Fire Fighter FACE Report No. F2005-16, Captain Suffers an Acute Aortic Dissection After Responding to Two Alarms and Subsequentl
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chapter Xi the Circulatory System and Blood
CHAPTER XI THE CIRCULATORY SYSTEM AND BLOOD Page General characterlstlcs______ __ __ _ __ __ __ __ __ __ _ 239 of these organs are independent of the beating of The pericardium ___ __ __ __ 239 the principal heart, and their primary function is The heart. _____ __ __ 240 Physiology of the heart.______________________________________________ 242 to oscillate the blood within the pallial sinuses. Automatism of heart beat. _ 242 The pacemaker system_ 245 THE PERICARDIUM Methods of study of heart beat_____________________________________ 247 Frequency of beat___ __ __ _ 248 Extracardlac regulatlon____ __ __ _ 250 The heart is located in the pericardium, a thin Effects of mineral salts and drugs___________________________________ 251 Blood vessels_ __ ___ _ 253 walled chamber between the visceral mass and the The arterial system______ __ __ ___ __ __ __ __ __ 253 adductor muscle (fig. 71). In a live oyster the The venous system_________________________________________________ 254 location of the heart is indicated by the throbbing The accessory heart._____________ 258 The blood______ __ __ __ __ __ __ __ 259 of the wall of the pericardium on the left side. Color of blood_ __ __ 261 Here the pericardium wall lies directly under the The hyaline cells___________________________________________________ 261 The granular cells .______________________________________ 262 shell. On the right side the promyal chamber Specific gravity of blood____________________________________________ 265 extends down over the heart region and the mantle Serology ___ __________ __________________ ____ __ ______________________ 265 Bibliography __ __ __ __ __ __ __ 266 separates the pericardium wall from the shell. The cavity in which the heart is lodged is slightly A heart, arteries, veins, and open sinuses form asymmetrical; on the right side it extends farther the circulatory system of oysters and other bi along the anterior part of the adductor muscle valves. -

Prolonged Asystole During Hypobaric Chamber Training
Olgu Sunumları Anadolu Kardiyol Derg 520 Case Reports 2012; 12: 517-24 contraction/ventricular tachycardia’s originating from mitral annulus contractions arising from the mitral annulus: a case with a pure annular are rarely reported (1). origin. Pacing Clin Electrophysiol 2009; 32: 680-2. [CrossRef] PVCs arising from the mitral annulus frequently originate from 5. Kimber SK, Downar E, Harris L, Langer G, Mickleborough LL, Masse S, et al. anterolateral, posteroseptal and posterior sites (2). It has been reported Mechanisms of spontaneous shift of surface electrocardiographic configuration that 2/3 of the PVCs arising from the mitral annulus originate from during ventricular tachycardia. J Am Coll Cardiol 1992; 15: 1397-404. [CrossRef] anterolateral site (2). Furthermore, small part of these arrhythmias origi- Address for Correspondence/Yaz›şma Adresi: Dr. Ömer Uz nates from the anteroseptal site of the mitral annulus. Ablation of this Gülhane Askeri Tıp Akademisi Haydarpasa, Kardiyoloji Kliniği, İstanbul-Türkiye site may be technically very challenging. Cases have been reported that Phone: +90 216 542 34 65 Fax: +90 216 348 78 80 successful catheter ablation of the premature ventricular contraction E-mail: [email protected] origin from the anteroseptal site of the mitral annulus can be performed Available Online Date/Çevrimiçi Yayın Tarihi: 22.06.2012 either by a transseptal or transaortic approach in literature (3, 4). ©Telif Hakk› 2012 AVES Yay›nc›l›k Ltd. Şti. - Makale metnine www.anakarder.com web Anterolateral site of the mitral annulus is in close proximity to anterior sayfas›ndan ulaş›labilir. of the right ventricle outflow tract, left ventricular epicardium near to ©Copyright 2012 by AVES Yay›nc›l›k Ltd. -

