHRONY WORK OF BREATHING Decreased High Work ASSIST CONTROL MODE VOLUME or PRESSURE of Breathing PATIENT-VENTILATOR AC (V) / AC (P) 6 Comfortable Breaths (WOB) SUPPORT SYNCHRONY COMFORT COMFORT 2⁰ ASSESSMENT PATIENT CIRCUIT VENT Mental Status PIP RR, WOB Pulse, HR, Rhythm ETT/Trach Position Tidal Volume (V ) Trachea T Blood Pressure Secretions Minute Ventilation (V ) SpO MIN Skin Temp/Color 2 Connections Synchrony ETCO Cap Refill 2 Air-Trapping 1. Recognize Signs of Shock Work-up and Manage 2. Assess 6Ps If single problem Troubleshoot Cause 3. If Multiple Problems QUICK FIX Troubleshoot Cause(s) PROBLEMS ©2017 Mayo Clinic Foundation for Medical Education and Research CAUSES QUICK FIX MANAGEMENT Bleeding Hemostasis, Transfuse, Treat cause, Temperature control HYPOVOLEMIA Dehydration Fluid Resuscitation (End points = hypoxia, ↑StO2, ↓PVI) 3rd Spacing Treat cause, Beware of hypoxia (3rd spacing in lungs) Pneumothorax Needle D, Chest tube Abdominal Compartment Syndrome FLUID Treat Cause, Paralyze, Surgery (Open Abdomen) OBSTRUCTED BLOOD RETURN Air-Trapping (AutoPEEP) (if not hypoxic) Pop off vent & SEE SEPARATE CHART PEEP Reduce PEEP Cardiac Tamponade Pericardiocentesis, Drain. -

Acute Compartment Syndrome Complicating Deep Venous Thrombosis
SMGr up Case Report SM Journal of Acute Compartment Syndrome Case Reports Complicating Deep Venous Thrombosis Senthil Dhayalan1*, David Jardine1*, Tony Goh2 and Nicholas Lash3 1Senior registrar and General Physician, Dept of General Medicine, NZ 2Consultant Radiologist, Dept of Radiology, NZ 3Orthopaediac Surgeon, Dept of Orthopaedics, NZ A 40-yr old, heavily-built man initially presented to his general practitioner 2 days before Article Information admission with recent onset of pain and swelling in his left calf. A duplex ultrasound scan Received date: Nov 21, 2018 demonstrated a popliteal and lower leg deep vein thrombosis [DVT], extending 15 cm above the Accepted date: Nov 26, 2018 knee into the femoral vein. He was started appropriately on enoxaparin 130 mg bd. Despite the Published date: Nov 27, 2018 treatment, the pain got worse, particularly when standing, and he was admitted for symptom control. Five weeks earlier he had undergone anterior cruciate ligament repair of the left knee, *Corresponding author [without heparin prophylaxis] and made a satisfactory recovery (Figure 1). Jardine D, General Medicine On examination he was mildly distressed with a low-normal blood pressure [110/70 mmHg] Department, Christchurch hospital, and a persistent low-grade fever [temperature ranged from 37.0-37.8 oC]. The left leg was moderately Private Bag 4710, Christchurch 8140, diffusely swollen, slightly warm and darker in colour [figure]. The pain was localised to the posterior New Zealand, compartments and was exacerbated by dorsi-flexing the ankle and squeezing the gastrocnemius. Email: [email protected] There were no signs of joint effusion, thrombophlebitis, lymphadenopathy or cellulitis. -

