Secondary Abdominal Compartment Syndrome Following Severe Extremity Injury: Unavoidable Or Unnecessary?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Thoracic and Abdominal Trauma
INJURIESINJURIES TOTO THETHE TRUNKTRUNK THROACIC AND ABDOMINAL INJURIES INITIALINITIAL ASSESSMENTASSESSMENT 1. PRIMARY SURVEY (1. MIN) 2. VITAL FUNCTIONS TREAT LIFE THREATENING FIRST 3. SECONDARY SURVEY 4. DEFINITIVE CARE A.B.C.D.E. LIFELIFE THREATENINGTHREATENING INJURIESINJURIES A. INJURIES TO THE AIRWAYS B. TENSION PTX SUCKING CHEST WOUND MASSIVE HEMOTHORAX FLAIL CHEST C. CARDIAC TAMPONADE MASSIVE HEMOTHORAX LIFELIFE THREATENINGTHREATENING CHESTCHEST INJURIESINJURIES •PNEUMOTHORAX •HEMOTHORAX •PULMONARY CONTUSION •TRACHEBRONCHIAL TREE INJURY •BLUNT CARDIAC INJURY •TRAUMATIC AORTIC INJURY •TRAMATIC DIAPHRAGMATIG INJURY •MEDIASTINAL TRANSVERSING WOUNDS PNEUMOTHORAXPNEUMOTHORAX AIR BETWEEN THE PARIETAL AND VISCERAL PLEURA RIB FRACTURES INJURIES TO THE LUNG INJURIES TO THE AIRWAYS BULLAS IATROGENIG FROM THE RETROPERITONEUM PNEUMOTHORAXPNEUMOTHORAX 1. 2. TENSIONTENSION PNEUMOTHORAXPNEUMOTHORAX ONE WAY VALVE – AIR FROM THE LUNG OR THROUGH THE CHEST WALL INTO THE THORACIC CAVITY CONSEQUENCE: HYPOXIA, BLOCKING OF THE VENOUS INFLOW CHEST PAIN, AIR HUNGER, HYPOTENSION, NECK VEIN DISTENSION, TACHYCARDIA CARDIAC TAMPONADE – NO BREATH SOUNDS IMMEDIATE TREATMENT TENSIONTENSION PNEUMOTHORAXPNEUMOTHORAX TENSION PTX NEEDLE THORACOCENTESIS HEMOTHORAXHEMOTHORAX BLOOD IN THE THORACIC CAVITY LUNG LACERATION RIB FRACTURE INTERCOSTAL VESSEL INJURY ART. MAMMARY INJURY PENETRATING OR BLUNT INJURY HEMOTHORAXHEMOTHORAX 1. ? 2. ! HTXHTX HEMOTHORAXHEMOTHORAX TREATMENT : CHEST TUBE – THORACOTOMY IS RARELY INDICATED THORACOTOMY: 1500 ML / DRAINAGE OR 200 ML/ HOUR -

Anesthesia for Trauma
Anesthesia for Trauma Maribeth Massie, CRNA, MS Staff Nurse Anesthetist, The Johns Hopkins Hospital Assistant Professor/Assistant Program Director Columbia University School of Nursing Program in Nurse Anesthesia OVERVIEW • “It’s not the speed which kills, it’s the sudden stop” Epidemiology of Trauma • ~8% worldwide death rate • Leading cause of death in Americans from 1- 45 years of age • MVC’s leading cause of death • Blunt > penetrating • Often drug abusers, acutely intoxicated, HIV and Hepatitis carriers Epidemiology of Trauma • “Golden Hour” – First hour after injury – 50% of patients die within the first seconds to minutesÆ extent of injuries – 30% of patients die in next few hoursÆ major hemorrhage – Rest may die in weeks Æ sepsis, MOSF Pre-hospital Care • ABC’S – Initial assessment and BLS in trauma – GO TEAM: role of CRNA’s at Maryland Shock Trauma Center • Resuscitation • Reduction of fractures • Extrication of trapped victims • Amputation • Uncooperative patients Initial Management Plan • Airway maintenance with cervical spine protection • Breathing: ventilation and oxygenation • Circulation with hemorrhage control • Disability • Exposure Initial Assessment • Primary Survey: – AIRWAY • ALWAYS ASSUME A CERVICAL SPINE INJURY EXISTS UNTIL PROVEN OTHERWISE • Provide MANUAL IN-LINE NECK STABILIZATION • Jaw-thrust maneuver Initial Assessment • Airway cont’d: – Cervical spine evaluation • Cross table lateral and swimmer’s view Xray • Need to see all seven cervical vertebrae • Only negative CT scan R/O injury Initial Assessment • Cervical -

Case Report Forearm Compartment Syndrome Following Thrombolytic Therapy for Massive Pulmonary Embolism: a Case Report and Review of Literature