Ventricular Rhythms Originate Below the Branching Portion of The
Northwest Community Healthcare Paramedic Program VENTRICULAR DYSRHYTHMIAS Pacemakers Connie J. Mattera, M.S., R.N., EMT-P Reading assignments: Bledsoe Vol 3; pp. 96-109 SOPs: VT with pulse; Ventricular fibrillation/PVT; Asystole/PEA Drugs: Amiodarone, magnesium, epinephrine 1mg/10mL Procedure manual: Defibrillation; Mechanical Circulatory Support (MCS) using a Ventricular Assist Device KNOWLEDGE OBJECTIVES: Upon completion of the reading assignments, class and homework questions, reviewing the SOPs, and working with their small group, each participant will independently do the following with at least an 80% degree of accuracy and no critical errors: 1. Identify the intrinsic rates, morphology, conduction pathways, and common ECG features of ventricular beats/rhythms. 2. Identify on a 6-second strip the following: a) Idioventricular rhythm b) Accelerated idioventricular rhythm c) Ventricular tachycardia: monomorphic & polymorphic d) Ventricular escape beats e) Premature Ventricular Contractions (PVCs) f) Ventricular fibrillation g) Asystole h) Paced rhythms i) Intraventricular conduction defects (Bundle branch blocks) 3. Systematically evaluate each complex/rhythm for the following: a) Rate (atrial and ventricular) b) Rhythm: Regular/irregular - R-R Interval, P-P Interval c) Presence/absence/morphology of P waves d) Presence/absence/morphology of QRS complexes d) P-QRS relationships f) QRS duration 4. Correlate the cardiac rhythm with patient assessment findings to determine the emergency treatment for each rhythm according to NWC EMSS SOPs. 5. Discuss the action, prehospital indications, side effects, dose and contraindications of the following during VT a) Amiodarone b) Magnesium 6. Describe the indications, equipment needed, critical steps, and patient monitoring parameters for cardioversion and defibrillation. 7. Identify the management of a patient with an implanted defibrillator and/or pacemaker. -
The Aorta Simulating Pulmonary Embolism D
Thorax: first published as 10.1136/thx.29.1.142 on 1 January 1974. Downloaded from Thorax (1974), 29, 142. Pulmonary artery compression by haemorrhage from the aorta simulating pulmonary embolism D. H. FRANKLIN and J. JACQUES The University Department of Medicine, The Royal Infirmary, Edinburgh and the Department of Pathology, Edinburgh University Franklin, D. H., and Jacques, J. (1974). Thorax, 29, 142-144. Pulmonary artery compression by haemorrhage from the aorta simulating pulmonary embolism. A case is presented in which pulmonary embolism was simulated by compression of the pulmonary artery by haematoma during an episode of acute bacterial endocarditis occurring 18 months after aortic valve replacement. CASE REPORT replacement with a fascia lata prosthesis. After his operation he remained very well, but three months A 38-year-old male clerk was admitted to hospital before the present admission he had toothache for suffering from bacterial efndocarditis. Seven years pre- which he did not seek advice. viomly he had been treated for a similar episode due On admission he complained of fever, shivering, and to Streptococcus viridans. Over the ensuing five years stiffness in the back and joints. He was noted to have he had developed progressive aortic incompetence a pale, muddy complexion and petechial haemorrhages which ultimately required treatment by aortic valve in the conjunctivae and optic fundi. A systolic murmur http://thorax.bmj.com/ on October 2, 2021 by guest. Protected copyright. FIG. 1. Chesvt radiograph showing prominence of the left pulmonary artery. 142 Thorax: first published as 10.1136/thx.29.1.142 on 1 January 1974. -

The Unsuspected Complications of Bacterial Endocarditis Imaged by Gallium-67 Scanning
The Unsuspected Complications of Bacterial Endocarditis Imaged by Gallium-67 Scanning Shobha P. Desai and David L. Yuille Nuclear Medicine Department, St. Luke's Medical Center, Milwaukee, @V&sconsin tivity in the region of the aortic valve which extended into the In this case report, we present a patient with bacterial endocar right atrium (Fig. 1)but was better appreciated on an axial SPECF ditiswho was evaluatedby 67(@imagingfor persistentfever image (Fig. 2). despitetreatmentwith multipleintravenousantibiotics.Afthough cardiac catheterizationconfirmeda densely calcified bicuspid evidence of bactenal endocarditiswas absent wfth @“Gaimag aorticvalve with both stenosis and insufficiencyas well as what ing,the studydemonstratedfindingsthat representcomplica was thoughtto be aveiy largerightsinus ofvalsalva aneurysm.At tions of bacterial endocarditis. The procedure demonstrated surgery, there was evidence of epicarditisand pericarditisand a moderatepencardialuptakeof isotopeandthus pro@4dedthe hugerightsinus of valsalva abscess was foundwhich was eroding first evidence of pehcardi@swhich was later confirmed at sur into the aortic wall. The aortic valve annuluswas debrided, the gery.The studyalsodemonstratedmi@ increasedactivityin abscess cavity was drainedandthe patient's diseased aorticvalve thevicinityoftheaorticrootandnghtattium.A sinusofvalsalva was replacedwith a no. 25 St. Jude's prosthesis (St. JudeMedical abscess, complicatingthe underlyingdiagnosis of bacterialen Inc., St. Paul, MN). The immediatepostoperativeperiodwas docarc@bs,was -