ISR/PFC Crush Injury Clinical Practice Guideline
All articles published in the Journal of Special Operations Medicine are protected by United States copyright law and may not be reproduced, distributed, transmitted, displayed, or otherwise published without the prior written permission of Breakaway Media, LLC. Contact [email protected]. An Ongoing Series Management of Crush Syndrome Under Prolonged Field Care Thomas Walters, PhD; Douglas Powell, MD; Andrew Penny, NREMT-P; Ian Stewart, MD; Kevin Chung, MD; Sean Keenan, MD; Stacy Shackelford, MD Introduction to the Prolonged Field Care beyond the initial evaluation and treatment of casual- Prehospital Clinical Practice Guideline Series ties in a PFC operational environment. This and fu- ture CPGs are aimed at serious clinical problems seen Sean Keenan, MD less frequently (e.g., crush injury, burns) or where fur- ther advanced practice recommendations are required THIS FIRST CLINICAL PRACTICE GUIDELINE (CPG) (e.g., pain and sedation recommendations beyond was produced through a collaboration of the SOMA TCCC recommendations, traumatic brain injury). Prolonged Field Care Working Group (PFCWG) and the Joint Trauma System (JTS) at the U.S. Army Insti- We hope that this collaboration of experienced op- tute of Surgical Research (USAISR) in San Antonio. Of erational practitioners and true subject matter ex- note, this effort is the result from requests for informa- perts, operating under the guidance set forth in past tion and guidance through the PFC website (PFCare.org) JTS CPG editorial standards, will bring practical and and from the Joint Special Operations Medical Training applicable clinical recommendations to the advanced Center instructors located at Fort Bragg, North Carolina. practice first responders and Role 1 providers in the field. -

With Crush Injury Syndrome
Crush Syndrome Made Simple Malta & McConnelsville Fire Department Division of Emergency Medical Service Objectives Recognize the differences between Crush Injury and Crush Syndrome Understand the interventions performed when treating someone with Crush Syndrome Assessing the Crush Injury victim S&S of crush injuries Treatment of crush injury Malta & McConnelsville Fire Department Division of Emergency Medical Service INJURY SYNDROME • Cell Disruption/ • Systemic effects injury at the point of when muscle is impact. RELEASED from Compression • Occurs < 1 hour • Occurs after cells have been under pressure >4 hours* • Suspect Syndrome with lightening strikes Malta & McConnelsville Fire Department Division of Emergency Medical Service CRUSHING MECHANISM OF INJURY • Building and Structure Collapse • Bomb Concussions • MVAs’ and Farm Accidents • Assault with blunt weapon Malta & McConnelsville Fire Department Division of Emergency Medical Service AKA: COMPRESSION SYNDROME First described by Dr. Minami in 1940 Malta & McConnelsville Fire Department Division of Emergency Medical Service INVOLVED ANATOMY Upper Arms Upper Legs Thorax and Buttocks Malta & McConnelsville Fire Department Division of Emergency Medical Service Crush Injuries Crush injuries occur when a crushing force is applied to a body area. Sometimes they are associated with internal organ rupture, major fractures, and hemorrhagic shock. Early aggressive treatment of patients suspected of having a crush injury is crucial. Along with the severity of soft tissue damage and fractures, a major concern of a severe crush injury is the duration of the compression/entrapment. Malta & McConnelsville Fire Department Division of Emergency Medical Service Crush Injuries Prolonged compression of a body region or limb may lead to a dangerous syndrome that can become fatal. Crush Syndrome is difficult to diagnose and treat in the pre-hospital setting because of the many complex variables involved. -

Bilateral Atraumatic Compartment Syndrome of the Legs Leading to Rhabdomyolysis and Acute Renal Failure Following Prolonged Kneeling in a Heroin Addict
PAJT 10.5005/jp-journals-10030-1075 CASE REPORTBilateral Atraumatic Compartment Syndrome of the Legs Leading to Rhabdomyolysis and Acute Renal Failure Bilateral Atraumatic Compartment Syndrome of the Legs Leading to Rhabdomyolysis and Acute Renal Failure Following Prolonged Kneeling in a Heroin Addict. A Case Report and Review of Relevant Literature Saptarshi Biswas, Ramya S Rao, April Duckworth, Ravi Kothuru, Lucio Flores, Sunil Abrol ABSTRACT cerrado, que interfiere con la circulación de los componentes mioneurales del compartimento. Síndrome compartimental Introduction: Compartment syndrome is defined as a symptom bilateral de las piernas es una presentación raro que requiere complex caused by increased pressure of tissue fluid in a closed una intervención quirúrgica urgente. En un reporte reciente osseofascial compartment which interferes with circulation (Khan et al 2012), ha habido reportados solo 8 casos de to the myoneural components of the compartment. Bilateral síndrome compartimental bilateral. compartment syndrome of the legs is a rare presentation Se sabe que el abuso de heroína puede causar el síndrome requiring emergent surgical intervention. In a recent case report compartimental y rabdomiólisis traumática y atraumática. El (Khan et al 2012) there have been only eight reported cases hipotiroidismo también puede presentarse independiente con cited with bilateral compartment syndrome. rabdomiólisis. Heroin abuse is known to cause compartment syndrome, traumatic and atraumatic rhabdomyolysis. Hypothyroidism can Presentación del caso: Presentamos un caso de una mujer also independently present with rhabdomyolysis. de 22 años quien presentó con tumefacción bilateral de las piernas asociado con la perdida de la sensación, después Case presentation: We present a case of a 22 years old female de pasar dos días arrodillado contra una pared después de who presented with bilateral swelling of the legs with associated usar heroína intravenosa. -