Hindawi Publishing Corporation Case Reports in Orthopedics Volume 2011, Article ID 678525, 4 pages doi:10.1155/2011/678525 Case Report Forearm Compartment Syndrome following Thrombolytic Therapy for Massive Pulmonary Embolism: A Case Report and Review of Literature Ravi Badge and Mukesh Hemmady Department of Trauma and Orthopaedics Surgery, Wrightington, Wigan and Leigh NHS Trust, Wigan WN1 2NN, UK Correspondence should be addressed to Ravi Badge, [email protected] Received 2 November 2011; Accepted 6 December 2011 Academic Editor: M. K. Lyons Copyright © 2011 R. Badge and M. Hemmady. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Use of thrombolytic therapy in pulmonary embolism is restricted in cases of massive embolism. It achieves faster lysis of the thrombus than the conventional heparin therapy thus reducing the morbidity and mortality associated with PE. The compartment syndrome is a well-documented, potentially lethal complication of thrombolytic therapy and known to occur in the limbs involved for vascular lines or venepunctures. The compartment syndrome in a conscious and well-oriented patient is mainly diagnosed on clinical ground with its classical signs and symptoms like disproportionate pain, tense swollen limb and pain on passive stretch. However these findings may not be appropriately assessed in an unconscious patient and therefore the clinicians should have high index of suspicion in a patient with an acutely swollen tense limb. In such scenarios a prompt orthopaedic opinion should be considered. In this report, we present a case of acute compartment syndrome of the right forearm in a 78 years old male patient following repeated attempts to secure an arterial line for initiating the thrombolytic therapy for the management of massive pulmonary embolism. -

Characteristics and Management of Penetrating Abdominal Injuries in a German Level I Trauma Center
European Journal of Trauma and Emergency Surgery (2019) 45:315–321 https://doi.org/10.1007/s00068-018-0911-1 ORIGINAL ARTICLE Characteristics and management of penetrating abdominal injuries in a German level I trauma center Patrizia Malkomes1 · Philipp Störmann2 · Hanan El Youzouri1 · Sebastian Wutzler2 · Ingo Marzi2 · Thomas Vogl3 · Wolf Otto Bechstein1 · Nils Habbe4 Received: 19 October 2017 / Accepted: 13 January 2018 / Published online: 22 January 2018 © Springer-Verlag GmbH Germany, part of Springer Nature 2018 Abstract Purpose Penetrating abdominal injuries caused by stabbing or firearms are rare in Germany, thus there is lack of descriptive studies. The management of hemodynamically stable patients is still under dispute. The aim of this study is to review and improve our management of penetrating abdominal injuries. Methods We retrospectively reviewed a 10-year period from the Trauma Registry of our level I trauma center. The data of all patients regarding demographics, clinical and outcome parameters were examined. Further, charts were reviewed for FAST and CT results and correlated with intraoperative findings. Results A total of 115 patients with penetrating abdominal trauma (87.8% men) were analyzed. In 69 patients, the injuries were caused by interpersonal violence and included 88 stab and 4 firearm wounds. 8 patients (6.9%) were in a state of shock at presentation. 52 patients (44.8%) suffered additional extraabdominal injuries. 38 patients were managed non-operatively, while almost two-thirds of all patients underwent surgical treatment. Hereof, 20 laparoscopies and 3 laparotomies were non- therapeutic. There were two missed injuries, but no patient experienced morbidity or mortality related to delay in treatment. -

Orthopedic Trauma Postoperative Care and Rehab