Premature Obliteration of the Foramen Ovale by G
PREMATURE OBLITERATION OF THE FORAMEN OVALE BY G. AUSTIN GRESHAM From the Department of Pathology, University of Cambridge Received August 16, 1955 Obliteration of the foramen ovale occurring during intrauterine life is a rare condition. It throws some light on the mechanism of development of endocardial fibroelastosis and also upon the factors concerned in determining the size of the aorta and of the cardiac chambers. CASE HISTORY The patient was the second child of a mother (aet. 21) whose previous obstetric history was normal. Apart from two periods of rather rapid gain of weight for which no cause could be found, the pregnancy was uneventful. The child was eleven days postmature; labour was induced with an enema and lasted forty-five minutes. The infant cried lustily but was cyanosed: the heart was clinically normal. Abnormalities were present in all four limbs. The left radius and ulna were absent and rudimentary digits were present on the skin over the distal end of the limb. Terminal phalanges were absent in the fingers of the right hand, and four toes were present on each foot with a rudimentary fifth digit on the left foot. Cyanosis and dyspniea became more intense and the child died three hours after birth despite the use of oxygen. NECROPSY The body was that of a full-term male infant (weight 3430 g.). The limbs were abnormal as previously described. The lips were blue-black in colour. On the septal wall of the right atrium a hemispherical grey-white area (10x 12 x 4 mm. deep) with a central dimple filled in the usual site of the fossa ovalis (Fig. -

The Cardiovascular System
11 The Cardiovascular System WHAT The cardiovascular system delivers oxygen and HOW nutrients to the body tissues The heart pumps and carries away wastes blood throughout the body such as carbon dioxide in blood vessels. Blood flow via blood. requires both the pumping action of the heart and changes in blood pressure. WHY If the cardiovascular system cannot perform its functions, wastes build up in tissues. INSTRUCTORS Body organs fail to function properly, New Building Vocabulary and then, once oxygen becomes Coaching Activities for this depleted, they will die. chapter are assignable in hen most people hear the term cardio- only with the interstitial fluid in their immediate Wvascular system, they immediately think vicinity. Thus, some means of changing and of the heart. We have all felt our own “refreshing” these fluids is necessary to renew the heart “pound” from time to time when we are ner- nutrients and prevent pollution caused by vous. The crucial importance of the heart has been the buildup of wastes. Like a bustling factory, the recognized for ages. However, the cardiovascular body must have a transportation system to carry system is much more than just the heart, and its various “cargoes” back and forth. Instead of from a scientific and medical standpoint, it is roads, railway tracks, and subways, the body’s important to understand why this system is so vital delivery routes are its hollow blood vessels. to life. Most simply stated, the major function of the Night and day, minute after minute, our tril- cardiovascular system is transportation. Using lions of cells take up nutrients and excrete wastes. -