Western Trauma Association Critical Decisions in Trauma: Penetrating Chest Trauma
WTA 2014 ALGORITHM Western Trauma Association Critical Decisions in Trauma: Penetrating chest trauma Riyad Karmy-Jones, MD, Nicholas Namias, MD, Raul Coimbra, MD, Ernest E. Moore, MD, 09/30/2020 on BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3Ypodx1mzGi19a2VIGqBjfv9YfiJtaGCC1/kUAcqLCxGtGta0WPrKjA== by http://journals.lww.com/jtrauma from Downloaded Martin Schreiber, MD, Robert McIntyre, Jr., MD, Martin Croce, MD, David H. Livingston, MD, Jason L. Sperry, MD, Ajai K. Malhotra, MD, and Walter L. Biffl, MD, Portland, Oregon Downloaded from http://journals.lww.com/jtrauma his is a recommended algorithm of the Western Trauma Historical Perspective TAssociation for the acute management of penetrating chest The precise incidence of penetrating chest injury, varies injury. Because of the paucity of recent prospective randomized depending on the urban environment and the nature of the trials on the evaluation and management of penetrating chest review. Overall, penetrating chest injuries account for 1% to injury, the current algorithms and recommendations are based 13% of trauma admissions, and acute exploration is required in by on available published cohort, observational and retrospective BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3Ypodx1mzGi19a2VIGqBjfv9YfiJtaGCC1/kUAcqLCxGtGta0WPrKjA== 5% to 15% of cases; exploration is required in 15% to 30% of studies, and the expert opinion of the Western Trauma Asso- patients who are unstable or in whom active hemorrhage is ciation members. The two algorithms should be reviewed in the suspected. Among patients managed by tube thoracostomy following sequence: Figure 1 for the management and damage- alone, complications including retained hemothorax, empy- control strategies in the unstable patient and Figure 2 for the ema, persistent air leak, and/or occult diaphragmatic injuries management and definitive repair strategies in the stable patient. -

Secondary Abdominal Compartment Syndrome Following Severe Extremity Injury: Unavoidable Or Unnecessary?
Session IV Poster # 1 SECONDARY ABDOMINAL COMPARTMENT SYNDROME FOLLOWING SEVERE EXTREMITY INJURY: UNAVOIDABLE OR UNNECESSARY? Bryan A Cotton MD, Michael C Madigan BS, Clinton D Kemp MD, J Chad Johnson MD PhD, John A Morris Jr MD*, Vanderbilt University Medical Center, Nashville, TN Introduction: Secondary abdominal compartment syndrome (2ACS) is the development of ACS in the absence of abdominal injury. 2ACS is often viewed as an unavoidable sequela of the large volume crystalloid resuscitation “required” to treat severe shock. We hypothesized that early, aggressive resuscitation techniques place patients with severe extremity injuries at risk for developing 2ACS. Methods: The TRACS database was queried for all patients with extremity AIS of 3 or greater and abdominal AIS of 0 treated at our institution between 01/01/2001-12/31/2005. The study group included those patients who developed 2ACS, while the comparison cohort included those who did not develop 2ACS. Results: 48 patients developed 2 ACS and were compared to 48 randomly sampled patients who had extremity AIS of ? 3 and abdomen AIS of 0. There were no differences between the groups with respect to age, sex, race, or individual AIS scores. However, the 2ACS group had a higher ISS (25.6 vs 21.4, p=0.02), higher OR crystalloid administration (9.9 L vs 2.7 L, p<0.001), and more frequent use of a rapid infuser (12.5% vs 0.0%, p=0.01). 65% of those who developed 2ACS did so within 12 hours of admission. Multiple logistic regression identified pre-hospital and ED crystalloid volume as predictors of 2ACS. -