Orthopedic Trauma Postoperative Care and Rehab Serge Charles Kaska, MD Name that Beach 100$ Still 100$ 75$ 50$ 1$ Omaha • June 6th 1941 • !st Infantry Division • 2000 KIA LIFE OR LIMB THREAT 1. Compartment Syndrome 2. Fat Emboli Syndrome 3. Pulmonary Embolism 4. Shock Compartment syndrome case A 16 year old male was retrieving a tire from his truck bed on the side of the highway in the pouring rain when a car careens off of the road and sandwiches the patients legs between the bumpers at freeway speed. Acute compartment syndrome Compartment syndrome DEFINED Definition: Elevated tissue pressure within a closed fascial space • Pathogenesis – Too much in-flow: results in edema or hemorrhage – Decreased outflow: results in venous obstruction caused by tight dressing and/or cast. • Reduces tissue perfusion • Results in cell death Compartment syndrome tissue survival • Muscle – 3-4 hours: reversible changes – 6 hours: variable damage – 8 hours: irreversible changes • Nerve – 2 hours: looses nerve conduction – 4 hours: neuropraxia – 8 hours: irreversible changes Physical exam 1. Pain 2. Pain 3. Pain Physical exam • Inspection – Swelling, skin is tight and shiny • Motion – Active motion will be refused or unable. Must see dorsiflexion • Palpation – Severe pain with palpation • Alarming pain with passive stretch Physical exam • Dorsiflexion Physical Exam • Palpation – Severe pain with palpation • Alarming pain with passive stretch Physical exam • Evaluations from nurses, therapists, and orthotech’s are CRITICAL • If you call a doctor and say that -
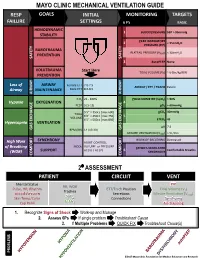
Mechanical Ventilation Guide
MAYO CLINIC MECHANICAL VENTILATION GUIDE RESP GOALS INITIAL MONITORING TARGETS FAILURE SETTINGS 6 P’s BASIC HEMODYNAMIC 1 BLOOD PRESSURE SBP > 90mmHg STABILITY PEAK INSPIRATORY 2 < 35cmH O PRESSURE (PIP) 2 BAROTRAUMA PLATEAU PRESSURE (P ) < 30cmH O PREVENTION PLAT 2 SAFETY SAFETY 3 AutoPEEP None VOLUTRAUMA Start Here TIDAL VOLUME (V ) ~ 6-8cc/kg IBW PREVENTION T Loss of AIRWAY Female ETT 7.0-7.5 AIRWAY / ETT / TRACH Patent Airway MAINTENANCE Male ETT 8.0-8.5 AIRWAY AIRWAY FiO2 21 - 100% PULSE OXIMETRY (SpO2) > 90% Hypoxia OXYGENATION 4 PEEP 5 [5-15] pO2 > 60mmHg 5’5” = 350cc [max 600] pCO2 40mmHg TIDAL 6’0” = 450cc [max 750] 5 VOLUME 6’5” = 500cc [max 850] ETCO2 45 Hypercapnia VENTILATION pH 7.4 GAS GAS EXCHANGE BPM (RR) 14 [10-30] GAS EXCHANGE MINUTE VENTILATION (VMIN) > 5L/min SYNCHRONY WORK OF BREATHING Decreased High Work ASSIST CONTROL MODE VOLUME or PRESSURE of Breathing PATIENT-VENTILATOR AC (V) / AC (P) 6 Comfortable Breaths (WOB) SUPPORT SYNCHRONY COMFORT COMFORT 2⁰ ASSESSMENT PATIENT CIRCUIT VENT Mental Status PIP RR, WOB Pulse, HR, Rhythm ETT/Trach Position Tidal Volume (V ) Trachea T Blood Pressure Secretions Minute Ventilation (V ) SpO MIN Skin Temp/Color 2 Connections Synchrony ETCO Cap Refill 2 Air-Trapping 1. Recognize Signs of Shock Work-up and Manage 2. Assess 6Ps If single problem Troubleshoot Cause 3. If Multiple Problems QUICK FIX Troubleshoot Cause(s) PROBLEMS ©2017 Mayo Clinic Foundation for Medical Education and Research CAUSES QUICK FIX MANAGEMENT Bleeding Hemostasis, Transfuse, Treat cause, Temperature control HYPOVOLEMIA Dehydration Fluid Resuscitation (End points = hypoxia, ↑StO2, ↓PVI) 3rd Spacing Treat cause, Beware of hypoxia (3rd spacing in lungs) Pneumothorax Needle D, Chest tube Abdominal Compartment Syndrome FLUID Treat Cause, Paralyze, Surgery (Open Abdomen) OBSTRUCTED BLOOD RETURN Air-Trapping (AutoPEEP) (if not hypoxic) Pop off vent & SEE SEPARATE CHART PEEP Reduce PEEP Cardiac Tamponade Pericardiocentesis, Drain. -

Acute Compartment Syndrome Complicating Deep Venous Thrombosis