The Surgical Treatment of Constrictive Fibrous Endocarditis
The Surgical Treatment of Constrictive Fibrous Endocarditis CH. DUBOST, P. MAURICE, A. GERBAUX, E. BERTRAND, R. RULLIERE, F. VIAL, A. BARRILLON, C. PRIGENT, A. CARPENTIER, R. SOYER Constrictive fibrous endocarditis is a pathological entity described From the Department of Cardiovascular Surgery, by Lo6ffler in 1936. Its etiology is unknown. The clinical course Broussais Hospital, Paris, France is characterized by an evolution towards cardiac insufficiency leading rapidly to a fatal outcome. Modern paraclinical investi- gations are necessary to assess the diagnostic. Cardiac catheteriza- tion brings the proof of adiastole and angiocardiography re- Endocardiectomy was first performed by us in 19715-7 veals the shape of amputation of the ventricle with auriculo- and the patient was improved. Since then, four more cases ventricular regurgitation. The operative procedure consists of have been done, either right or left sided or combined resection of the ventricular fibrosis including the valves and endocardiectomy and there is no doubt that a better auriculo-ventricular valve replacement 'by ;a prosthetic valve. The disease affects both Caucasians and Negros. Our experience knowledge of the clinical aspects of the disease will includes 5 cases. The indications for operation and their results increase the number of cases referred for treatment. are discussed. Pathology C ONSTRICTIVE FIBROUS ENDOCARDITIS, first described The development of fibrous endocarditis is similar in by Loeffler6 in 1936, consists of endocardial fibrosis all cases: it involves the filling chambers of one or several millimeters in thickness which is potentially both ventricles including the papillary muscles and constrictive and limited to the ventricular cavities. chordae tendinae of the mitral and tricuspid valves The clinical course is characterized by an evolution which themselves are included in the process in the towards cardiac insufficiency which may be predomi- majority of cases.8 nantly right or left sided leading rapidly to a fatal outcome. -

Development of the Endocardium
Pediatr Cardiol DOI 10.1007/s00246-010-9642-8 RILEY SYMPOSIUM Development of the Endocardium Ian S. Harris • Brian L. Black Received: 7 January 2010 / Accepted: 17 January 2010 Ó The Author(s) 2010. This article is published with open access at Springerlink.com Abstract The endocardium, the endothelial lining of the cardiac crescent. We propose a third model that reconciles heart, plays complex and critical roles in heart develop- these two views and suggest future experiments that might ment, particularly in the formation of the cardiac valves resolve this question. and septa, the division of the truncus arteriosus into the aortic and pulmonary trunks, the development of Purkinje Keywords Endocardium Á Endothelial Á Heart fibers that form the cardiac conduction system, and the formation of trabecular myocardium. Current data suggest that the endocardium is a regionally specialized endothe- Overview of Cardiogenesis lium that arises through a process of de novo vasculogen- esis from a distinct population of mesodermal cardiogenic The cardiovascular system is the first organ system to form precursors in the cardiac crescent. In this article, we review and function in the vertebrate embryo. The heart forms recent developments in the understanding of the embryonic when regions of bilaterally symmetrical cardiac progenitor origins of the endocardium. Specifically, we summarize cells in the anterior lateral mesoderm fuse at the ventral vasculogenesis and specification of endothelial cells from midline to form a linear tube, which is continuous with the mesodermal precursors, and we review the transcriptional dorsal aorta anteriorly and the cardinal veins posteriorly pathways involved in these processes. We discuss the [5]. -

Structure of the Heart 2121
8941d_c21.qxd 8/13/03 2:19 PM Page 249 mac 106 mac 106:Desktop Folder:211_sks: EXERCISE STRUCTURE OF THE HEART 2121 OBJECTIVES MATERIALS After completing this exercise, you should • human heart model be able to: • human torso or chart showing the pulmonary and • Describe the location and coverings of the heart systemic circulations and the three layers of the heart wall • colored pencils • Identify major features of cardiac muscle tissue on • preserved sheep heart (or other mammal heart) a prepared microscope slide • dissecting instruments, trays, disposable gloves, • Identify the major heart structures on models or 5-inch blade knife charts • compound microscope with cardiac muscle slide • Describe the flow of a drop of blood through the (for demonstration) pulmonary and systemic circulations, listing the vessels, chambers, and valves • Describe the changes that take place in the heart after birth • Identify the selected heart structures on a dissected sheep heart our heart beats without external stimulation and rests A. COVERINGS only between heart beats. The heart is a small double Ypump that simultaneously pumps blood to and from AND LAYERS body cells through the systemic circulation and to and from OF THE HEART the lungs through the pulmonary circulation. The heart is about the size of a fist and lies in the thoracic cavity. The base of the heart is the wide superior portion of the heart from which the great vessels emerge, and the apex of the heart is the inferior end pointing to the left. The heart is tilted at an angle so that its inferior surface lies against the diaphragm with two-thirds of the heart to the left side of the sternum. -