Idiopathic Acute Compartment Syndrome of the Leg with Incidental Deep Venous Thrombosis: a Case Report
Open Access Case Report DOI: 10.7759/cureus.5130 Idiopathic Acute Compartment Syndrome of the Leg with Incidental Deep Venous Thrombosis: A Case Report Ehizogie Edigin 1 , Hafeez Shaka 1 1. Internal Medicine, John H. Stroger Jr. Hospital of Cook County, Chicago, USA Corresponding author: Ehizogie Edigin, [email protected] Abstract Acute compartment syndrome (ACS) is an emergency. The majority of cases are caused by underlying trauma, especially fractures. Idiopathic atraumatic ACS of the leg is very rare. The diagnosis and management of ACS should focus on the clinical presentation to avoid delay in fasciotomy for limb salvage. ACS of the leg can be caused by massive proximal iliofemoral thrombosis and rarely occlusive popliteal vein thrombosis with total or near total occlusion. Nonocclusive distal popliteal vein thrombosis, especially if chronic, does not cause ACS and when seen in a patient with ACS, it is likely an incidental finding rather than the cause of the compartment syndrome. This is a case of idiopathic ACS of the right leg occurring in the presence of an incidental right chronic nonocclusive distal popliteal vein thrombosis. Categories: Cardiology, Emergency Medicine, Orthopedics Keywords: acute compartment syndrome, deep vein thrombosis, anticoagulation, fasciotomy, idiopathic acute compartment syndrome, spontaneous acute compartment syndrome, acute extremity compartment syndrome Introduction Acute compartment syndrome (ACS) occurs when increased pressure within a compartment, bounded by unyielding fascial membranes, compromises the circulation and function of the tissues within that space [1]. This increased pressure compromises the function and with time, the viability of the limb affected. However, the diagnosis can be challenging as the symptoms associated with ACS can also be found in other often more common conditions [2]. -

Ad Ult T Ra Uma Em E Rgen Cies
Section SECTION: Adult Trauma Emergencies REVISED: 06/2017 4 ADULT TRAUMA EMERGENCIES TRAUMA ADULT 1. Injury – General Trauma Management Protocol 4 - 1 2. Injury – Abdominal Trauma Protocol 4 - 2 (Abdominal Trauma) 3. Injury – Burns - Thermal Protocol 4 - 3 4. Injury – Crush Syndrome Protocol 4 - 4 5. Injury – Electrical Injuries Protocol 4 - 5 6. Injury – Head Protocol 4 - 6 7. Exposure – Airway/Inhalation Irritants Protocol 4 - 7 8. Injury – Sexual Assault Protocol 4 - 8 9. General – Neglect or Abuse Suspected Protocol 4 - 9 10. Injury – Conducted Electrical Weapons Protocol 4 - 10 (i.e. Taser) 11. Injury - Thoracic Protocol 4 - 11 12. Injury – General Trauma Management Protocol 4 – 12 (Field Trauma Triage Scheme) 13. Spinal Motion Restriction Protocol 4 – 13 14. Hemorrhage Control Protocol 4 – 14 Section 4 Continued This page intentionally left blank. ADULT TRAUMA EMERGENCIES ADULT Protocol SECTION: Adult Trauma Emergencies PROTOCOL TITLE: Injury – General Trauma Management 4-1 REVISED: 06/2015 PATIENT TRAUMA ASSESSMENT OVERVIEW Each year, one out of three Americans sustains a traumatic injury. Trauma is a major cause of disability in the United States. According to the Centers for Disease Control (CDC) in 2008, 118,021 deaths occurred due to trauma. Trauma is the leading cause of death in people under 44 years of age, accounting for half the deaths of children under the age of 4 years, and 80% of deaths in persons 15 to 24 years of age. As a responder, your actions within the first few moments of arriving on the scene of a traumatic injury are crucial to the success of managing the situation.