SMGr up Case Report SM Journal of Acute Compartment Syndrome Case Reports Complicating Deep Venous Thrombosis Senthil Dhayalan1*, David Jardine1*, Tony Goh2 and Nicholas Lash3 1Senior registrar and General Physician, Dept of General Medicine, NZ 2Consultant Radiologist, Dept of Radiology, NZ 3Orthopaediac Surgeon, Dept of Orthopaedics, NZ A 40-yr old, heavily-built man initially presented to his general practitioner 2 days before Article Information admission with recent onset of pain and swelling in his left calf. A duplex ultrasound scan Received date: Nov 21, 2018 demonstrated a popliteal and lower leg deep vein thrombosis [DVT], extending 15 cm above the Accepted date: Nov 26, 2018 knee into the femoral vein. He was started appropriately on enoxaparin 130 mg bd. Despite the Published date: Nov 27, 2018 treatment, the pain got worse, particularly when standing, and he was admitted for symptom control. Five weeks earlier he had undergone anterior cruciate ligament repair of the left knee, *Corresponding author [without heparin prophylaxis] and made a satisfactory recovery (Figure 1). Jardine D, General Medicine On examination he was mildly distressed with a low-normal blood pressure [110/70 mmHg] Department, Christchurch hospital, and a persistent low-grade fever [temperature ranged from 37.0-37.8 oC]. The left leg was moderately Private Bag 4710, Christchurch 8140, diffusely swollen, slightly warm and darker in colour [figure]. The pain was localised to the posterior New Zealand, compartments and was exacerbated by dorsi-flexing the ankle and squeezing the gastrocnemius. Email: [email protected] There were no signs of joint effusion, thrombophlebitis, lymphadenopathy or cellulitis. -

Deaths from Abdominal Trauma: Analysis of 1888 Forensic Autopsies
DOI: 10.1590/0100-69912017006006 Original Article Deaths from abdominal trauma: analysis of 1888 forensic autopsies Óbitos por trauma abdominal: análise de 1888 autopsias médico-legais POLYANNA HELENA COELHO BORDONI1; DANIELA MAGALHÃES MOREIRA DOS SANTOS2; JAÍSA SANTANA TEIXEIRA2; LEONARDO SANTOS BORDONI2-4. ABSTRACT Objective: to evaluate the epidemiological profile of deaths due to abdominal trauma at the Forensic Medicine Institute of Belo Horizonte, MG - Brazil. Methods: we conducted a retrospective study of the reports of deaths due to abdominal trauma autopsied from 2006 to 2011. Results: we analyzed 1.888 necropsy reports related to abdominal trauma. Penetrating trauma was more common than blunt one and gun- shot wounds were more prevalent than stab wounds. Most of the individuals were male, brown-skinned, single and occupationally active. The median age was 34 years. The abdominal organs most injured in the penetrating trauma were the liver and the intestines, and in blunt trauma, the liver and the spleen. Homicide was the most prevalent circumstance of death, followed by traffic accidents, and almost half of the cases were referred to the Forensic Medicine Institute by a health unit. The blood alcohol test was positive in a third of the necropsies where it was performed. Cocaine and marijuana were the most commonly found substances in toxicology studies. Conclusion: in this sam- ple. there was a predominance of penetrating abdominal trauma in young, brown and single men, the liver being the most injured organ. Keywords: Autopsy. Forensic Medicine. Homicide. Abdominal Injuries. INTRODUCTION In addition, the accuracy of abdominal phy- sical examination is low and the level of consciousness eaths from external causes represent the second produced by hemorrhages or by the association of ab- Dleading cause of mortality in Brazil and the main dominal trauma (AT) with traumatic brain injury and/or cause when considering individuals under the age of effects of central nervous system of previously consu- 351. -

Bilateral Atraumatic Compartment Syndrome of the Legs Leading to Rhabdomyolysis and Acute Renal Failure Following Prolonged Kneeling in a Heroin Addict