Cardiac Arrhythmias in Survivors of Sudden Cardiac Death Requiring Impella Assist Device Therapy
Journal of Clinical Medicine Article Cardiac Arrhythmias in Survivors of Sudden Cardiac Death Requiring Impella Assist Device Therapy Khaled Q. A. Abdullah 1,2, Jana V. Roedler 1, Juergen vom Dahl 1, Istvan Szendey 1, Dimitrios Dimitroulis 1, Lars Eckardt 3, Albert Topf 4, Bernhard Ohnewein 4, Lorenz Fritsch 4, Fabian Föttinger 4, Mathias C. Brandt 4, Bernhard Wernly 4,5,6 , Lukas J. Motloch 4 and Robert Larbig 2,3,* 1 Department of Cardiology, Hospital Maria Hilf Moenchengladbach, 41063 Moenchengladbach, Germany; [email protected] (K.Q.A.A.); [email protected] (J.V.R.); [email protected] (J.v.D.); [email protected] (I.S.); [email protected] (D.D.) 2 Department of Cardiology, University Hospital Aachen, RWTH University Aachen, 52062 Aachen, Germany 3 Department of Cardiovascular Medicine, Division of Electrophysiology, University of Muenster, 48149 Muenster, Germany; [email protected] 4 Department of Cardiology, Clinic II for Internal Medicine, University Hospital Salzburg, Paracelsus Medical University, 5020 Salzburg, Austria; [email protected] (A.T.); [email protected] (B.O.); [email protected] (L.F.); [email protected] (F.F.); [email protected] (M.C.B.); [email protected] (B.W.); [email protected] (L.J.M.) 5 Department of Anesthesiology, Perioperative Medicine and Intensive Care Medicine, Paracelsus Medical University of Salzburg, 5026 Salzburg, Austria 6 Center for Public Health and Healthcare Research, Paracelsus Medical University of Salzburg, 5026 Salzburg, Austria Citation: Abdullah, K.Q.A.; Roedler, * Correspondence: [email protected]; Tel.: +49-216-1892-4770 J.V.; vom Dahl, J.; Szendey, I.; Dimitroulis, D.; Eckardt, L.; Topf, A.; Abstract: In this retrospective single-center trial, we analyze 109 consecutive patients (female: 27.5%, Ohnewein, B.; Fritsch, L.; Föttinger, F.; median age: 69 years, median left ventricular ejection fraction: 20%) who survived sudden cardiac et al. -
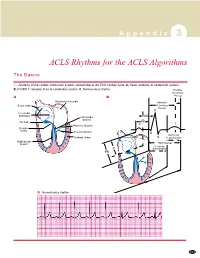
ACLS Rhythms for the ACLS Algorithms
A p p e n d i x 3 ACLS Rhythms for the ACLS Algorithms The Basics 1. Anatomy of the cardiac conduction system: relationship to the ECG cardiac cycle. A, Heart: anatomy of conduction system. B, P-QRS-T complex: lines to conduction system. C, Normal sinus rhythm. Relative Refractory A B Period Bachmann’s bundle Absolute Sinus node Refractory Period R Internodal pathways Left bundle AVN branch AV node PR T Posterior division P Bundle of His Anterior division Q Ventricular Purkinje fibers S Repolarization Right bundle branch QT Interval Ventricular P Depolarization PR C Normal sinus rhythm 253 A p p e n d i x 3 The Cardiac Arrest Rhythms 2. Ventricular Fibrillation/Pulseless Ventricular Tachycardia Pathophysiology ■ Ventricles consist of areas of normal myocardium alternating with areas of ischemic, injured, or infarcted myocardium, leading to chaotic pattern of ventricular depolarization Defining Criteria per ECG ■ Rate/QRS complex: unable to determine; no recognizable P, QRS, or T waves ■ Rhythm: indeterminate; pattern of sharp up (peak) and down (trough) deflections ■ Amplitude: measured from peak-to-trough; often used subjectively to describe VF as fine (peak-to- trough 2 to <5 mm), medium-moderate (5 to <10 mm), coarse (10 to <15 mm), very coarse (>15 mm) Clinical Manifestations ■ Pulse disappears with onset of VF ■ Collapse, unconsciousness ■ Agonal breaths ➔ apnea in <5 min ■ Onset of reversible death Common Etiologies ■ Acute coronary syndromes leading to ischemic areas of myocardium ■ Stable-to-unstable VT, untreated ■ PVCs with