PAJT 10.5005/jp-journals-10030-1075 CASE REPORTBilateral Atraumatic Compartment Syndrome of the Legs Leading to Rhabdomyolysis and Acute Renal Failure Bilateral Atraumatic Compartment Syndrome of the Legs Leading to Rhabdomyolysis and Acute Renal Failure Following Prolonged Kneeling in a Heroin Addict. A Case Report and Review of Relevant Literature Saptarshi Biswas, Ramya S Rao, April Duckworth, Ravi Kothuru, Lucio Flores, Sunil Abrol ABSTRACT cerrado, que interfiere con la circulación de los componentes mioneurales del compartimento. Síndrome compartimental Introduction: Compartment syndrome is defined as a symptom bilateral de las piernas es una presentación raro que requiere complex caused by increased pressure of tissue fluid in a closed una intervención quirúrgica urgente. En un reporte reciente osseofascial compartment which interferes with circulation (Khan et al 2012), ha habido reportados solo 8 casos de to the myoneural components of the compartment. Bilateral síndrome compartimental bilateral. compartment syndrome of the legs is a rare presentation Se sabe que el abuso de heroína puede causar el síndrome requiring emergent surgical intervention. In a recent case report compartimental y rabdomiólisis traumática y atraumática. El (Khan et al 2012) there have been only eight reported cases hipotiroidismo también puede presentarse independiente con cited with bilateral compartment syndrome. rabdomiólisis. Heroin abuse is known to cause compartment syndrome, traumatic and atraumatic rhabdomyolysis. Hypothyroidism can Presentación del caso: Presentamos un caso de una mujer also independently present with rhabdomyolysis. de 22 años quien presentó con tumefacción bilateral de las piernas asociado con la perdida de la sensación, después Case presentation: We present a case of a 22 years old female de pasar dos días arrodillado contra una pared después de who presented with bilateral swelling of the legs with associated usar heroína intravenosa. -
Assessment, Management and Decision Making in the Treatment of Polytrauma Patients with Head Injuries
Compartment Syndrome Andrew H. Schmidt, M.D. Professor, Dept. of Orthopedic Surgery, Univ. of Minnesota Chief, Department of Orthopaedic Surgery Hennepin County Medical Center April 2016 Disclosure Information Andrew H. Schmidt, M.D. Conflicts of Commitment/ Effort Board of Directors: OTA Critical Issues Committee: AOA Editorial Board: J Knee Surgery, J Orthopaedic Trauma Medical Director, Director Clinical Research: Hennepin County Med Ctr. Disclosure of Financial Relationships Royalties: Thieme, Inc.; Smith & Nephew, Inc. Consultant: Medtronic, Inc.; DGIMed; Acumed; St. Jude Medical (spouse) Stock: Conventus Orthopaedics; Twin Star Medical; Twin Star ECS; Epien; International Spine & Orthopedic Institute, Epix Disclosure of Off-Label and/or investigative Uses I will not discuss off label use and/or investigational use in my presentation. Objectives • Review Pathophysiology of Acute Compartment Syndrome • Review Current Diagnosis and Treatment – Risk Factors – Clinical Findings – Discuss role and technique of compartment pressure monitoring. Pathophysiology of Compartment Syndrome Pressure Inflexible Fascia Injured Muscle Vascular Consequences of Elevated Intracompartment Pressure: A-V Gradient Theory Pa (High) Pv (Low) artery arteriole capillary venule vein Local Blood Pa - Pv Flow = R Matsen, 1980 Increased interstitial pressure Pa (High) Tissue ischemia artery arteriole capillary venule vein Lysis of cell walls Release of osmotically active cellular contents into interstitial fluid Increased interstitial pressure More cellular -

Western Trauma Association Critical Decisions in Trauma: Penetrating Chest Trauma
WTA 2014 ALGORITHM Western Trauma Association Critical Decisions in Trauma: Penetrating chest trauma Riyad Karmy-Jones, MD, Nicholas Namias, MD, Raul Coimbra, MD, Ernest E. Moore, MD, 09/30/2020 on BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3Ypodx1mzGi19a2VIGqBjfv9YfiJtaGCC1/kUAcqLCxGtGta0WPrKjA== by http://journals.lww.com/jtrauma from Downloaded Martin Schreiber, MD, Robert McIntyre, Jr., MD, Martin Croce, MD, David H. Livingston, MD, Jason L. Sperry, MD, Ajai K. Malhotra, MD, and Walter L. Biffl, MD, Portland, Oregon Downloaded from http://journals.lww.com/jtrauma his is a recommended algorithm of the Western Trauma Historical Perspective TAssociation for the acute management of penetrating chest The precise incidence of penetrating chest injury, varies injury. Because of the paucity of recent prospective randomized depending on the urban environment and the nature of the trials on the evaluation and management of penetrating chest review. Overall, penetrating chest injuries account for 1% to injury, the current algorithms and recommendations are based 13% of trauma admissions, and acute exploration is required in by on available published cohort, observational and retrospective BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3Ypodx1mzGi19a2VIGqBjfv9YfiJtaGCC1/kUAcqLCxGtGta0WPrKjA== 5% to 15% of cases; exploration is required in 15% to 30% of studies, and the expert opinion of the Western Trauma Asso- patients who are unstable or in whom active hemorrhage is ciation members. The two algorithms should be reviewed in the suspected. Among patients managed by tube thoracostomy following sequence: Figure 1 for the management and damage- alone, complications including retained hemothorax, empy- control strategies in the unstable patient and Figure 2 for the ema, persistent air leak, and/or occult diaphragmatic injuries management and definitive repair strategies in the stable patient. -

ABC Ofmajor' Trauma ABDOMINAL TRAUMA BMJ: First Published As 10.1136/Bmj.301.6744.172 on 21 July 1990
ABC ofMajor' Trauma ABDOMINAL TRAUMA BMJ: first published as 10.1136/bmj.301.6744.172 on 21 July 1990. Downloaded from Andrew Cope, William Stebbings The aim ofthis article is to enable all those concerned with the management of patients with abdominal trauma to perform a thorough examination and assessment with the help of diagnostic tests and to institute safe and correct treatment. Intra-abdominal injuries carry a high morbidity and mortality because they are often not detected or their severity is underestimated. This is particularly common in cases of blunt trauma, in which there may be few or no external signs. Always have a high index ofsuspicion ofabdominal injury when the history suggests severe trauma. Traditionally, abdominal trauma is classified as either blunt or penetrating, but the initial assessment and, if required, resuscitation are essentially the same. Blunt trauma Road traffic accidents are one of the commonest causes of blunt injuries. Since wearing seat belts was made compulsory the number of fatal head injuries has declined, but a pattern of blunt abdominal trauma that is specific to seat belts has emerged. This often includes avulsion injuries of the mesentery of the small bowel. The symptoms and signs of blunt abdominal trauma can be subtle, and consequently diagnosis is difficult. A high degree of suspicion of underlying intra-abdominal injury must be adopted when dealing with blunt trauma. Blunt abdominal trauma is -usually associated with trauma to other areas, especially the head, chest, http://www.bmj.com/ .. , :and pelvis. Penetrating trauma Penetrating wounds are either due to low velocity projectiles such as on 1 October 2021 by guest.